Should You Get Knee Nerve Ablation?
On this page:
- What is nerve ablation used to treat?
- What does nerve ablation do?
- What are the types of RFA procedures?
- Does knee nerve ablation work?
- How long does it take for a nerve ablation to work?
- How long do the effects of a nerve ablation last?
- Do you need a diagnostic block?
- What imaging techniques are used to place the RFA probe?
- What are the side effects of radiofrequency ablation?
- What are the concerns about cooled RF?
- Are there other treatment options?
Nerve ablation knee treatment has become all the rage these past few years. What is it and who should get it done? Are there risks? Does it work? Are there other options? Let’s dig in.
What Is Nerve Ablation Used to Treat?
The most common use for nerve ablation knee treatment is knee pain caused by moderate to severe arthritis. Generally, these procedures are performed for those patients who are knee replacement candidates, but who don’t want that procedure. They should generally not be used to treat mild arthritis as better options exist for that problem.
What Does Nerve Ablation Do?
Rumruay/Shutterstock
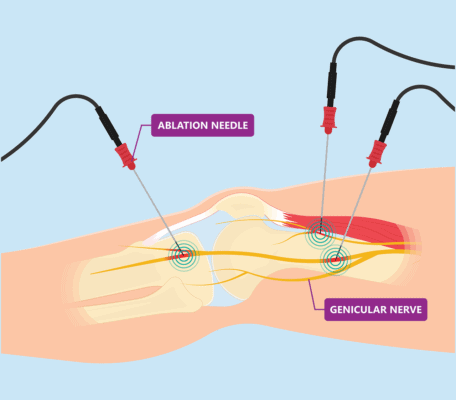
In the knee, there are geniculate nerves that surround the joint and carry pain signals from the area. The idea behind nerve ablation is that nerves carry pain signals, so destroying the nerves carrying those signals should get rid of the pain (1).
What Are the Types of RFA Procedures?
There are two main types of nerve ablation procedures, also called RFA, which stands for radiofrequency ablation. The first is called “cooled RF,” but it has nothing to do with icing the nerve.
In fact, electricity passes through the RF probe (like a thick needle) and this produces quite a bit of heat. The probe has to be cooled to maintain a constant and safe, but high temperature, which in turn “cooks” or destroys the nerve. In the second type of RFA, a pulsed electrical field is generated, which doesn’t completely destroy the nerve (14).
PRF is generally considered safer in that there is less tissue damage, in addition, when cooled RF has been compared to pulsed RF, there was no difference in how the procedure worked across a review of many small studies (10). However, one of the reasons it doesn’t get used as often is the more destructive type of RFA is eligible for insurance reimbursement.
Does Nerve Ablation Work?
The answer is likely yes, although much of the research is made up of small studies (5,10). However, you should be aware that no large, high-level studies exist at this point. Meaning the research on this procedure is still in its infancy.
How Long Does It Take for a Nerve Ablation to Work?
Not long. The effects are generally seen from immediately to several weeks, but on average about 10 days. For Cooled RF, you’re waiting for the nerve to die off and the swelling from the tissue destruction to calm down.
How Long Do the Effects of a Nerve Ablation Last?
The pain-relieving effects generally last about 6 months but could last up to a year. For example, in one study at 3 months, 88% of the patients had good relief, by 6 months that had dropped to 64% and by one year only about 1/3 of the patients still had noticeably less pain (11).
Do You Need a Diagnostic Block?
A diagnostic block is when the doctor numbs the nerves to be treated to see if the procedure will be effective. If you have good short-term pain relief from the numbing injection, then you’re thought to be a good candidate. Is this needed?
One small study showed no improved results when knee arthritis patients had a diagnostic block before the procedure (6). However, a 2017 study reported poor results (only 19% of patients responded), if no diagnostic block was used (9). Hence, on balance, you may want a diagnostic block.
What Imaging Techniques Are Used to Place the RFA Probe?
Your doctor can use either fluoroscopy (realtime x-ray) or ultrasound to guide the placement of the RF probe (2). Fluoroscopy allows him or her to see your bones, but not the nerve. Hence the probe is placed via bone landmarks in the locations where the nerve should likely travel.
