Is Spinal Stenosis Behind Your Persistent Back Pain?
Back pain is common, but when discomfort persists or limits movement, a more complex issue, such as spinal stenosis, may be involved. Spinal stenosis typically affects adults over 50 and involves a narrowing of the spaces in the spine, which may place pressure on nearby nerves, often leading to radiating discomfort in the arms or legs.
Unlike temporary back discomfort from soft tissue strain, spinal stenosis symptoms may gradually worsen over time, particularly during standing or walking.
At the Rehabilitation Medicine Center of New Jersey, part of the licensed Regenexx network, physicians may use procedures with Regenexx injectates to help support spinal function and target areas of structural dysfunction. These options are part of a comprehensive, less invasive approach to spine care.
What Is Spinal Stenosis?
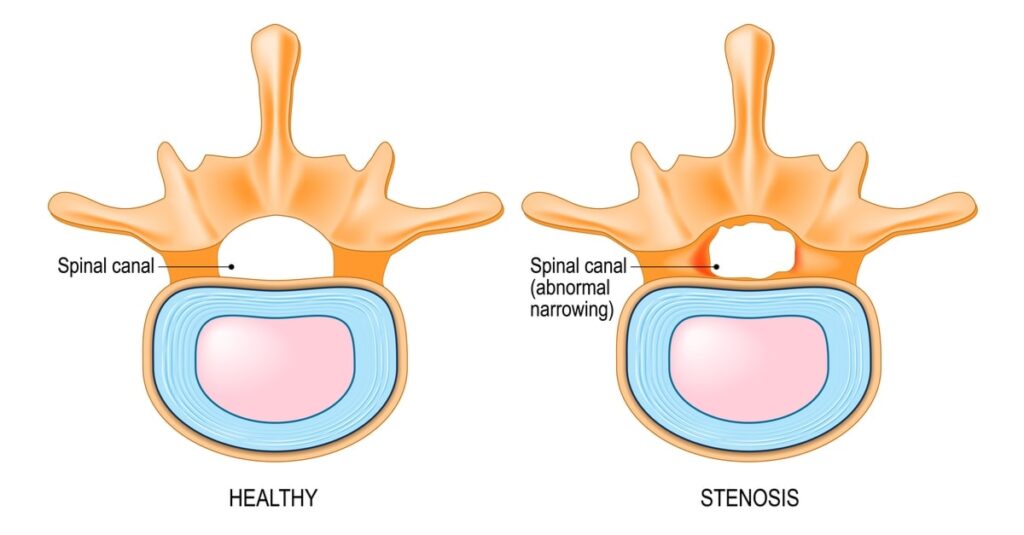
Spinal stenosis occurs when the open spaces within the spine begin to narrow, which may lead to pressure on the nerves that pass through the spinal canal. Each vertebra, the bones that make up the spine, features a central opening called the spinal canal, which serves to protect the spinal cord and the branching nerves that communicate with other areas of the body.
Under typical conditions, this canal allows sufficient room for the spinal cord and nerves to function without interference. However, when this space becomes restricted, nerve function may be affected. The narrowing is often associated with changes in surrounding spinal structures and may contribute to a complex clinical picture that requires a tailored and comprehensive treatment approach.
Stages Of Spinal Stenosis
Spinal stenosis may progress over time and can vary in severity from person to person. It is typically classified into stages based on how much the spinal canal has narrowed and the potential effects on nearby nerves. These classifications—ranging from mild to severe, can help physicians evaluate the condition and determine a treatment approach tailored to the individual. They may also provide helpful context for patients seeking to understand how their symptoms could change over time.
Outlined below are the three commonly recognized stages of spinal stenosis:
Grade 1 (Mild)
In the mild stage of spinal stenosis, the narrowing of the spinal canal is minimal and may not significantly affect daily activities. Individuals at this stage might occasionally experience stiffness or mild discomfort in the back, but these symptoms are often infrequent and manageable. Mobility and nerve function are generally unaffected during this stage.
Grade 2 (Moderate)
The moderate stage of spinal stenosis is characterized by a noticeable reduction in the space within the spinal canal, which may affect nerve function. Individuals at this stage could experience persistent discomfort, including back pain, numbness, tingling, or limb weakness. These symptoms might interfere with daily activities, particularly those requiring prolonged standing or walking.
