Shoulder Osteoarthritis: Causes, Symptoms, And Treatments

Medically Reviewed By:
Shoulder discomfort can make daily activities, such as lifting groceries, reaching, or dressing, more difficult. When stiffness or limited motion interferes with routines, it may suggest a more advanced issue. One condition that may contribute to these limitations is shoulder osteoarthritis (OA).
This article outlines the potential causes and symptoms of shoulder OA, as well as treatment options that may help reduce pain and improve joint mobility.
What Is Shoulder Osteoarthritis?
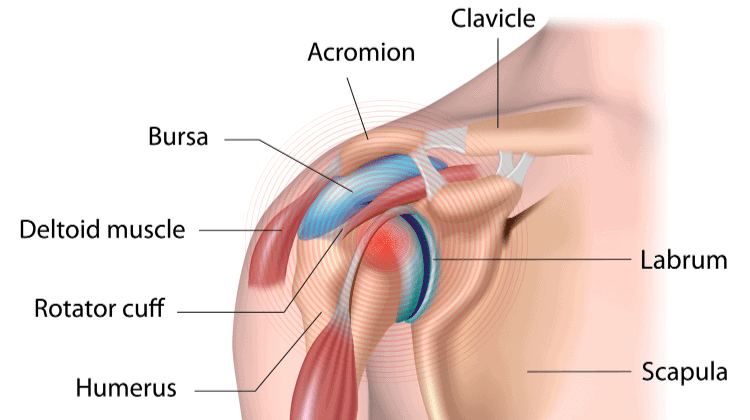
Shoulder OA is a form of degenerative arthritis that results from the gradual loss of protective cartilage within the shoulder joint. Unlike inflammatory types of arthritis that may affect multiple joints, shoulder OA typically involves a single joint, most often the glenohumeral joint, where the upper arm bone (humerus) meets the shoulder socket (glenoid).
Cartilage helps cushion the joint and reduce friction during movement. As this cartilage wears away over time, the bones may begin to rub directly against one another. This may lead to pain, stiffness, and reduced shoulder mobility. Age-related wear and tear, repetitive joint use, prior injury, and certain underlying conditions may contribute to the progression of shoulder OA.
An estimated 30% of adults over 60 have shoulder OA. While a range of treatment options is available, some nonsurgical interventions, such as corticosteroid injections, may provide only temporary relief and are associated with cartilage damage over time. Surgical outcomes vary, particularly in cases of complex joint damage or other health factors.
Identifying Key Signs And Symptoms
Shoulder OA typically develops over time, and symptoms may vary depending on the extent of cartilage wear and joint involvement. Common signs that may indicate shoulder OA include:
- Grinding sensation: A feeling or sound of grinding, clicking, or popping within the joint, especially during overhead or circular arm movements.
- Joint instability or weakness: The shoulder may feel less stable or reliable when lifting objects, raising the arm, or performing daily activities.
- Limited range of motion: Difficulty lifting the arm overhead, rotating it, or reaching behind the back due to joint stiffness or discomfort.
- Localized pain: A deep, aching sensation in the shoulder joint that can worsen with use and ease somewhat with rest.
- Stiffness and tenderness: Reduced flexibility, particularly after periods of inactivity, along with soreness when moving or pressing on the joint.
- Occasional swelling or discoloration: Inflammation or minor tissue irritation around the shoulder may lead to visible swelling or bruising after activity.
- Tight Pecs And Shoulder Pain: Tight chest muscles or pecs can contribute to shoulder pain by restricting movement and altering posture. This may lead to discomfort, reduced range of motion, and increased strain on the neck and upper back. Read More About Tight Pecs And Shoulder Pain.
Causes Of Shoulder Joint Degeneration
Shoulder OA is often associated with gradual cartilage wear over time, but other factors may contribute to joint degeneration. Common causes include:
Age
As individuals age, the shoulder joint may become more vulnerable to structural changes contributing to OA. Reduced circulation to joint tissues, slower cellular repair, and changes in cartilage composition are common with aging and may influence how the joint responds to daily wear. These changes can increase the likelihood of shoulder OA.
Injuries Or Trauma
Shoulder OA may develop more quickly following an injury. Fractures, dislocations, or soft tissue damage, such as rotator cuff tears, can disrupt normal joint alignment or movement patterns. Even after recovery, these changes may place uneven stress on the joint, increasing the likelihood of cartilage wear.
Physicians often refer to shoulder OA that follows a previous injury as post-traumatic OA. They commonly see this form of degeneration in individuals with a history of significant shoulder trauma.
Joint Misalignment
When the shoulder joint is not aligned correctly, movement may place uneven stress on specific areas of cartilage. This abnormal loading can accelerate localized wear and contribute to the gradual progression of OA.
Joint misalignment may stem from prior injuries, structural differences present at birth, or long-standing muscle imbalances that affect how the shoulder moves and stabilizes.
