Understanding Medical Risk Is a Key Life Skill

Credit: Shutterstock
If there’s one thing that patients often fail to understand it’s Medical Risk. In fact, this plays out every day usually to the detriment of otherwise smart people. So let’s explore that topic this morning.
Risk Is Everywhere
We all get up each morning and most of us hop in a car at some point in the day. Your chances of dying in a car crash in your lifetime are 1 in 107. Depending on where you live, your chances of a car crash death in any given year are between 10 and 25 per 100,000 people. Hence, this happens so infrequently that we just don’t think about it. How about other risks?
These were the current leading causes of death in 2020 according to the CDC (1):
- Heart disease (696,962)
- Cancer (602,350)
- COVID-19 (350,831)
- Accidents (200,955)
- Stroke (160,264)
- Lung Diseases (like COPD) (152,657)
- Alzheimer’s (134,242)
- Diabetes (102,188)
- Influenza and pneumonia (53,544)
- Kidney disease (52,547)
I’ve put that risk in a pie chart:
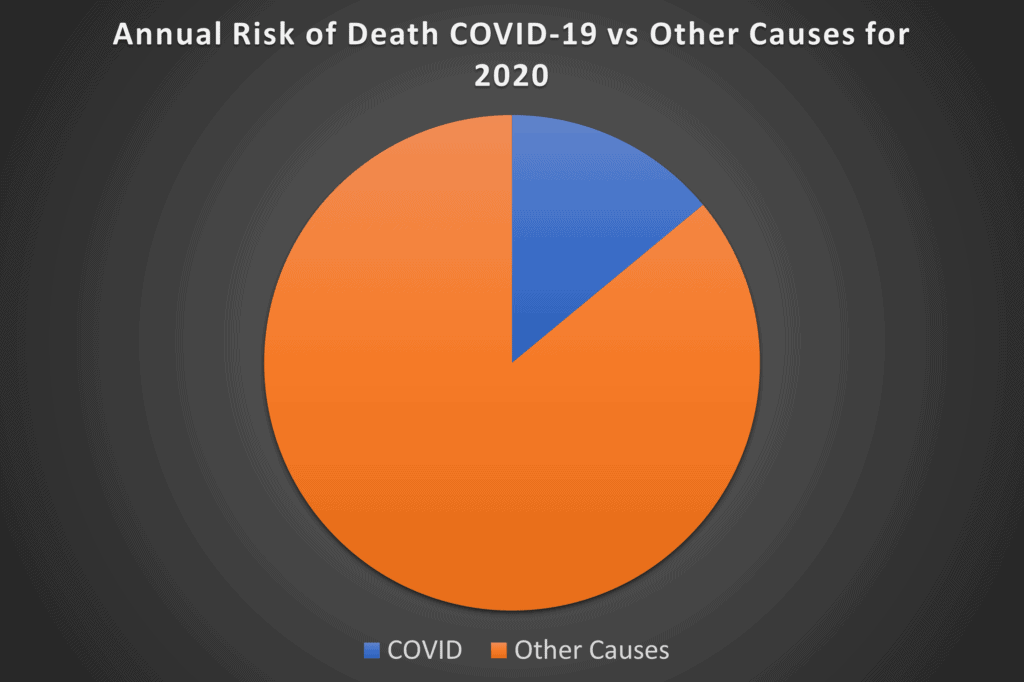
A quick glance above shows that you were MUCH more likely to die of something else in 2020 than COVID-19. In addition, this represents the risk of the much more lethal Alpha variant. The current Omicron variant is MUCH less lethal, so this pie chart for 2022 will look quite different with even less COVID death risk.
Despite these facts, I still see people out and about ignoring their diet, overall health, and other things they can control, wild-eyed with an N-95 mask looking like they have a 1 in 10 chance of dying on that trip to Whole Foods.
Why? We know the data doesn’t support that perception of risk. In this case, it’s because of the influence of mainstream and Social Media.
