Treating the Cervical Spine Like It’s 1999!

If you read this blog, you know I often write as a type of catharsis. I see something in our medical care system that seems so nutty that if I don’t write about it, I’ll explode. This morning, a poor, dizzy patient in Australia was being treated like he lived in the last century, not this one. Let’s dig in.
Writing as Catharsis
When my mother would get upset at something, she used to say that this was “getting her vinegar up,” a phrase she used that meant that she was pissed off. I’ll see something so silly a few times weekly that it gets my vinegar going. Writing about it then serves a dual purpose. First, it’s easy to write these blogs because of that vinegar; second, writing serves as the needed catharsis to allow me to process the silliness.
The Australian Patient
This morning, I performed a telemedicine visit on an Australian patient in his 30s. He has a particular type of dizziness. Often, when he’s lying in bed at night, his upper neck will ache, and then this is followed by the room spinning. This is called cervicogenic dizziness or dizziness that’s coming from the neck.
He had already had some treatment locally, and this consisted of:
- Left-sided C3-C6 intra-articular facet injections with corticosteroids using CT guidance
- Left-sided C3-C6 medial branch radiofrequency ablation (RFA) using CT guidance
The good news is that this reduced his neck pain and partially helped his dizziness. The bad news is that I haven’t heard of CT-guided facet injections in the US since the late 1990s. Why? Because the X-ray exposure is 10X what it would take to use C-arm fluoroscopy with contrast.
Does treating the above levels make sense? For neck pain, yes, but for dizziness, NO. Dizziness is a phenomenon heavily associated with the upper cervical spine. However, if all you did were to look at his MRI report, you would think he has no issues:
Here, his C2-C3 level is read out as normal, but is it? Nope, he has very clear evidence of left C2-C3 osteoarthritis:
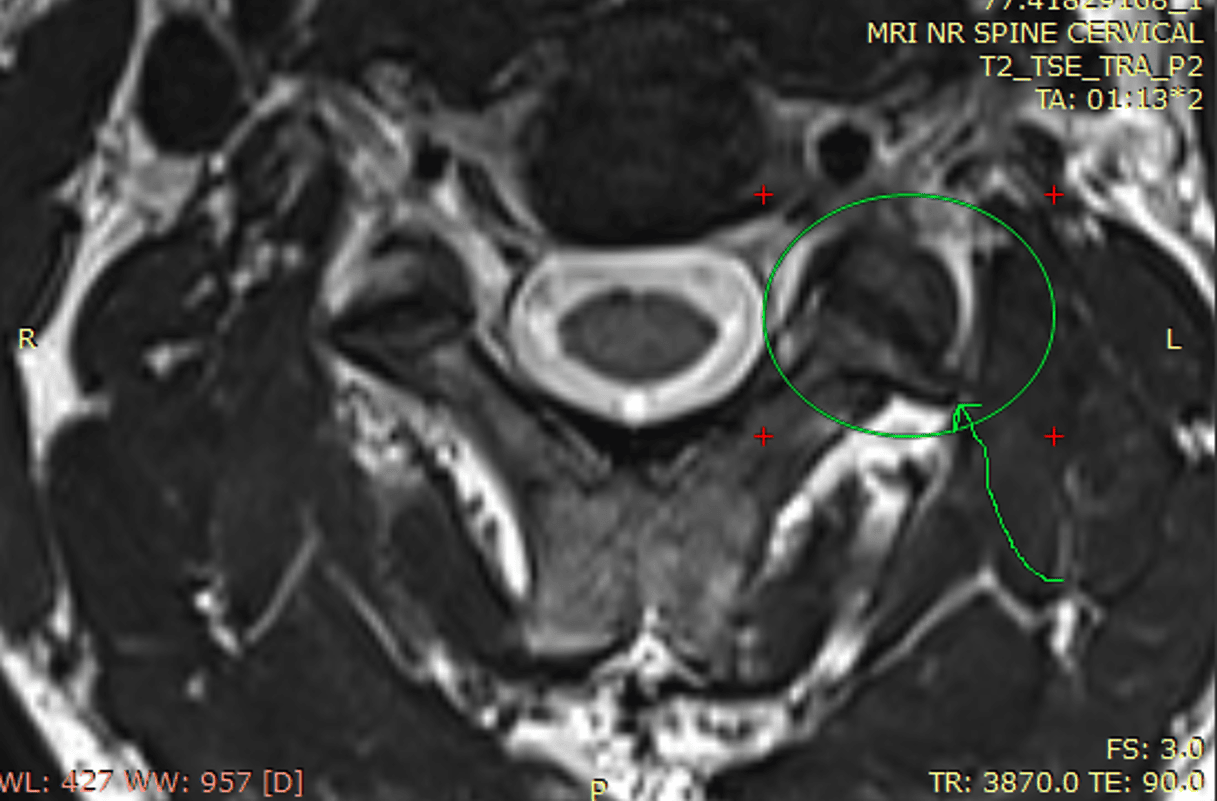
That arrow points to a clear osteophyte (bone spur) coming off the left C2-C3 facet joint. Hence, this level is “WNL” ONLY if that stands for “We Never Looked.” Given that the C2-C3 facet joints can cause dizziness by providing bad position sense information to the brain and inner ear, this could have been a target of the aforementioned 1990s-style CT-guided facet injections.
