Spinal Fusion Is It Worth It? More Research Says No…
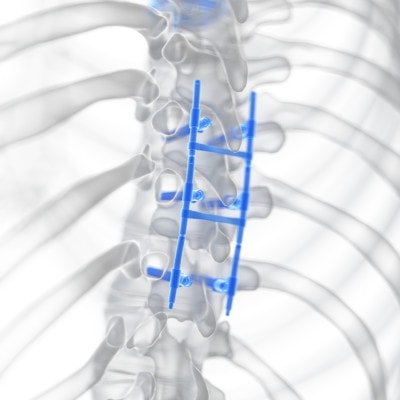
A spinal fusion is a surgery that uses hardware and screws to “fix” together two or more vertebrae to make a damaged section of spine immovable. Given that this is a big surgery with many known serious side effects, a patient the other day posed this question: “Spinal fusion is it worth it?” My answer, based on what I already knew, was a strong no, but when I dug deeper into the research, my resolve deepened.
SciePro/Shutterstock
So what is spinal fusion? One of the more common types of fusions is called a 360 degree fusion (360 fusion) because it fuses together the vertebrae from both the front and back sides of the spinal column. Fusion surgery is commonly done when a patient has some type of degenerative disc disease, herniated discs, stenosis, or other spinal injuries that cause pain or spinal instability. These surgeries are lengthy, risky, and painful, and besides the fact that the term “fusing” seems more suited a welder’s trade than a surgeon’s—or perhaps because of it—the truth is, long-term 360 degree fusion outcomes are awful!
To address why spinal fusions are such a bad idea, we’ll first explain the structures of the back, and then we’ll jump into the latest of many studies showing the ineffectiveness of spinal fusion surgery.
The Structures of the Spinal Column
To answer the question,”Spinal Fusion is it worth it?, you need to understand the spine and how it works.
The spine is like a series of blocks stacked one upon the other, creating structure and containing and protecting the spinal cord. The “blocks” are our vertebrae, or the bones in our spinal column, and there are discs between each vertebra for absorbing shock.
Some other structures along our spine include facet joints, which control the motion between each vertebra. Our spinal column also protects our spinal cord, which is like a bundle of wire containing all of our nerves and nerve roots that, along with the brain, make up our central nervous system. These nerves transmit feeling and tell our muscles what to do. It’s all held together by ligaments and kept stable by a series of muscles called multifidus, and the column has natural opposing curves to distribute our weight and provide stability. A more in-depth description of the spine can be viewed in my video below.
Damage (degenerative or an injury) to the discs, vertebrae, ligaments and other structures can cause instability. Fusion surgery is done when vertebrae become so unstable that movement affects the nerves or causes pain. But the problem from a structural standpoint is that making two or more vertebrae “fixed” and immovable simply puts more stress and load on the vertebrae above and below the fusion, which causes degenerative arthritis and can lead to Adjacent Segment Disease (ASD) as you’ll see in the study highlighted next.
Study Shows Serious Issues with 360 Degree Lumbar Fusions
A new study looked at circumferential lumbar fusions (360 degree lumbar fusions) in 73 patients at 2, 5, 10, and 15 years postop. While the fusions show good short-term results, this is deceiving; there is actually a progressive worsening of the patients’ conditions throughout the duration of the study. Take a look at these statistics below showing the number of patients who underwent revision surgeries because of Adjacent Segment Disease (ASD), or degeneration in the disc levels adjacent to, or above and below, the fusion:
- By 5 years postop, 7 patients required revision.
- By 10 years postop, 18 patients required revision.
- By 15 years postop, 24 patients required revision.
Are you seeing a pattern? Is the answer to Spinal Fusion is it worth it getting clearer? Even more stunning is the fact that by 10 years, 37 (51%) of the 73 patients showed ASD on radiology exams. The study concludes, “The high rate of ASD occurrence and reintervention questions the reliability of this technique for lumbar fusion.”
