Understanding Knee Bursitis

Knee bursitis is the inflammation of fluid-filled sacs around the knee, known as bursae. It can occur due to repetitive motions, constant pressure on the knee, or injuries, and cause pain, tenderness, and swelling.
When experiencing these symptoms, proper diagnosis is crucial. Symptoms like pain and inflammation might be signs of deeper issues like tendon damage [1].
Common treatments, such as painkillers or corticosteroid injections, can offer short-term relief. However, they don’t solve the underlying problem and can have severe side effects. If left untreated, these problems may lead to long-term pain and complications, as well as an over-reliance on medications.
The Regenexx approach provides a non-surgical alternative to address the causes of knee pain. Interventional orthobiologics can help promote the body’s natural healing processes without the complications associated with surgery or long-term medication use.
Defining the Anatomy of the Knee
The knee is one of the body’s most complex joints. It connects the thigh bone (femur) to the shinbone (tibia). At the front of the knee is the patella, or kneecap. This is a small, triangular bone that protects the main knee joint.
The bones in the knee joint are connected by strong bands of tissue, ligaments and tendons. Ligaments connect bones and stabilize the knee joint. Tendons attach muscles to bones, facilitating movement.
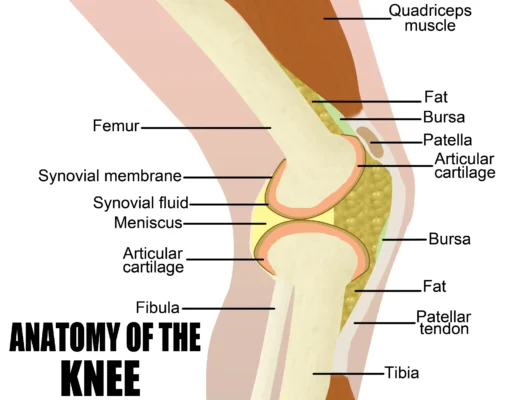
Bursae are small sacs filled with fluid that act as “cushions”. They reduce friction on pressure points between bones and the tendons or muscles near the joints.
Adults have around 160 bursae in the body [2]. They are located around major joints like shoulders, elbows, hips, and knees.
Each knee contains 12 bursae. Five of them play a primary role:
- Prepatellar bursa: Located between the skin and the kneecap.
- Infrapatellar bursae: Located below the kneecap, they cushion the patellar tendon.
- Suprapatellar bursa: Located above the patella, between the thigh muscle and the knee joint.
- Pes anserine bursa: Located on the inner side of the knee, under the hamstring tendon.
- Semimembranosus bursa: Located on the inner side of the knee, near the semimembranosus muscle.
What Is Bursitis of the Knee?
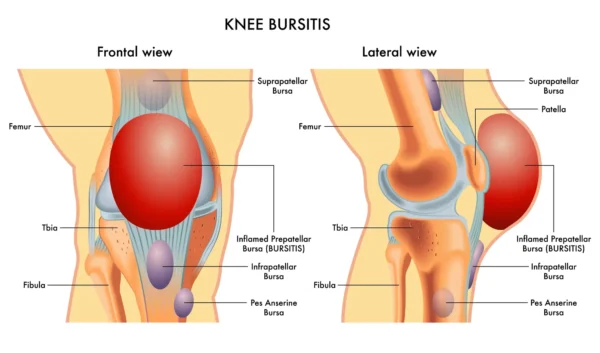
Knee bursitis affects one in every 10,000 people every year [1]. It occurs when one or more of the bursae in the knee become inflamed, damaged, and irritated. Causes include repetitive motion, prolonged pressure on the knee, or complications from an injury or infection.
Swelling is a common symptom of bursitis. It occurs when the body’s inflammatory response sends more fluids to the injured area. Other symptoms include pain, tenderness, and warmth around the knee.
Different Types of Bursitis of the Knee
Common types of knee bursitis include:
- Prepatellar bursitis: This type of bursitis affects the bursa located in front of the kneecap (patella). It is usually known as “coal miner’s knee,” “carpenter’s knee” or “housemaid’s knee.” It results from frequent kneeling on hard surfaces.
