When IPM Is Worse than Spine Surgery

Credit: Shutterstock
I’ve blogged a few times on the idea that some Interventional Pain Medicine clinics are becoming as bad as the surgeons they have long criticized. Case in point this morning is an x-ray shared by a radiologist. If a picture is worth 1,000 words, this one is worth 1,001. Let’s dig in.
IPM
IPM=Interventiopnal Pain Management. The idea is that through the use of x-ray or ultrasound-guided injections, devices, or minimally invasive implants, these doctors can help patients in chronic pain. When this specialty began, the promise was that it would help avoid all of the crazy things happening in spine surgery. The cascading Fusions and the “bull in the china shop” effect where one surgery turns into a second to fix the first and then another surgery is done to fix the poor results of the second, etc… And when the field first got a head of steam around the early 2000’s, that was its promise.
However, these past 5 years, some IPM practices have tried to mold themselves in the image of surgical practices, where device companies drive the procedures. Meaning, since a screw made in China for $20 can be sold to an insurer for thousands of dollars, the amount of financial pressure that can be brought to bear to make inserting that screw “standard of care” is immense. There’s just so much money sloshing around the system of sales reps and physician “Key Opinion Leaders” that it’s a foregone conclusion that your screw will be used frequently, even when it shouldn’t be.
The Picture
This morning the picture I want to review was shared by Shane Rose, M.D., a neurointerventional radiologist in Indiana. I have to applaud Shane for having the courage to buck the trend against device companies incenting doctors to implant stuff in patients. That takes a lot of courage these days, as not only are you fighting an uphill battle against an army of sales reps and cash-rich device companies, but you’re also likely to take flak from some of your colleagues as well. This is the x-ray film:
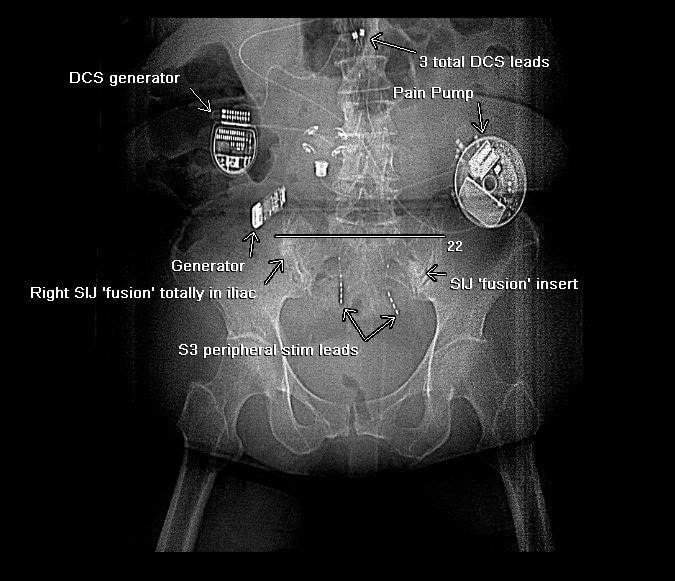
This is a mess. First up are the SI joint fusion screws (SIJ Fusion). This has become all the rage to treat SI joint instability and pain. While this type of problem can be treated easily with a cheap and simple injection of Prolotherapy, PRP, or Bone Marrow Concentrate, many patients never get access to those therapies to help damaged ligaments heal, instead, they get offered a several thousand dollar screw that’s banged across their SI joint. Why? Because their insurance company will cover the screw. The problem? Not only is this a stupidly invasive way to treat a simple problem, but as Shane points out in the Linkedin post above, he now frequently sees many patients with screws that never make it across the SI joint or that never fuse the joint as advertised. In this patient, one screw never got close to the SI joint where it belonged and the other never caused the joint to fuse.
Next up are the crazy stimulator leads that can be seen. When the SI joint fusion didn’t work, presumably the interventional pain physician tried to use an implantable stimulator across the sacral nerves to “block” the pain from the SI joint (“S3 peripheral stim leads”). The idea is that an implantable generator will cause the leads to emit an electrical pulse which will help the pain. Well, it looks like that didn’t work.
Next up are the dorsal column stimulator leads. This is a system installed at the back of the spinal cord to emit an electrical pulse to block the pain as it travels up that structure to the brain. These are shown as “3 total DCS leads” in the x-ray above.
Finally, presumably, when all of that didn’t work, we now see the “pièce de résistance”, which is the “Pain Pump”. This is an implantable reservoir usually filled with a narcotic that delivers small amounts of medication into the area right around the spinal cord. It needs to be filled periodically with more medication.
The Side Effects of the Hardware Store
The above x-ray looks like someone lost the contents of a shopping trip to the local hardware store in this patient’s body. However, while the stuff you could buy at the local Home Depot would cost a few hundred dollars, this is likely more than $100,000 worth of medical device hardware. Think about that for a second as that’s not even the real final cost. The total cost here, when hospital/ASC fees, professional, and anesthesia fees are added is likely hundreds of thousands of dollars.
While any procedure can have complications and side effects, what are the side effects of the hardware store approach?
- SI joint fusion – Banging huge screws across the SI joint can cause fractures, serious nerve injuries, a lack of fusion, infection, etc… In fact, we know that it will forever destroy this joint as there is no way to get around that fact. We also know that the fusion (if one is achieved), will lead to ASD, or overload of the L5-S1 area above and the hip joints below, wearing these levels out more quickly. I have covered these side effects as reported in an FDA database of SI joint fusion device complications here.
- Implantable local stimulator leads (S3 peripheral stim leads) – These systems have exploded in popularity these past 5 years. They are implanted at the site of pain and are left there permanently. They can cause local tissue damage, scarring, nerve injury, etc… We have no idea of the long-term side effects of leaving these at the site of pain.
- Dorsal Column Stim Leads (DCS leads) – These have all of the side effects of the local leads above, plus the specter of possible permanent spinal cord injury. In addition, since they have wires that go to them, those wires frequently break and need to be replaced and are also a site where infections can occur.
- Pain Pump – All of the same side effects of the DCS leads plus fatal overdose of the patient is possible.
WHY?
As I have said, this is happening, IMHO, due to the tremendous financial incentive that device manufacturers can provide doctors and insurers to get their stuff implanted. It’s just that simple. While it’s great to have lots of options to help patients, those incentives end up driving the use of these technologies more than they should be used. Meaning, less invasive and cheaper solutions are often overlooked in favor of implanting more invasive and more complication-laden solutions. For example, while it’s great to have the option of fusing someone’s SI joint, from what I observe, only a tiny fraction of the patients who end up with this procedure should have ever have had this procedure.
The upshot? At the end of the day, it’s disturbing to see these technologies become commonplace. As Dr. Rose points out in the LinkedIn post I linked above, the dark underbelly of these devices as he sees them come across his radiology viewing screens are the serious side effects and problems created by the devices themselves. Thanks to a really honest international radiologist for sharing this image!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