Between 10 and 15 years postop, the average ODI scores (which measure the degree of disability) for the patients in this study had returned to the levels they were at before the 360 fusion. What’s amazing about this study is that it’s one of the few that seems to match what we see in the clinic every day, even with fusions that only install hardware on the back part of the spine. While other studies show that adjacent levels break down due to the fusion, they always seem to minimize the phenomenon and somehow blame it on the patient. For example, some are now claiming that it’s bad genetics that are responsible for these poor sad sacks who have rapid deterioration of the levels next to the fusion. Huh? These levels would have been fine without the fusion, even with the patient’s genes.
There are many different types of spinal fusion surgeries out there, and each carry significant risks with them. One of the most common is posterolateral gutter fusion, which places bone graft in the region that lies right outside the spine. Posterior lumbar interbody fusion is done from the back and involves the removal of the disk found between the affected vertebrae. Anterior lumbar interbody fusion is a type of surgery approached from the front instead of the back, like the PLIF version. Extreme lateral interbody fusion is similar to the others but done from the side.
Yes, there are many spinal fusion surgeries, but let’s take a look at the risks involved. For most kinds of spinal fusion, there’s a chance that surgeons are unable to solidly fuse the vertebrae, which would require another surgery in the future. In cases where the fuse is solid, patients may also experience what is referred as Adjacent Segment Disease or ASD. This is what happens when a segment adjacent to the fused area begins to break down thanks to an increase in stress. Some types of spinal fusion surgery, like anterior lumbar interbody fusion surgery, carry added risks. Due to the nature of the surgery, the procedure comes close to large blood vessels. Any damage done to those blood vessels could lead to a great deal of blood loss.
Other complications may arise in a major surgery such as this one. Patients may experience blood clots, infection, bleeding, pain, and the risks that come from using anesthesia. But that’s not the end of potential problems. A surgery dealing so closely with the spine may end up causing a nerve injury. Mild conditions of this may result in sensations of tingling or even numbness in the leg. A more serious complication would be losing movement in a limb. Outside of nerve injuries, patients may also have to deal with donor bone graft issues, the most common being tissue rejection and infection.
For some, the potential issues and complications are risks they’re willing to take for pain relief. However, even in cases where spinal fusion is successful, there’s always a risk that the patient’s pain doesn’t completely go away. It might even get worse. Think about that for a moment. Getting rid of pain is the very reason someone undertakes such a drastic surgery, and there’s a notable chance that they won’t get the outcome they wanted.
The other thing to consider is the spinal fusion surgery recovery process. A surgery of this scope will require a hospital stay of around four days, possibly more. The patient will need to be hooked up to medical devices, from a heart monitor to an IV and catheter. Even when the patient is out of the hospital, they’ll need follow-up appointments for months and even years afterwards. And that doesn’t count the physical therapy they’ll need before they’re back to where they want to be.
Other Poor Outcomes Due to Spinal Fusions
While I have seen a few patients who have a severe instability that can only benefit from a fusion, these patients are rare. More often than not, post-fusion patients require revision surgeries; need ongoing narcotics following surgery; experience complications due to their surgery, such as irrevocable damage to the multifidus muscle; and spend a lot of money on a serious surgery providing very little to no long-term returns. With results this poor and so much research showing reasons not to, why would you want a fusion?
Even more concerning is the fact that we don’t have any high-level evidence that spinal fusions are effective. There are low-level studies published by spine surgeons and fusion-device manufacturers that seem to show that fusion works. However, this doesn’t fit with the clinical experience of anyone who sees a lot of post-fusion patients who are still in pain. And it certainly doesn’t mesh with high-level studies such as the one above showing glaringly poor 360 fusion outcomes.
In addition, in the case of spinal stenosis, for example, spinal fusions are far more dangerous due to their complication rates than the decompression surgery they’ve gradually replaced over the last 10–20 years.
The upshot? So spinal fusion is it worth it? Just because a 360 degree fusion is the popular option doesn’t mean it’s the safest or most effective option. The spine is not meant to be a stationary structure, so leave the fusing to the welders, and look into other options to address your pain and spinal instability that will allow you to maintain the natural movement and curve of your spine.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.