- Pes anserine bursitis: This occurs at the bursa situated on the inner side of the knee, just below the joint. This bursa is similar in appearance to a goose’s foot. Pes anserine bursitis is often caused by overuse, obesity, or sports like running. Its symptoms worsen when climbing stairs or due to other weight-bearing activities.
Other types of bursitis are less common. They include:
- Infrapatellar bursitis, affecting the bursa below the kneecap
- Suprapatellar bursitis, affecting the bursa above the kneecap
Identifying the Signs and Symptoms
Knee bursitis symptoms develop over time. They progress from mild discomfort to pain that impacts daily activities. Their location varies depending on which bursae is affected.
Pain and Tenderness
Pain and tenderness are common in the initial stages of bursitis. They occur when the body’s inflammatory response causes the build-up of fluids around the injured area. These fluids compress surrounding tissues and lead to discomfort.
Patients often describe knee bursitis pain as an aching or burning sensation. Discomfort can intensify with movement or pressure on the affected area, like kneeling.
Localized Knee Swelling
Swelling results from the build-up of fluid around the affected bursa. Fluid build-up causes puffiness around the joint. It can also form a soft lump that is visible when comparing the affected knee to a healthy one.
Warmth Around the Knee
An injured or irritated bursa triggers the inflammatory response. Inflammation increases the blood flow to the injured area to deliver oxygen, nutrients, and healing factors. The blood flow increase causes a sensation of warmth in the area, even when the rest of the body feels cool.
Causes of Bursitis of the Knee
The causes of knee bursitis can vary. Around 70% of knee bursitis cases arise from repetitive stress [3], injury, trauma, or mechanical issues.
Repetitive Irritation
Repetitive movements or pressure on the knee can irritate and inflame the bursa. These movements include frequent kneeling, jumping, or running.
These activities can also affect the nerves around the bursae. Impacted nerve endings influence how forces are distributed in the knee joint during activities like running or walking. Over time, this imbalance can cause the bursae to become inflamed.
Injury and Trauma
Direct injury to the knee causes acute inflammation, leading to bursitis. Traumatic events that cause injured bursae include falls and car accidents. The bursae can also become injured when nearby components are damaged, like knee ligaments, tendons, and bones.
Inflammation typically eases down once the underlying injury has healed. However, sometimes it remains active for long periods. This leads to chronic pain, swelling, and mobility issues.
Bacterial Infection
In some cases, the bursae can become infected by bacteria. This condition is called septic bursitis. 80-90% of cases of septic bursitis are caused by the Staphylococcus aureus bacteria [4].
Often, infection results from a cut or wound near the knee that allows bacteria to enter. However, bacterial infections can also be a complication of surgical interventions like knee replacement surgery.
Low Back Issues
Problems with the back’s alignment, like scoliosis or bad posture, can change walking patterns and stress knee tendons. This stress leads to bursitis and knee inflammation.
In particular, having flat feet increases the risk of Pes anserine bursitis [5]. They misalign the limbs, increasing pressure on the knee’s inner side, where this bursa is located.
Additionally, spinal nerves control leg movement and feeling. If they’re squeezed, irritated, or damaged, it can cause referred pain. This pain might appear as knee pain and numbness but actually start in the spine.
Spinal nerves control leg movement and sensation. When these nerves are pinched, they can weaken muscles, leading to extra strain on tendons, especially near the knee. This problem often worsens with a tight iliotibial (IT) band, a tissue that runs along the outer thigh. A tight IT band can pull the knee out of alignment, causing pain. Even though the issue starts in the spine, it shows how nerve problems, muscle weakness, and tendon strain are connected, with the knee being especially affected.
It’s vital to pinpoint the pain’s source for proper treatment. For example, using topical anti-inflammatory drugs on the knee won’t help if the pain comes from a pinched nerve in the back.
Other Underlying Medical Conditions
Diseases like rheumatoid arthritis or gout can cause body-wide inflammation.
