Bone Cement to Treat Bone Marrow Lesions in a Knee?
One of the hottest trends in arthritis treatment right now is the idea that you need to treat bone marrow lesions if found on MRI as well as cartilage. This is a new procedure has many names. This opportunity has excited the companies that make bone cement, and they have created devices to inject this into these weak bone areas. While some of the bone cement-injected patient knees I’ve seen presented at conferences seem to do well, I’d like to present a patient we saw in clinic last week who did very poorly.
What Is a BML?
BML means bone marrow lesion. Another name for it is BME, or bone marrow edema. It’s a bright or dark spot (depending on the type of MRI sequence) that’s seen in the bone, usually in a patient with arthritis. For many years these were ignored by doctors, but in the last decade and especially the last five years, it’s become clear that in many patients, these spots in the bone that represent swelling or bone damage are part of the arthritis process. In addition, other research shows that while many patients with lost cartilage or torn meniscus tissue don’t feel pain, patients with BMLs are more likely to have pain. Hence, it may make sense to treat BMLs to help arthritis.
What Is Bone Cement?
Bone cement is an injectable paste that hardens in the body and takes the place of bone. It’s supposed to be broken down by the body and replaced by bone. One type of bone cement is basically plexiglass (polymethyl methacrylate). This type of bone cement heats up (exothermic) when it cures, so it could be harmful to local cells on that basis alone. The type of bone cement used typically to treat BMLs is endothermic (doesn’t heat up). This is usually calcium phosphate cement, which is closer to the actual bone composition than plexiglass.
Bone Cement Companies Get in on the Action
Given that bone cement is in itself an industry and that there is an opportunity in developing devices to help place this product in BMLs in knee arthritis patients, we’ve seen bone cement manufacturers start studies to treat knee arthritis. The concept is that if you can stabilize these weak areas in the bone, you can help the patients’ pain and maybe their cartilage. I have seen some nice cases presented at conferences showing that injecting bone cement can help patients. Having said that, I have also seen cases presented where the cement seeped from the bone into the joint and caused some real disasters.
Our Patient Where Bone Cement Was a Disaster
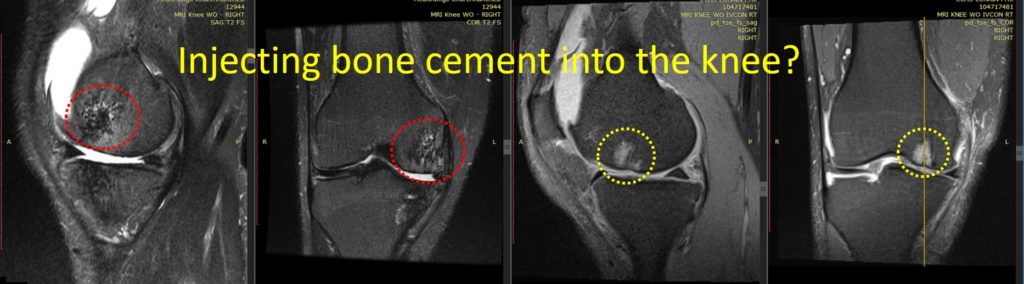
A patient presented to us recently to treat his knee arthritis with stem cells. He had previously had an arthroscopic debridement surgery and at the same time, the orthopedic surgeon injected bone cement into his BMLs. The surgeon admitted that this was his first case of a bone cement injection. The patient proceeded to get much worse, so we asked for a new MRI, which is above. Note that the two images on the right are the “before” images showing the BML bright spots in the bone (yellow dashed circles). Note that the after images are the two on the left. What we should be seeing is normal dark bone, but instead what we see in the red dashed circles is a disaster. The bone looks like it has died off and tried to heal, leaving gaps and holes. In addition, he has lost significant cartilage between the two films. Given that this is about nine months after the bone cement injections, this bone cement procedure has done the opposite of what was expected.
What Else Could Be Injected?
We’ve had data since the 1990s, mostly published by Phillipe Hernigou in Europe, showing that injecting bone marrow concentrate (same-day stem cell procedure, or BMC) can help heal bone. Hence, it would make sense that instead of bone cement, this may be a better substance as it’s natural and from the patient. This is one area where our knee arthritis research has focused. We are now readying for publication a matched case-control series showing that injecting these BMLs with BMC does help knee arthritis outcome in patients receiving a same-day stem cell procedure in their joint. Meaning that in patients with knee arthritis and BMLs, their function was better when the bone and the joint were injected versus just the joint.
The upshot? The pictures above look awful, so it’s unclear why this happened. Was the patient allergic to a component of the bone cement? Did this get infected? Is this just how some patients respond to bone cement? There are more questions than answers, but right now we’ll just stick with injecting the patients’ own stem cells into BMLs!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.