Grade 3 (Severe)
The severe stage typically involves significant narrowing, which may lead to chronic pain, pronounced weakness, and difficulty with movement. Daily activities can become more limited, and symptoms such as impaired balance or coordination may develop.
Common Causes And Risk Factors Of Spinal Canal Narrowing
Spinal canal narrowing, a defining characteristic of spinal stenosis, may develop due to a variety of structural or degenerative factors. These changes can affect the stability and alignment of the spine over time. Below are several common causes and contributing risk factors that may be associated with this condition:
Genetics
Inherited traits may influence spinal anatomy and increase the likelihood of developing spinal canal narrowing. Some individuals are born with a congenitally narrow spinal canal, which may not cause symptoms initially but can elevate the risk of developing spinal stenosis later in life. A family history of spinal abnormalities, such as scoliosis or other congenital variations, may also contribute to structural vulnerability in the spine.
Lifestyle-Related Factors
Occupational or daily activities involving repetitive movements, heavy lifting, or prolonged periods of sitting or standing may place cumulative stress on spinal structures. Over time, poor posture or physical inactivity may contribute to wear and tear on the spine, potentially increasing the risk of canal narrowing and related symptoms.
Thick Ligaments
Ligaments within the spine, including the ligamentum flavum, play an important role in maintaining spinal stability. However, with age or chronic mechanical stress, these ligaments may become thicker and less flexible. When this occurs, they may encroach on the spinal canal and contribute to narrowing, which can lead to pressure on adjacent neural tissues.
Spinal Injuries
Traumatic injuries, such as those caused by falls, sports-related impacts, or motor vehicle accidents, can disrupt normal spinal alignment or cause fractures and dislocations. These structural changes may lead to immediate or gradual narrowing of the spinal canal, especially during the healing and remodeling phases following injury.
Tumors
Benign or malignant growths that develop near or within the spinal canal may occupy space and compress spinal nerves. While tumors are a less common cause of spinal stenosis, their presence can significantly impact spinal structure and function, underscoring the importance of thorough diagnostic evaluation in cases of unexplained back pain or neurological symptoms.
Arthritis
Degenerative joint conditions, such as osteoarthritis and autoimmune conditions like rheumatoid arthritis, are frequently associated with changes in spinal structure. Osteoarthritis can result in cartilage degradation and the formation of bone spurs, which may protrude into the spinal canal. Rheumatoid arthritis may cause inflammation and structural joint damage, both of which can contribute to narrowing of the spinal canal and nerve compression.
Other Spine Conditions
Spinal canal narrowing may also develop as a result of various spine-related conditions that influence spinal structure and alignment. These conditions can affect overall spinal stability and may contribute to the onset or progression of spinal stenosis. Below are several commonly associated spine conditions:
- Scoliosis: A sideways spinal curvature may misalign vertebrae, creating uneven pressure and potentially contributing to canal narrowing.
- Bulging Disc: When a spinal disc extends beyond its normal boundaries, it can encroach on the spinal canal, which may reduce space and potentially irritate nearby nerves.
- Herniated Disc: A herniated disc is a more advanced form of disc injury in which the inner material leaks through a tear, which may cause significant nerve or spinal cord compression.
- Spondylolysis: A stress fracture or crack in a vertebra, often in the lower back, may weaken spinal stability and potentially contribute to narrowing over time.
Recognizable Signs And Symptoms To Monitor
Spinal stenosis often develops gradually, with symptoms that may begin subtly and progress over time. Identifying these early signs may support timely evaluation, which could assist in managing symptoms and limiting further progression. The nature and severity of symptoms can vary based on the location and degree of spinal canal narrowing, but they often reflect irritation or compression of nearby nerves.
Below are some commonly reported signs and symptoms that may be associated with spinal stenosis:
Radiating Pain And Numbness
The spinal nerves that extend into the legs and feet are sensitive to pressure. When these nerves become compressed, individuals may experience lower back pain along with radiating symptoms such as numbness, tingling, or weakness in the legs and feet. These sensations may become more noticeable during activities like walking or standing and often improve with rest or while sitting.