Ultrasound does allow the doctor to see the nerve and place the needle across that area. However, in a recent study, despite this advantage, ultrasound-guided procedures didn’t work any better than fluoroscopy-guided RFAs (10).
What Are the Side Effects of Radiofrequency Ablation?
The most common side effect is numbness, tingling, or burning over the skin of the knee, which is due to the destruction of the nerve. Other side effects include infection, damage to the overlying tendons, and skin burns (3,4,7).
However, while rare, damage to the blood vessels can occur as well. The nerve travels with the artery and vein, hence when you ablate the nerve, you can damage either of those blood vessels. These adverse vascular events are documented in the literature with 27 cases being reported to date. Most often, there was a blow out of the artery (pseudoaneurysm), an abnormal connection between the artery and vein (arteriovenous fistula), bleeding into the joint (hemarthrosis), and/or death of the knee cap bone (osteonecrosis of the patella) (13).
What Are the Concerns About Cooled RF?
While “cooled RF” sounds “cool,” as discussed, it’s cooled because the probe can get very hot. At least one expert has chimed in that the high energy used in these procedures means that more tissue damage may occur (8).
Hence, it’s important to note that in one study, there was no difference between a numbing shot with steroid around the nerves versus the actual cooled RFA procedure (12). Meaning a numbing shot without burning the nerve worked as well as killing the nerve.
Are There Other Treatment Options?
As a physician trained to perform many different procedures including RFA, I have never been a fan of killing nerves if it isn’t absolutely necessary. As a result, we more often use orthobiologics than RFA, meaning the injections of substances that can promote healing of, or help the arthritic joint.
For example, platelet-rich plasma or knee stem cell injections are viable options to treat knee arthritis without killing nerves (15-18). However, few of these are covered by insurance.
The upshot? Nerve ablation knee treatment is a new way to help relieve pain. However, please understand that the most commonly used procedure kills the nerve through heat and that complications are possible.
As a result, you may want to consider procedures that can help repair the damaged knee structures rather than kill the nerves. However, if you have severe arthritis and insurance reimbursement is a must, then nerve ablation knee treatment is a procedure to consider.
_______________________________________________
References
(1) Kidd VD, Strum SR, Strum DS, Shah J. Genicular Nerve Radiofrequency Ablation for Painful Knee Arthritis: The Why and the How. JBJS Essent Surg Tech. 2019;9(1):e10. Published 2019 Mar 13. doi:10.2106/JBJS.ST.18.00016
(2) Kim DH, Lee MS, Lee S, Yoon SH, Shin JW, Choi SS. A Prospective Randomized Comparison of the Efficacy of Ultrasound- vs Fluoroscopy-Guided Genicular Nerve Block for Chronic Knee Osteoarthritis. Pain Physician. 2019;22(2):139-146. https://pubmed.ncbi.nlm.nih.gov/30921977/
(3) Conger A, McCormick ZL, Henrie AM. Pes Anserine Tendon Injury Resulting from Cooled Radiofrequency Ablation of the Inferior Medial Genicular Nerve. PM R. 2019;11(11):1244-1247. doi:10.1002/pmrj.12155
(4) Khanna A, Knox N, Sekhri N. Septic Arthritis Following Radiofrequency Ablation of the Genicular Nerves. Pain Med. 2019;20(7):1454-1456. doi:10.1093/pm/pny308
(5) El-Hakeim EH, Elawamy A, Kamel EZ, et al. Fluoroscopic Guided Radiofrequency of Genicular Nerves for Pain Alleviation in Chronic Knee Osteoarthritis: A Single-Blind Randomized Controlled Trial. Pain Physician. 2018;21(2):169-177. https://pubmed.ncbi.nlm.nih.gov/29565947/