Genetic Factors
Genetics may play a role in increasing an individual’s likelihood of developing shoulder OA. Inherited traits can influence cartilage durability, joint shape, or how the body responds to inflammation, all of which may contribute to earlier or more advanced joint degeneration.
Although genetic factors alone may not cause shoulder OA, they can increase susceptibility when combined with other contributors such as joint injury, overuse, or age-related changes.
Obesity And Excess Weight
Excess body weight may contribute to shoulder OA through systemic effects rather than direct mechanical load. While the shoulder is not a weight-bearing joint, obesity has been associated with increased levels of inflammation throughout the body, which may accelerate cartilage deterioration.
Additionally, metabolic changes linked to excess body fat can impact joint health and may increase the risk of tissue damage over time.
Previous Surgery
A history of shoulder surgery, particularly procedures involving the rotator cuff, may increase the likelihood of developing or accelerating shoulder OA. Studies have shown that individuals with existing OA who undergo rotator cuff repair for large or complex tears may face a higher risk of re-injury and faster joint degeneration.
Even in cases without prior arthritis, osteoarthritic changes have been observed following surgery. Factors such as altered joint mechanics, inflammation during recovery, or incomplete tissue healing may contribute to this increased risk.
How Medical Professionals Diagnose This Condition
Diagnosing shoulder OA typically involves a combination of symptom review, physical evaluation, and imaging. These steps help confirm joint changes and rule out other causes.
- Physical examination: A physician may assess the range of motion, strength, and tenderness. The physician may also observe grinding or clicking sounds during shoulder movement.
- Imaging tests: Physicians commonly use X-rays to evaluate joint space or bone changes. MRI or CT scans may provide additional detail when necessary. Ultrasound can be used to assess soft tissue structures around the joint that are commonly associated with damage in shoulder OA.
Conventional Treatment Options
Conventional treatments for shoulder OA aim to help reduce symptoms and improve joint mobility. Treatment plans may vary based on joint condition and overall health.
- Heat and cold therapy: Heat may ease stiffness, while cold packs can help reduce swelling and discomfort after joint use.
- Physical therapy: Exercises may improve strength, flexibility, and shoulder stability to support joint function and reduce stress on affected areas.
- Slings and braces: Supportive devices may protect the joint during flare-ups or recovery, but extended use is generally not recommended.
- Surgery: Physicians typically consider surgical options when joint damage is advanced and conservative measures no longer provide relief.
- Shoulder arthroscopy: This is a less invasive procedure using small instruments to remove or repair damaged tissue or bone spurs from the joint.
- Shoulder replacement: Surgeons may replace damaged joint surfaces with artificial parts to help restore movement and reduce pain in severe cases.
Can Surgery Treat Shoulder Osteoarthritis?
Physicians may recommend surgery when shoulder OA symptoms become severe, and other treatments no longer provide relief. However, they must carefully evaluate long-term risks and benefits.
Shoulder replacement is a highly invasive procedure that involves removing the natural joint and implanting a prosthesis. Recovery can be lengthy and may involve physical restrictions and potential complications, such as infection, nerve injury, or implant loosening. Research shows that up to 40% of shoulder replacements in individuals under 55 may fail within 10 years.
While surgery may provide symptom relief in some advanced cases, it does not reverse joint degeneration and may carry added risks, especially for younger or more active individuals.
How The Regenexx Approach Provides A Non-Surgical Shoulder Care Option
For individuals with shoulder OA looking to avoid surgery or reduce reliance on pain medications, the Regenexx approach may offer a nonsurgical alternative. Procedures using Regenexx lab processes involve image-guided injections of the individual’s own bone marrow concentrate or platelet-based injectates to support joint function.
These procedures are designed to support the shoulder’s natural structure and movement. Unlike surgical interventions, the Regenexx approach does not involve joint removal or extended recovery periods. By using advanced imaging for precise placement, these procedures aim to support the body’s natural healing process and promote improved joint function.
Physicians may recommend this approach for individuals with mild to moderate cartilage loss or those looking to delay or avoid surgery. Procedures using Regenexx injectates may help maintain mobility, support long-term joint health, and reduce symptoms.
Explore Non-Surgical Strategies For Osteoarthritis Care
Shoulder OA can gradually affect mobility, strength, and daily function, but surgery is not the only option. Early recognition, informed decision-making, and nonsurgical strategies may support long-term joint health.
While conventional care may help manage symptoms, procedures using Regenexx lab processes offer a less invasive way to support joint function. These image-guided treatments aim to support mobility and reduce discomfort.
For individuals exploring alternatives to surgery, consulting with a physician experienced in interventional orthobiologics, such as physicians in the licensed Regenexx network, may help guide a care plan based on a thorough evaluation of joint conditions and personal goals.
Get started to see if you are a Regenexx candidate
To talk one-on-one with one of our team members about how the Regenexx approach may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.

Medically Reviewed By:
