More Evidence that ACL Surgeries Cause Knee Problems
Alila Medical Media/Shutterstock
Patients often believe that getting a new part installed is no big deal like bringing a broken car into a mechanic for an upgrade. However, nothing could be further from the truth. Today we’ll focus on the world’s most popular sports medicine surgery — ACL Reconstruction. New research shows clear problems in how the new ACL “ligament” functions.
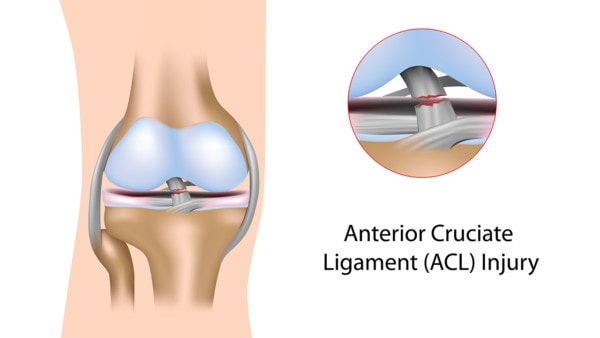
The ACL Ligament
The ACL ligament lives inside the knee and controls stability between the femur and tibia. The ligament can be injured with sports or through wear and tear. When that happens, surgery is often recommended. This procedure, called a surgical ACL reconstruction, removes the damaged ligament and replaces it with a tendon that is drilled into the bones.
The Wiring of the ACL
The wiring of the ACL is just as critical as its stability functions. This is a collection of sensors and nerves that determine the amount of stretch of the ligament which is critical in determining the degree to which the knee muscles should contract to protect the knee. So for example, when you jump and land, the ligament sensors and wiring tell the muscles how best to keep the knee from getting injured.
So what happens when you rip out the damaged ACL? All of these sensors and wiring go away. Meaning the tendon that’s installed to take the place of the ligament is unable to hook itself up to the natural wiring of the knee.
The New Study
18 athletes who had ACL surgery were matched by sex, age, and activity to 18 healthy athletes (1). The goal was to test the wiring of the ACL in the operated knee versus knees that never had surgery. The tests performed included corticospinal excitability, using resting motor threshold (RMT), and motor-evoked potential studies.
What did they find? The knees that had been operated had very poor ability to control the muscles to protect the knee. This was because of the loss of the normal wiring.
Other Issues with ACL Surgeries
There are many other issues with ACL surgery:
- Other studies show that disrupting the normal wiring of the knee impacts normal position sense and performance
- The surgery doesn’t prevent the onset of arthritis
- 2/3rds of teens who get ACL surgery will have arthritis by age 30
- Most ACL surgeries leave the knee unstable
How Can You Prevent this Ligament Wiring Problem?
How can we prevent creating a knee that doesn’t have the ability to protect itself? Don’t rip out the wiring! How can you do that? See if your ACL injury can be treated with a precise injection of your own stem cells, which maintains that wiring by healing the damaged ligament. We developed this new procedure, called Perc-ACLR. This is what that procedure looks like:
If you want to see what this procedure is capable of, check out these before and after MRIs:
The upshot? The ACL ligament in the knee has critical wiring that helps protect your knee. Yank that wiring out and there are problems. Hence, the goal should be to repair the damaged ACL if possible, rather to surgically yank it out.
—
References:
(1) Zarzycki R, Morton SM, Charalambous CC, Pietrosimone B, Williams GN, Snyder-Mackler L. Examination of Corticospinal and Spinal Reflexive Excitability During the Course of Postoperative Rehabilitation After Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther. 2020 Sep;50(9):516-522. doi: 10.2519/jospt.2020.9329. Epub 2020 Aug 1. PMID: 32741329. [Google Scholar]

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