(6) McCormick ZL, Reddy R, Korn M, et al. A Prospective Randomized Trial of Prognostic Genicular Nerve Blocks to Determine the Predictive Value for the Outcome of Cooled Radiofrequency Ablation for Chronic Knee Pain Due to Osteoarthritis. Pain Med. 2018;19(8):1628-1638. doi:10.1093/pm/pnx286
(7) McCormick ZL, Walega DR. Third-Degree Skin Burn from Conventional Radiofrequency Ablation of the Inferiomedial Genicular Nerve. Pain Med. 2018;19(5):1095-1097. doi:10.1093/pm/pnx204
(8) Sluijter ME, Teixeira A. Cooled Radiofrequency Ablation of Genicular Nerves for Knee Osteoarthritis Pain: A Letter to Editor. Anesth Pain Med. 2017;7(3):e46940. Published 2017 Apr 8. doi:10.5812/aapm.46940
(9) McCormick ZL, Korn M, Reddy R, Marcolina A, Dayanim D, Mattie R, Cushman D, Bhave M, McCarthy RJ, Khan D, Nagpal G, Walega DR. Cooled Radiofrequency Ablation of the Genicular Nerves for Chronic Pain due to Knee Osteoarthritis: Six-Month Outcomes. Pain Med. 2017 Sep 1;18(9):1631-1641. doi: 10.1093/pm/pnx069
(10) Gupta A, Huettner DP, Dukewich M. Comparative Effectiveness Review of Cooled Versus Pulsed Radiofrequency Ablation for the Treatment of Knee Osteoarthritis: A Systematic Review. Pain Physician. 2017;20(3):155-171. https://pubmed.ncbi.nlm.nih.gov/28339430/
(11) Santana Pineda MM, Vanlinthout LE, Moreno Martín A, van Zundert J, Rodriguez Huertas F, Novalbos Ruiz JP. Analgesic Effect and Functional Improvement Caused by Radiofrequency Treatment of Genicular Nerves in Patients With Advanced Osteoarthritis of the Knee Until 1 Year Following Treatment. Reg Anesth Pain Med. 2017;42(1):62-68. doi:10.1097/AAP.0000000000000510
(12) Qudsi-Sinclair S, Borrás-Rubio E, Abellan-Guillén JF, Padilla Del Rey ML, Ruiz-Merino G. A Comparison of Genicular Nerve Treatment Using Either Radiofrequency or Analgesic Block with Corticosteroid for Pain after a Total Knee Arthroplasty: A Double-Blind, Randomized Clinical Study. Pain Pract. 2017;17(5):578-588. doi:10.1111/papr.12481
(13) Kim SY, Le PU, Kosharskyy B, Kaye AD, Shaparin N, Downie SA. Is Genicular Nerve Radiofrequency Ablation Safe? A Literature Review and Anatomical Study. Pain Physician. 2016;19(5):E697-E705. https://pubmed.ncbi.nlm.nih.gov/27389113/
(14) Facchini G, Spinnato P, Guglielmi G, Albisinni U, Bazzocchi A. A comprehensive review of pulsed radiofrequency in the treatment of pain associated with different spinal conditions. Br J Radiol. 2017;90(1073):20150406. doi:10.1259/bjr.20150406
(15) Xing D, Wang B, Zhang W, et al. Intra-articular platelet-rich plasma injections for knee osteoarthritis: An overview of systematic reviews and risk of bias considerations. Int J Rheum Dis. 2017;20(11):1612-1630. doi:10.1111/1756-185X.13233
(16) Filardo G, Kon E, Buda R, et al. Platelet-rich plasma intra-articular knee injections for the treatment of degenerative cartilage lesions and osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):528-535. doi:10.1007/s00167-010-1238-6
(17) Southworth TM, Naveen NB, Tauro TM, Leong NL, Cole BJ. The Use of Platelet-Rich Plasma in Symptomatic Knee Osteoarthritis. J Knee Surg. 2019;32(1):37-45. doi:10.1055/s-0038-1675170
(18) Centeno C, Sheinkop M, Dodson E, et al. A specific protocol of autologous bone marrow concentrate and platelet products versus exercise therapy for symptomatic knee osteoarthritis: a randomized controlled trial with 2 year follow-up. J Transl Med. 2018;16(1):355. Published 2018 Dec 13. doi:10.1186/s12967-018-1736-8

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
