Hip Labral Tear with Arthritis = Poor Outcomes
The most common hip surgery in America, outside of hip replacement is now hip arthroscopy to treat a labral tear. In one four year period, the number of hip arthroscopy surgeries exploded by 600%! Many of these patients have a hip labral tear with arthritis. However, according to a recent study, many of hip surgeries may be useless in helping to prevent hip replacement.
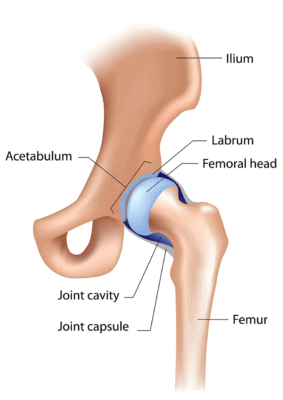
Alila Medical Media/Shutterstock
The hip is a ball and socket joint with a “lip” or labrum around the socket. This labral structure can become torn or frayed, which is often considered an indication for arthroscopy. The torn piece can be either cut out or an attempt at rebuilding the labrum through various means can be accomplished. In addition, bone spurs that form at socket (called pincer deformity) can be taken out surgically or the size of a short socket (hip dysplasia) can be enlarged.
The pressing reason hip arthroscopy is performed is to avoid the need for a hip replacement. However, how much research do we have about this surgery and it’s indications?
-A number of studies question whether hip labrum pain is for real by demonstrating that tears in the labrum are common in patients without pain
-A recent study found that about half of hip surgery patients with a labral tear mounted a successful recovery
-Several recent studies have shown that hip impingement or FAI is very common in patients without any symptoms with almost all people without hip issues in one study having at least one criteria for the diagnosis
The new study looked at a very common occurrence in hip surgery, whether patients with minimal evidence of arthritis at the time of the hip surgery had different outcomes from those patients who had no evidence of arthritis. The new study was also prospective (meaning that it was designed from the start to measure outcome) unlike most of the research on hip arthroscopy which has been retrospective (looking backwards at results). The authors found that even the smallest evidence of arthritis at the time of surgery dramatically reduced outcomes with almost 6 in 10 having worsening arthritis as a result of the surgery. In addition, while the patients with no arthritis fared the best, we have no idea if they would have done just fine if asked to stay off the hip without any surgery. This is a big issue, as countless knee arthroscopy studies have now shown that patients who get a sham surgery do just as well or better than those who get the actual surgery.
The upshot? Many hip arthroscopy patients that we evaluate after failed surgeries had evidence of arthritis before their procedure, so we know it’s still a common practice to operate on patients with that diagnosis. This is despite this and other studies showing that hip arthroscopy isn’t effective in that group of patients. In addition, since we have no placebo controlled trials, I wouldn’t be surprised to find higher level studies in a few years that conclude that most of hip arthroscopy is a boondoggle.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