Standing Intolerance
Standing intolerance is commonly reported among individuals with spinal stenosis. Prolonged periods of standing or walking may contribute to discomfort in the back or legs, sometimes described as numbness, tingling, or aching. As spinal canal narrowing progresses, tolerance for upright activity may decline. Symptoms often ease when sitting or leaning forward, positions that may temporarily reduce pressure on the affected nerves.
Muscle Cramps
Muscle cramps can occur in association with spinal stenosis and are often linked to nerve irritation within the narrowed spinal canal. These cramps typically affect the lower back or legs and may arise during movement or periods of rest. Nerve compression may disrupt normal signaling to the muscles, occasionally resulting in sudden, involuntary contractions or spasms.
- Low Back Pain: Low back pain may be caused by muscle strain, disc issues, or spinal degeneration. Accompanying symptoms may include stiffness, aching, or nerve-related symptoms, often aggravated by prolonged sitting, standing, or certain movements. Read More About Low Back Pain.
- Back Pain When Getting Up From A Chair: Pain when rising from a seated position may be due to muscle stiffness, joint degeneration, or spinal issues. It can cause discomfort in the lower back, often easing with movement but recurring with prolonged sitting. Read More About Back Pain When Getting Up From A Chair.
When To Seek Medical Attention
Some symptoms associated with spinal stenosis may indicate more significant nerve involvement and should prompt medical evaluation. These warning signs may reflect progression or complications that could require timely clinical attention. If any of the following symptoms occur, it is important to consult a healthcare professional:
- Worsening symptoms: Increasing pain, numbness, or weakness, particularly when walking or standing, may reflect greater nerve compression and should not be ignored.
- Changes in bladder or bowel control: New or worsening difficulty in managing bladder or bowel function may indicate more serious nerve involvement and may warrant urgent medical assessment.
Diagnosing Spine Health Issues
Physicians at Rehabilitation Medicine Center of New Jersey, NY, part of the licensed Regenexx network, focus on identifying the underlying sources of pain through a comprehensive evaluation to help determine whether the Regenexx approach may be appropriate.
During the initial consultation, a physician at the Rehabilitation Medicine Center location performs the four-part SANS evaluation, stability, articulation, neuromuscular function, and symmetry, to assess the structures contributing to discomfort. This process involves a full range of motion assessment and may include real-time ultrasound imaging to observe spinal structures in motion.
This evaluation is essential, as research indicates that an MRI showing spinal stenosis alone may not always confirm it as the true source of pain. Watch a physician in the licensed Regenexx network perform a real-time image-guided procedure designed to address disc-related spine conditions.
The goal is to identify the least invasive and most appropriate procedure to support improved function. The physician will determine whether a platelet-based procedure or a bone marrow concentrate (BMC) procedure may be an option based on individual needs.
How Is Spinal Stenosis Commonly Treated?
Conservative treatments for spinal stenosis are designed to help reduce irritation or inflammation around the affected nerves.
- Non-Steroidal and Inflammatory Drugs (NSAIDs): NSAIDs are commonly used to reduce inflammation and manage pain related to joint, muscle, or spine conditions, helping improve function. While they provide quick relief, NSAIDs do not treat the underlying issue causing the pain. Long-term use may lead to serious side effects, including heart and kidney issues. Read More About Non-Steroidal and Inflammatory Drugs (NSAIDs).
- Steroid Injections: Steroid injections reduce inflammation and provide temporary pain relief for joint, muscle, and spine conditions. While they may help manage symptoms, repeated use can contribute to tissue damage, joint degeneration, and systemic side effects, requiring careful consideration. Read More About Steroid Injections..
While steroid injections may offer short-term relief, they have been associated with potential risks, including side effects that may interfere with the body’s natural healing processes.
If conservative measures do not provide adequate symptom management, surgical procedures may be considered to relieve pressure in the spinal canal. This type of intervention often involves removing portions of bone, disc material, or ligaments to create more space for the spinal cord or nerve roots.
In some cases, spinal fusion surgery may be recommended to stabilize the spine by permanently connecting adjacent vertebrae using surgical hardware. Over time, this approach has been linked to a condition known as adjacent segment disease (ASD), where increased stress may affect the spinal segments above or below the fused area.