We Need an “Understanding Medical Risk” Course for Patients
While COVID is an easy example of how people don’t understand Medical Risk, I see patients every day who have no conception of how to interpret risk. For example, they skip over far less risky treatments and go right to invasive surgical procedures that carry far more risk of injury and death. Why?
Knowledge Asymmetry
Despite Dr. Google, knowledge asymmetry is alive and well in Medicine. This happens when you go to the doctor, who has much more knowledge about the risk of the treatment choices being presented. Here the physician fails to present all of the possible options or uses specific language to push a patient in one direction or the other. Let me get into an example.
Neurosurgeons love to use the “If I don’t operate soon you may become paralyzed” sales tactic in selling an invasive surgery. This often happens in patients with Spinal Stenosis or bone spurs causing less room for the Spinal Cord or nerves. A patient who hears this from an authority figure like a Surgeon is at a distinct knowledge disadvantage. How much knowledge asymmetry is there?
As a Physician who has seen patients become paralyzed or otherwise disabled by Spine surgeries go bad, I spent years searching for studies that compared these risks. I did finally find a way to compare the risk of spontaneous Spinal Cord injury because of Stenosis to the risk of surgery to correct that problem. It turns out that you’re 10 times more likely to be paralyzed by Spinal surgery than by Stenosis.
This is a great example of knowledge asymmetry. If an educated doctor who knows how to search the medical literature can’t immediately find the comparison of these two risks, how is the average patient going to be able to find out if the sales pitch they just got from the Surgeon is true? It’s never going to happen. Maybe they hit my 2019 blog that covers this comparison. However, since Google’s algorithms now prioritize information from university websites that never mention these comparative risks, the chances are that 99.99% of patients will never be able to judge these two risks side by side.
Desperation
Bad decisions are often made by desperate people. The same thing happens in Medicine. Patients who have been in pain or suffering for years tend to hang onto things that they’re told may help, despite the personal risk.
Take for example a choice I deal with every day with patients suffering from Craniocervical Instability. It’s trendy in this patient population to consider “Spinal Cord Detethering“. This is Neurosurgery to cut the anchor for the Spinal Cord to help release nerve tension. Does this work? There is scant medical evidence that supports this is a good idea. In fact, most of the positive responses are sourced on Social Media chat groups. We’ve seen a few people who have had disastrous results. In addition, given that this is invasive Neurosurgery, it should be a last resort for anyone that understands Medical Risk. Meaning, if you’re going to get this procedure done, at least exhaust everything else that’s less invasive. However, I still get questions of whether patients should do this before or after upper neck injections to help instability. The answer should ALWAYS be AFTER you have tried less invasive injections.
Cost
Regrettably, cost often pushes patients to make bad medical decisions regarding risk. For example, we have randomized controlled trials showing that simple and inexpensive Prolotherapy or Platelet-Rich Plasma injections can help Sacroiliac instability. However, because these solutions aren’t covered by most insurance plans, patients often skip over these much less invasive choices and get a MUCH more invasive SI Joint Fusion. The bizarre thing is that doing the math and considering the out-of-pocket co-pay, co-insurance, and deductible the Fusion is likely more or as much as the non-covered injections. However, the idea of out-of-pocket costs pushes patients to make an upside-down Medical Risk decision.
We also see people fail to consider all of the costs. For example, a self-employed person who needs to take a month off work because of a knee replacement will lose big bucks in income. That’s often more than the cost of less invasive procedures.
My Advice on Accessing Medical Risk
Here’s a list of things to do to properly access Medical Risk:
- First, slow down and do your homework.
- Realize that while physicians should be presenting you with a comparative risk assessment in an unbiased way, that’s rarely the case.
- Do the math on cost and don’t let it force you into bad decisions.
The upshot? Patients that understand medical risk make better decisions than those who don’t understand how to access risk. Our job as Physicians is supposed to be to help you understand the risks and benefits of all of the treatment options. Sometimes that happens, but often it doesn’t. Hence, like many things in Medicine, an educated patient is powerful!
_______________________________________
References:
(1) CDC. National Center for Health Statistics. Leading Causes of Death. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