Other conditions that may increase the risk of bursitis include diabetes and degenerative diseases. For instance, NIH research notes that pes anserine bursitis affects about a quarter of diabetics, more often women [5]. A 2015 study showed that 20% of 85 knee osteoarthritis patients had pes anserine bursitis [6]. This rate was much higher than in the general population.
Bursitis risk can also be increased by:
- Conditions like syphilis and tuberculosis, which cause mild, widespread inflammation.
- Factors that weaken the immune system, like chronic steroid use and hemodialysis.
- Autoimmune diseases and gout
Understanding the Vulnerable or At-Risk Groups
Some demographics are more prone to knee bursitis because of risk factors like:
- Aging population: With age, tendons lose elasticity and become more prone to damage. This makes older adults more prone to bursitis. A 2014 study shows that 80% of all patients with knee bursitis are males aged between 40 and 60 [7].
- Athletes: High-impact sports like running, basketball, and football involve repetitive knee stress. This can cause tendon damage and bursitis. One study shows that pes anserine tendo-bursitis, which is the inflammation of both tendons and the bursae, accounts for 2.5% of knee pain cases in athletes [8].
- Manual laborers: Occupations that require frequent kneeling or heavy lifting, such as construction work, can cause repetitive irritation. This leads to a higher rate of bursitis among these workers [9].
- Obese individuals: Excess weight puts additional pressure on the knee joints. This increases friction and the risk of bursae inflammation. A 2021 study found that obese individuals have a higher risk of inflammatory joint conditions [10].
Potential Complications of Untreated Knee Problems
Letting knee bursitis go untreated can lead to complications, including ongoing inflammation and the development of other knee conditions.
Ongoing knee problems can progress into more serious conditions like osteoarthritis, meniscal injuries, and cartilage degeneration. Untreated bursitis may also cause the bursae to tear or rupture. This can severely affect knee mobility.
Bursitis itself doesn’t cause more injury but indicates there’s a problem. Severe knee damage, along with bursitis, may need surgery. However, surgery can bring extra risks like infection and further knee damage.
A focus on the importance of an accurate diagnosis
Prompt treatment of knee bursitis is crucial. However, treatment should not be limited to just taking painkillers to numb the pain. If underlying issues such as tendon damage, osteoarthritis, or spinal misalignments are present, painkillers will not address the root cause of the condition.
Additionally, relying on painkillers can expose patients to side effects and delay an accurate diagnosis by masking the pain. This can lead to undiagnosed and untreated symptoms, resulting in further complications.
Diagnosing Bursitis of the Knee
Physicians employ several diagnostic methods to determine the root cause of pain:
- Clinical examination: This initial physical assessment involves checking for visible signs. These include swelling, tenderness, and reduced range of motion.
- Medical history: A physician may evaluate past injuries or conditions that could be contributing to current symptoms. This helps determine the cause of pain.
- X-rays: These scans can help visualize bone structures. They are also used to rule out fractures or arthritis.
- MRI (magnetic resonance imaging): These tests provide detailed images of soft tissues. These images help identify tendon damage, inflammation, or fluid buildup in the bursae.
- Ultrasound: Ultrasound scans are effective tools for assessing soft tissue swelling and fluid build-up in real-time.
- Aspiration: This process involves extracting fluid from the bursae with a needle. The samples are analyzed in a laboratory to rule out infection. As we’ll see below, this technique also has therapeutic applications beyond diagnostic ones.
- Blood tests: Specific blood tests can help identify systemic conditions like rheumatoid arthritis or infections.
Diagnosing knee bursitis itself can be straightforward because of the characteristic swelling. However, identifying the underlying cause can be more complex. Root problems may include hidden tendon damage, spine misalignments, and conditions like osteoarthritis.
Advanced diagnostic methods and comprehensive evaluations, such as the ones performed as part of the Regenexx approach, are crucial for accurate diagnosis and treatment.
