What’s Causing Your Bladder Pain? Interstitial Cystitis Or Irritated Low Back Nerves

Image credit: Dragana991/Getty Images Pro
Physicians often miss the connection between interstitial cystitis (IC) — also known as painful bladder syndrome (PBS) or bladder pain syndrome — and low back pain. That’s because connecting the bladder to the low back involves two different specialties: one that treats the bladder and the other that treats the spine.
But 65% of those diagnosed with interstitial cystitis will experience low back pain, according to the International Urogynecology Journal and Pelvic Floor Dysfunction. Sadly, many patients with interstitial cystitis bounce around from specialist to specialist because few have the expertise to connect the dots.
The Story of My Burning Bladder and Interstitial Cystitis Diagnosis
I had a burning sensation in my bladder and was 100% convinced I had some sort of urinary tract infection (UTI) or prostate issue. I went to the urologist who performed his exam and tests, then announced I had “interstitial cystitis,” which, for a urologist, is like saying, “I don’t have a clue what’s causing your chronic bladder pain.”
A few weeks later, when my low-back sciatica fired up, one of my partner physicians gave me an epidural injection using the growth factors from my own blood platelets. My bladder pain suddenly dissipated. Researching the anatomy, it became obvious to me why this worked.
Since then, I’ve seen countless patients with bladder burning who get extensive medical workups and end up getting dubious alternative medicine treatments despite it being clear that their low back is the culprit. Each specialist evaluates and interprets the symptoms in their own way, but each misses the mark by a wide margin.
The Connection Between Bladder Pain and The Low Back
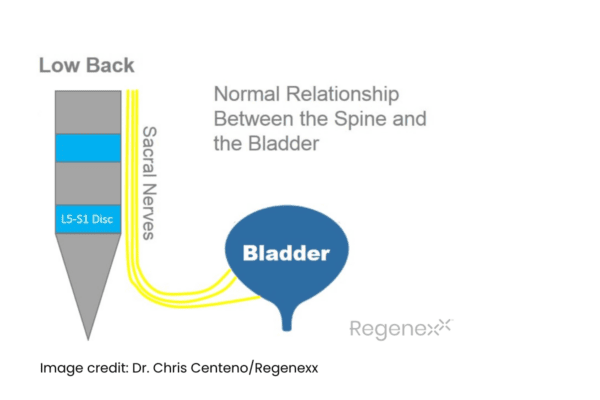
The diagram below shows the sacral nerves coursing by the L5-S1 disc in the low back. These then head toward the bladder and act as a conduit for bladder sensation. Without any pressure on the nerves, they function normally to allow the sensation from the bladder to reach the brain through these spinal nerves.
The diagram below shows what happens when an L5-S1 disc bulge or “slipped disc” places pressure on the sacral nerves. These irritated nerves cause spasms and pain in the bladder wall. They can also make the patient believe the bladder is full when it’s not, increasing urinary frequency. All of this happens because the nerve stimulation that creates bladder sensations get disrupted by the irritated sacral nerves.
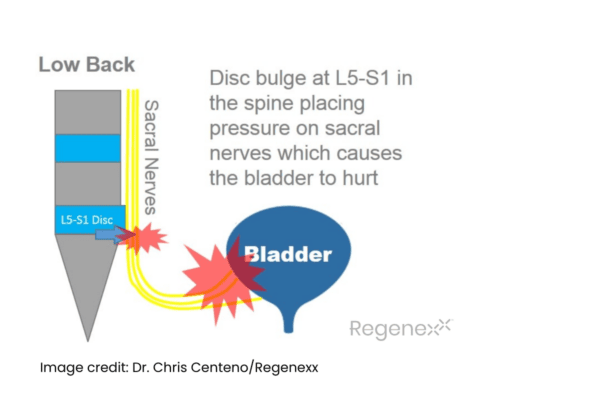
What’s even more interesting is that only some patients whose symptoms include bladder burning, spasm, and pain and get diagnosed with interstitial cystitis will have back pain. Many patients don’t have that symptom, even though the trouble spot is in the spine.
So whether you have back pain or not, irritated sacral nerves being from a disc bulge can still irritate your bladder.
Treating A Burning Bladder Sensation Due to Irritated Sacral Nerves
Despite all of the runaround interstitial cystitis patients go through to try to find effective treatment, the fix is usually simple if sacral nerve irritation is causing the issue.
Regenexx physicians use an injection of the growth factors isolated from the patient’s own platelets and delivered through a precise, fluoroscopy-guided caudal epidural to help calm the irritated sacral nerves. This can be combined with physical therapy to get the stabilizer muscles back online and help strengthen the pelvic floor muscles.
The upshot? Interstitial cystitis patients often lose hope when multiple specialists have prescribed everything from ineffective antibiotics to pelvic floor physical therapy. For some reason, most physicians never put 2 and 2 together to look at the lower back as a possible cause for the burning bladder.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
