What’s the Difference between Prolotherapy, PRP, and Bone Marrow Concentrate?
While today’s topic may seem very simple, I get this question so often that it’s an important one to review now and again. Prolotherapy, PRP, and Bone Marrow Concentrate collectively make up about 70% of all Regen Med treatments offered in Orthopedic care. Hence, understanding the differences between them is critical. Let’s dive in.
Interventional Orthobiologics
At Regenexx, we are experts in Interventional Orthobiologics. That means that the doctor uses precise image guidance to place various substances specifically in damaged or injured musculoskeletal tissues. The goal is to heal that damage, make it better, or mitigate the degenerative cascade. To learn more about what that looks like, watch my video below:
Prolo vs PRP vs BMC
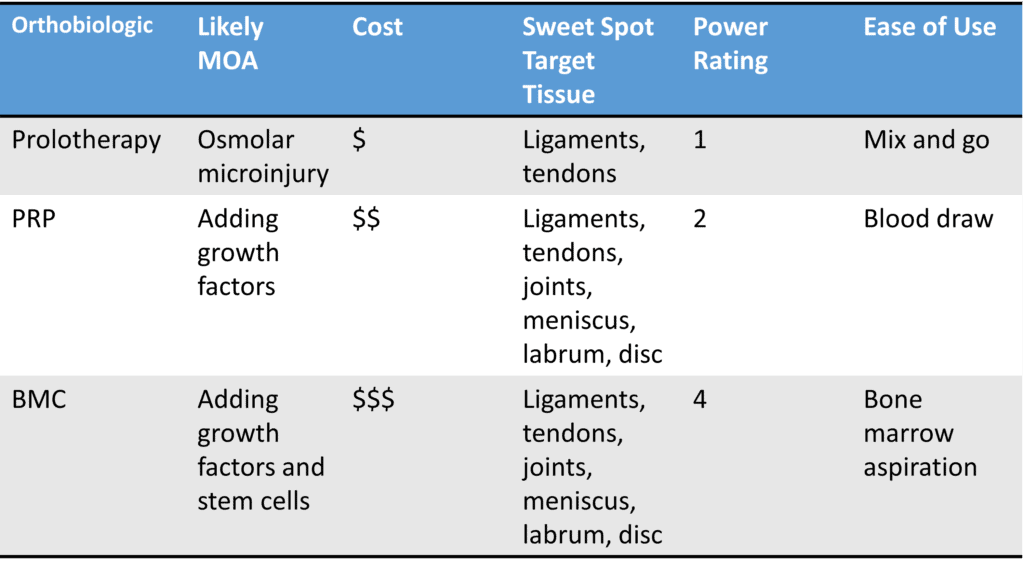
Let’s go through each one of these orthobiologic approaches and compare and contrast:
Prolotherapy
Prolotherapy works by creating another inflammatory healing reaction. When you injure yourself, you get one bite at the healing apple in terms of short-lived healing-type inflammation. If you can’t fully heal, then prolo works by kicking off a second or subsequent healing reaction. While there are many prolo solutions, the most common is Hypertonic Dextrose which is more concentrated than the body’s natural fluids. This causes an osmolar micro-injury and the body reacts to this injury by creating healing inflammation.
The good news I that prolo is cheap. The target tissues where it works best are mild ligament or tendon damage. These injuries would be best described as small partial tears or hypertrophy. On our power rating metric, prolo would be a one, which will make more sense as I go through these power ratings for other technologies. It’s also an easy-to-use technology in that it simply involves mixing various existing FDA-approved substances and then injecting.
PRP
PRP stands for Platelet-Rich Plasma. This is when the doctor takes blood and then concentrates the platelets in plasma. It’s believed to work by adding growth factors (GFs) to the area. GFs act like espresso shots for local repair cells, so they work harder. Other mechanisms by which PRP may work include exosomes secreted by the platelets as well as the platelet providing its good mitochondria to a dying cell in need of help.
The cost for PRP is mid-range, usually about double the cost of prolotherapy. Its sweet spot includes lots of tissues like ligaments, tendons, joints, meniscus, labrum, and spinal discs. Hence it generally has a broader list of indications than prolo. Its power index is two. That means that if a patient would normally need 8 prolo treatments to get the maximum healing effect, in general, it would require about 4 PRP treatments to get the same effect. PRP can also handle bigger partial tears in ligaments or tendons or other structures. For Arthritis, it seems to work best in the mild to moderate severity levels. The ease of use is good as all that’s needed is a blood draw and then either an automated centrifuge or as we do it at Regenexx, a much more flexible and powerful lab in the provider’s office.
BMC
BMC stands for Bone Marrow Concentrate. This is when the doctor takes a bone marrow aspirate and then uses a centrifuge to pull out the stem cell rich fractions, concentrates those, and then injects. It’s believed to also work via growth factors, exosomes, and the donation of mitochondria. However, there’s also the advantage of having mesenchymal stem cells that likely act as construction managers for the repair job. They can also differentiate into the needed cell types for the repair.
BMC is more expensive than PRP and also can be used in ligaments, tendons, joints, meniscus, labrum, and the spinal disc. Its power index is four. That means that if a patient would normally need 8 prolo treatments to get the maximum healing effect and 4 PRP treatments, they need about 2 BMC treatments to get the same effect. In fact, for many patients getting BMC injections, it’s a one-and-done therapy. BMC can handle larger partial or complete non-retracted ligament and tendon tears as well as moderate to severe Arthritis.
What’s NOT Discussed Here
What the provider injects is important, but equally critical is how it’s injected. While there are all sorts of variables in that category, a big one is precise image guidance. Out of 10 providers offering these three orthobiologics above, only 1 is a physician superspecialist who can precisely place this stuff exactly where it needs to go using both ultrasound and x-ray imaging techniques. At Regenexx, we screen and train our providers to be at this level.
The upshot? I hope this blog entry helps you understand the difference between these three commonly used Orthobiologic approaches. Each can be a great help when it’s used in its sweet spot!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
