Are All Hip Replacement Devices Associated with Pseudotumors?
A few years back, I blogged on a research study that looked at masses that were associated with metal-on-metal hip replacement surgeries called pseudotumors. However, now new research shows that these awful side effects may be more common than anyone realized and occur with other types of hip replacement devices as well. In fact, they may be a very common side effect of all hip replacement surgeries.
What Is a Pseudotumor?
Pseudotumors are growths in the body that look like tumors. They can occur as a result of inflammation, a buildup of fluid, or some other tissue reaction. They can occur in a variety of locations in the body, and oftentimes it’s uncertain what causes them. Today, however, we’re going to focus on hip replacement pseudotumors, or those that occur following hip replacement as research has shown that one-third of hip replacement patients will go on to develop a one-inch or larger pseudotumor. Hip replacement pseudotumors can cause pain, inflammation, and other discomfort when they press against nerves and blood vessels near the joint.
Why Are Hip Replacement Pseudotumors so Common?
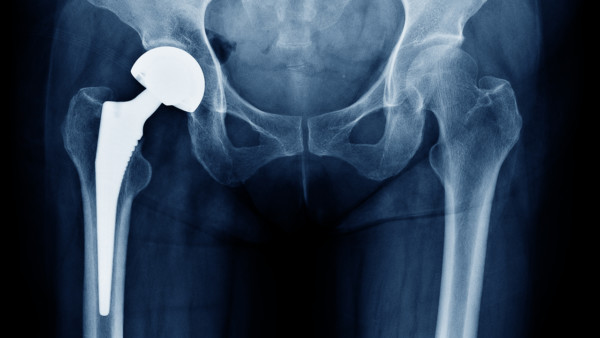
X-ray showing a hip replacement. ChooChin/Shutterstock
A hip replacement involves removing the native hip and replacing it with a prosthetic device (an artificial hip) designed to function like a hip. These devices are made from a variety of synthetic materials, such as metal, polyethylene (plastic), and ceramic. The hip joint is a ball-and-socket joint, meaning the ball that forms the head of the femur bone (upper-leg bone) fits into the socket (acetabulum) of the pelvic bone, and this creates the rotational hip joint.
As with any mechanical device, hip replacement devices wear down over time. It’s been well documented in the literature that the wear and tear of metal rubbing against metal in these artificial hip devices creates metal shavings. This results in toxic metal ions in the blood as well as soot-like particles that cause tissues to react by creating pseudotumors. However, these wear particles aren’t just limited to the metal-on-metal devices as other studies have shown that all of these hip replacement devices create wear particles.
Our feature study today looks at wear particles from hip replacement devices and suggests that the metal-on-polyethylene devices fare just as poorly (and in certain cases, worse) as the metal-on-metal devices in regards to the formation of hip replacement pseudotumors. Let’s take a look.
Different Types of Hip Replacement Devices
There are a dizzying array of hip replacement devices out there! Metal, plastic, and ceramic are the most common materials used. However, there are now many variants of each main material. For example, the plastic used by manufacturers for many years was polyethylene. However, more recently, a stronger version of the plastic called “cross-linked” polyethylene was developed. In addition. there are different metal and ceramic variants as well.
These different devices are named by the material that makes up the new ball and socket. So “metal on metal” (MoM) means that the ball is metal and the socket is metal. Metal on plastic (MoP) means that the ball is metal and the socket is plastic. You get the idea…
Pseudotumors Not Limited to MoM Hip Replacement Devices
The new study consisted of 111 subjects who underwent metal-on-metal hip replacement (n=30), metal-on-polyethylene (n=71), and metal-on-metal hip resurfacing (n=47). In a hip resurfacing procedure, the head of the femur (the ball) is not removed—it is instead cut back and a metal cap is placed over it. The acetabulum, or socket, is also lined with a metal insert.
The results? The prevalence of pseudotumors in general was nearly the same in the MoM (43%) and MoP (41%) hip replacement patients. While the hip resurfacing subjects fared better, still a disturbing number (28%) went on to develop pseudotumors. The interesting finding here, however, was that certain types of pseudotumors were significantly more prevalent in the MoP subjects with 10 of the MoP subjects displaying mixed or solid pseudotumors (34%) while 3 of the MoM subjects developed these pseudotumors (23%). This is significant because subjects who had these mixed or solid pseudotumors had higher levels of metal ions in their blood; poorer clinical scores measuring pain, function, and range of motion; and poorer patient-reported outcomes regarding pain and function.
Researchers concluded that pseudotumors associated with poorer pain and function outcomes were found to be more prevalent in metal-on-polyethylene hip replacement patients.
Pseudotumors Aren’t the Only Hip Replacement Problems
Hip replacement problems aren’t limited to pseudotumors. This surgery comes with many potential and painful complications. Let’s review a few I’ve covered over the years.
- If you’ve had a lumbar fusion, this increases your risk of dislocation following a hip replacement. And the more fusion levels, the higher the risk of dislocation. In addition, having just about any low-back problem (arthritis, disc issues, etc.) can be a risk factor for hip replacement.
- The alignment of not just the hip but also the knee can be changed following a hip replacement, which can disrupt the biomechanics of the leg and lead to more problems in the future.
- In men who undergo hip replacement, the heart attack risk is almost double.
- Stroke risk increases significantly following hip replacement.
- Allergies to the hip replacement device are common, and a good indicator that you could be at risk is if you have any allergy in general (e.g., pet dander, seasonal, etc.).
The upshot? It blows me away how many patients are walking around out there with masses around their hips created by a reaction to their hip replacement device! This means that in patients with pain or other issues after hip replacement, we physicians need to have a much higher index of suspicion that a pseudotumor could be pressing on nerves, arteries, or veins. In addition, many types of hip replacement devices can be the culprit! You just can’t make this stuff up!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