Using the industry-leading SANS evaluation method, physicians in the Regenexx network can examine the body in motion and review existing imaging (MRI and/or X-Ray). They also often use ultrasound to observe the inner workings of the joint in real time. Combined, these evaluation methods allow physicians in the Regenexx network to get a more accurate picture of what is contributing to symptoms, how function has been affected, and ultimately, the root cause of pain.
Conventional Treatment Approaches to Bursitis of the Knee
Painkillers and at-home remedies may offer short-term relief. However, they do not address the underlying causes of inflammation and may carry severe risks. Because of this, treatment should begin with an accurate diagnosis.
At-Home Relief
At-home pain relief often involves the RICE method: rest, ice, compression, and elevation. This method works by reducing pressure on the knee. It also slows down the blood supply to the injured area. This decreases stress on the joint, inflammation, and swelling.
However, a 2021 study shows that icing may hinder the recovery process [11], indicating it may be less effective than previously thought.
Over-the-Counter/Prescribed Medications
Pain medications work in different ways to alleviate discomfort and swelling. Some of the most common include:
- NSAIDs (nonsteroidal anti-inflammatory drugs): Medications like ibuprofen or naproxen reduce inflammation and relieve pain. They work by blocking the production of inflammatory agents known as prostaglandins. They are often used as a first-line defense against acute injuries but don’t not address the underlying cause of inflammation. A 2004 study suggests that long term use of NSAIDs are responsible for 30% of hospital admissions for adverse drug reactions (ADRs) [12], mainly due to bleeding, heart attack, stroke, and renal damage. In addition, a 2011 study suggests that NSAIDs increase the risk of a cardiac event by as much as 82%.
- Corticosteroid injections: Corticosteroids are the manufactured version of cortisol. Cortisol i
- s a hormone naturally produced by the body that helps regulate inflammation. These injections can provide temporary pain relief. However, repeated use can damage cartilage and disrupt normal cortisol production [13].
Septic bursitis, caused by infection, may require prescription medications to prevent further complications. Infection should be treated rapidly with antibiotics. It may also require surgical drainage to remove the infected fluid.
Surgical Interventions
Surgery is rarely necessary for bursitis and is considered only in severe cases. Common surgical options include:
- Aspiration: This involves draining excess fluid from the bursa to reduce swelling and discomfort.
- Bursa removal (bursectomy): In severe cases, the inflamed bursa may be surgically removed.
- Tendon repair: Addressing any underlying tendon damage may help prevent recurrent bursitis.
Surgery does not guarantee a pain-free outcome. Many patients may continue to experience pain. Sometimes, they also require additional interventions. A 2011 study was conducted on 60 patients who received surgery for prepatellar bursitis. Among these, 20% still experienced pain at follow-up, and three patients required repeated aspirations [14].
Why Choose a Non-Surgical Approach for Knee Health Care?
Today, interventional orthobiologics provide viable non-surgical options for treating knee bursitis without the risks and complications associated with surgery. Common options include platelet-rich plasma (PRP), and bone marrow concentrate (BMAC) injections.
However, not all interventional orthobiologics are the same. Regenexx procedures offer customizable cell concentrations. These can be tailored to each patient and their condition or injury needs, ranging from 6X to 20X. The 20X concentration of stem cells contained in bone marrow far exceeds what is generally achievable by non-Regenexx providers.
These alternatives use the body’s natural healing processes at the injury site. In turn, they may reduce the need for surgery.
How Physicians In The Regenexx Network Approach Knee Conditions
Regenexx’s non-surgical procedures leverage the body’s natural healing abilities. This could help patients manage musculoskeletal conditions, including bursitis, tendon damage, and chronic conditions like arthritis.
Physicians in the Regenexx network will customize each treatment plan based on the diagnosis and patient’s needs. They may use one or a combination of the interventional orthobiologic procedures below.
Regenexx-SD
The Regenexx-SD procedure includes a patented protocol that utilizes Bone Marrow Concentrate (BMC) which contains the patient’s own mesenchymal stem cells. The cell processing for a Regenexx-SD procedure routinely achieves 20x concentration of stem cell-containing bone marrow — far above what non-Regenexx providers achieve.
