How Do Stem Cells Get from Point A to B?
We’ve known for some time that stem cells can migrate to places they need to be as long as they’re placed in the right general area, but how does that work? Now a Stanford team has figured this out. Let’s dig in.
Stem Cells Are Magic?
One of the things that drives me crazy is when a clinic advertises that stem cells are magic. One example of magical thinking is that we can inject stem cells IV and have them just travel to the right spot on their own. The big issue with that is that stem cells need a blood supply to get there and many of the tissues we want to treat have a poor blood supply, which is one of the reasons they can’t heal on their own and need to be treated. In addition, we know that if someone injects stem cells into your veins, 97% of them will be filtered out by your lungs in what’s called a pulmonary first-pass effect. For information on all of this, see my video below:
Getting Stem Cells to the Right Spot?
So if many of the areas that need stem cells don’t have good blood supplies, how do we get them there? That’s through precise imaging guidance to place those cells there. However, this is often not performed by physicians using stem cells. Why? This takes quite a bit of expertise.
Let’s take one of the absolute simplest image-guided injection techniques that can be performed by any doctor, an ultrasound-guided knee joint injection. Here, all the doctor has to do is to place the cells inside the knee joint. Watch my video below to see what I’m talking about:
Now imagine trying to get cells into a tiny joint in the low back that’s 6 inches deep using x-ray guidance. That’s 10 times more complex. Or placing stem cells inside a low back disc or the TFCC in the wrist. All of this stuff requires a high level of training and hundreds of hours of hands-on experience. In addition, fewer than 1 in 100 clinics offering these procedures have providers who have that level of training and experience.
The New Research
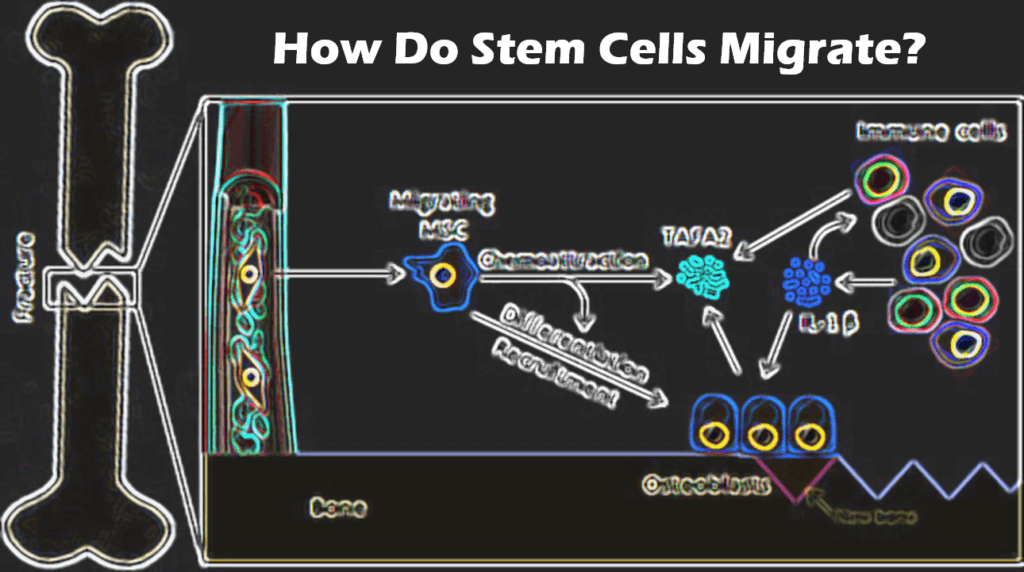
So once the mesenchymal stem cells are placed in the right spot, how do they get to exactly where they need to be? In particular, researchers often find that they have somehow squeezed themselves through tiny holes to get someplace. A Stanford team just spent time answering that question. It turns out that the answer has to do with the nuclear piston.
One of the questions that has long puzzled scientists is how bone marrow mesenchymal stem cells can squeeze themselves through tiny openings that are a hundred to a thousand times smaller than the stem cell? What force could make that happen? Turns out that the cell nucleus is the source of this propellant.
First, the cell places a small part of itself through the tiny opening. Then it moves its nucleus into the small hole to make it bigger. The nucleus also acts like a piston that propels the rest of the cell through the now bigger opening. The nuclear movements are facilitated by both actomyosin and microtubules.
How does this work? Watch my video below:
The upshot? MSCs are crafty little cells. While they often need to be placed exactly where they need to be, they can fine-tune that placement by squeezing through tiny holes by using their nuclear pistons!
_______________________
References:
Hong Pyo L, et al. The nuclear piston activates mechanosensitive ion channels to generate cell migration paths in confined microenvironments. Science Advances. Jan 8, 2021 : EABD4058

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