Surgical interventions such as spinal fusion are typically associated with longer recovery periods and may involve extended time away from normal activities.
- Spinal Fusion: Spinal fusion is a surgical procedure that connects two or more vertebrae to support spinal stability. It is commonly performed for conditions such as degenerative disc disease, spinal instability, or scoliosis. Read More About Spinal Fusion.
A Less-Invasive Alternative For Spinal Stenosis
Physicians within the licensed Regenexx network provide a non-surgical alternative for addressing spinal stenosis. Procedures using Regenexx lab processes involve the injection of customized concentrations of your biological materials into targeted areas of the spine to support the body’s natural healing response. These procedures may include platelet-rich plasma (PRP) derived from your blood or bone marrow concentrate (Regenexx SD injectate).
For individuals with spinal stenosis, the DDD procedure using Regenexx injectables offers a less invasive alternative to surgery. This approach aims to preserve your existing spinal structure while addressing the condition. Recovery time is typically shorter than with surgical intervention and may involve little or no reliance on opioid medications or extended time away from daily activities.
Discover Regenerative Relief For Spine Health Without Surgery
Spinal stenosis doesn’t have to result in ongoing discomfort or lead directly to surgery. At Rehabilitation Medicine Center of New Jersey, NY offers procedures using Regenexx injectables as an innovative, non-surgical approach that may help support spinal health, reduce discomfort, and improve function.
These less invasive, research-informed options, such as platelet-rich plasma (PRP) injections and bone marrow concentrate procedures, are designed to work with the body’s natural healing processes to address the condition.
Physicians at Rehabilitation Medicine Center of New Jersey, NY, tailor each procedure to the individual’s needs, offering a customized, non-surgical alternative for those seeking to improve spine function. Schedule a consultation to learn whether this approach may be appropriate for you.
131 West 35th Street
12th Floor
New York, NY 10001
Request an Appointment
Call to Schedule Schedule OnlineClinic Hours
| Sunday | Closed |
| Monday | 8AM–8PM |
| Tuesday | 8AM–8PM |
| Wednesday | 8AM–8PM |
| Thursday | 8AM–8PM |
| Friday | Closed |
| Saturday | Closed |
How to Treat Spinal Stenosis Without Surgery?
During Regenexx’s outpatient procedures, custom concentrations of your body’s natural healing agents are injected into the exact areas of damage in the spine. Treatments use only your own blood to make super-concentrated platelet-rich plasma (PRP) or your own bone marrow concentrate (BMC), which contains stem cells.
Spinal stenosis treatment may include Regenexx-DDD protocol, which is the world’s first alternative to stenosis surgery that allows you to maintain your normal anatomy. Best of all, your downtime will be a fraction of what it is with surgery and generally requires little or no opioid pain medications or time off of work.
Am I a candidate?Webinar: Treating Back Pain Without Surgery

Join Chris Centeno, MD, founder of Regenexx, to learn how Regenexx procedures can help treat your back pain without surgery and lead to a faster recovery.
During this free webinar you’ll learn:
- How procedures using bone marrow concentrate (BMC) and platelet-rich plasma (PRP) compare to surgery and other spine pain treatment options
- Procedure expectations
- Answers to the most common questions about regenerative medicine treatments
Is Regenexx Right For Your Spinal Stenosis?
At Regenexx, we want the best outcomes for everyone. So we’ve developed a process to determine if our treatments may be right for you.
During your initial appointment, your Regenexx doctor will use our four-part SANS (stability, articulation, neuromuscular, and symmetry) evaluation to identify the underlying causes of your pain. Your doctor will examine your injury through a full range of motion and may use ultrasound to observe the inner workings in real time.
This is important, as research shows that an MRI indicating stenosis isn’t enough to appropriately diagnose stenosis as the cause of back pain.
Am I a candidate?Watch a real Regenexx spinal procedure performed by a certified Regenexx physician:
Our goal is to use the least invasive, least expensive procedure to get the desired results. Your Regenexx physician will work with you to determine whether that would be a platelet procedure or a BMC procedure.