Regenexx-SCP
The Regenexx-SCP procedure pioneered by Regenexx represents a supercharged version of platelet-rich plasma (PRP). In this procedure, blood is drawn, then processed to isolate the platelets and growth factors. The growth factors are then purified, concentrated, and injected into the knee area using imaging guidance for precision. Regenexx-SCP provides a higher concentration of growth factors compared to standard PRP procedures
Regenexx-PL
Regenexx-PL is a highly specialized derivative of platelet-rich plasma (PRP) with a faster and more concentrated release of growth factors compared to traditional PRP. Regenexx’s proprietary platelet-lysate processing technology has evolved through multiple generations. PL is often combined with other treatments like Super Concentrated Platelets (SCP) and bone marrow concentrate.
Prognosis of Knee Bursitis
Mild knee bursitis from frequent kneeling typically resolves within a few weeks. However, the condition may indicate underlying issues such as tendon damage or spinal misalignment, leading to recurring symptoms. Physicians in the Regenexx network can diagnose the root cause of pain and determine if a non-surgical treatment plan is right for the patient.
References
- Rishor-Olney CR, Taqi M, Pozun A. Prepatellar Bursitis. [Updated 2024 Jan 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557508/
- Mercadante JR, Marappa-Ganeshan R. Anatomy, Skin Bursa. [Updated 2022 Oct 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554438/
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Overview: Bursitis. [Updated 2022 May 4]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525773/
- Truong J, Mabrouk A, Ashurst JV. Septic Bursitis. [Updated 2023 Apr 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470331/
- Mohseni M, Mabrouk A, Li DD, et al. Pes Anserine Bursitis. [Updated 2024 Jan 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532941/
- Uysal F, Akbal A, Gökmen F, Adam G, Reşorlu M. Prevalence of pes anserine bursitis in symptomatic osteoarthritis patients: an ultrasonographic prospective study. Clin Rheumatol. 2015;34(3):529-533. doi:10.1007/s10067-014-2653-8
- Baumbach SF, Lobo CM, Badyine I, Mutschler W, Kanz KG. Prepatellar and olecranon bursitis: literature review and development of a treatment algorithm. Arch Orthop Trauma Surg. 2014;134(3):359-370. doi:10.1007/s00402-013-1882-7
- Salati U, Doody O, Munk PL, Torreggiani W. Evaluation of Knee Pain in Athletes: A Radiologist’s Perspective. Can Assoc Radiol J. 2017;68(1):27-40. doi:10.1016/j.carj.2016.04.003.
- Le Manac’h AP, Ha C, Descatha A, Imbernon E, Roquelaure Y. Prevalence of knee bursitis in the workforce. Occup Med (Lond). 2012;62(8):658-660. doi:10.1093/occmed/kqs113
- Kanthawang T, Bodden J, Joseph GB, et al. Obese and overweight individuals have greater knee synovial inflammation and associated structural and cartilage compositional degeneration: data from the osteoarthritis initiative. Skeletal Radiol. 2021;50(1):217-229. doi:10.1007/s00256-020-03550-5
- Wang ZR, Ni GX. Is it time to put traditional cold therapy in rehabilitation of soft-tissue injuries out to pasture?. World J Clin Cases. 2021;9(17):4116-4122. doi:10.12998/wjcc.v9.i17.4116
- Pirmohamed M, James S, Meakin S, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ. 2004;329(7456):15-19. doi:10.1136/bmj.329.7456.15
- Broersen LHA, Pereira AM, Jørgensen JOL, Dekkers OM. Adrenal Insufficiency in Corticosteroids Use: Systematic Review and Meta-Analysis. J Clin Endocrinol Metab. 2015;100(6):2171-2180. doi:10.1210/jc.2015-1218.
- Huang YC, Yeh WL. Endoscopic treatment of prepatellar bursitis. Int Orthop. 2011;35(3):355-358. doi:10.1007/s00264-010-1033-5
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