If his C2-C3 level is causing his dizziness, why was the RFA of C3-C6 partially helpful for his dizziness? The C2-C3 facet joint is innervated by:
- C2 medial branch
- Third occipital nerve
- C3 medial branch
Hence, his provider denervated the C3 medial branch, so they treated 1/3 of this left-sided neck joint. Hence, some part of his dizziness was helped.
Facet Corticosteroids vs RFA
Corticosteroid joint injections are a treatment that can be traced back to the 1950s. However, regrettably, we now know that using these powerful anti-inflammatory drugs in joints chews up the cartilage and causes everything from more arthritis to an increased risk of joint infections (1-12). Hence, injecting milligram dose corticosteroids into the facet joints makes no sense in 2024.
We also know that RFA can destroy the small stabilizing muscles of the spine called multifidus. These muscles atrophy in chronic neck pain patients. So why are we doing something that can damage these stabilizers in this patient?
In addition, this patient is unstable at C2-C3 on his imaging. RFA is CONTRAINDICATED in spinal instability because it will make the instability WORSE.
How Should This Patient Be Treated?
First, we need to inject something into these facet joints that can help them, such as Platelet-Rich Plasma (PRP). We have data showing that high-dose PRP is a DMOAD (Disease-Modifying Osteoarthritis Drug).
In addition, since his C2-C3 is unstable, the ligaments that stabilize the spine are damaged. Hence, orthobiologics need to be targeted into those ligaments, which will improve his instability.
Why Was this Patient Treated Like It’s 1999?
Whether in the US or in a socialized medical care system, the reason for treating a patient like it’s the 1990s is insurance coverage! This means physicians will only do what is covered, even if it’s not the best thing for the patient. While that sounds crazy, Prince would be proud as it’s all a big insurance-sponsored party “like it’s 1999”!
The upshot? This Australian patient is getting treated like it’s 1999. To my colleagues, stop treating patients based on what their insurance will cover! How about treating them with what makes the most sense for the patient? Also, cervicogenic dizziness is common, which should provide a clue as to whether the upper neck is a possible cause.
_______________________________________________
References:
(1) McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA.2017;317(19):1967–1975. doi: 10.1001/jama.2017.5283
(2) Wijn SRW, Rovers MM, van Tienen TG, Hannink G. Intra-articular corticosteroid injections increase the risk of requiring knee arthroplasty. Bone Joint J. 2020 May;102-B(5):586-592. doi: 10.1302/0301-620X.
(3) Richardson SS, Schairer WW, Sculco TP, Sculco PK. Comparison of Infection Risk with Corticosteroid or Hyaluronic Acid Injection Prior to Total Knee Arthroplasty. J Bone Joint Surg Am. 2019 Jan 16;101(2):112-118. doi: 10.2106/JBJS.18.00454.
(4) Kang SS, Hwang BM, Son H, Cheong IY, Lee SJ, Chung TY. Changes in bone mineral density in postmenopausal women treated with epidural steroid injections for lower back pain. Pain Physician. 2012 May-Jun;15(3):229-36.
(5) Ravi B, Escott BG, Wasserstein D, Croxford R, Hollands S, Paterson JM, Kreder HJ, Hawker GA. Intraarticular hip injection and early revision surgery following total hip arthroplasty: a retrospective cohort study. Arthritis Rheumatol. 2015 Jan;67(1):162-8. doi: 10.1002/art.38886.
(6) Chon JY, Moon HS. Salivary cortisol concentration changes after epidural steroid injection. Pain Physician. 2012 Nov-Dec;15(6):461-6.
(7) STEINBROCKER O, EHRLICH ME, SILVER M, SICHER W, BERKOWITZ S, CARP S, FEISTEIN H. The clinical application of cortisone and ACTH in arthritis and related conditions: methods and problems. II: Side effects complications, contraindications, precautions and conclusions. Ariz Med. 1951 Sep;8(9):29-35.
(8) Brånemark PI, Goldie I. Observations on the action of prednisolone tertiary buryl acetate (Codelcortone TBA) and methylprednisolone acetate (depomedrone) on normal soft tissues. Acta Rheumatol Scand. 1967;13(4):241-56.
(9) Wang BL, Sun W, Shi ZC, et al. Decreased proliferation of mesenchymal stem cells in corticosteroid-induced osteonecrosis of femoral head. Orthopedics. 2008;31(5):444. doi:10.3928/01477447-20080501-33
(10) Bonnevialle N, Bayle X, Projetti F, Wargny M, Gomez-Brouchet A, Mansat P. Variations of the micro-vascularization of the greater tuberosity in patients with rotator cuff tears. Int Orthop. 2015;39(2):371‐376. doi:10.1007/s00264-014-2628-z
(11) Murray RC, DeBowes RM, Gaughan EM, Zhu CF, Athanasiou KA. The effects of intra-articular methylprednisolone and exercise on the mechanical properties of articular cartilage in the horse. Osteoarthritis Cartilage. 1998;6(2):106‐114. doi:10.1053/joca.1997.0100

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
