Foraminal Stenosis: Everything You Need To Know

Medically Reviewed By:
Back and neck discomfort can significantly affect daily life, making even routine activities like walking, sitting, or sleeping difficult. These symptoms often stem from various underlying causes, including spine structure issues. Conditions that reduce the spaces in the spine can create nerve pressure, leading to pain, tingling, or weakness in different body parts.
Foraminal stenosis is one such condition, frequently linked to age-related changes in the spine. While it may sound complex, understanding its causes, symptoms, and treatment options can provide clarity and direction. This guide explores the essentials, offering insights and practical information to support individuals seeking relief.
Understanding The Foramen’s Role In Nerve Health
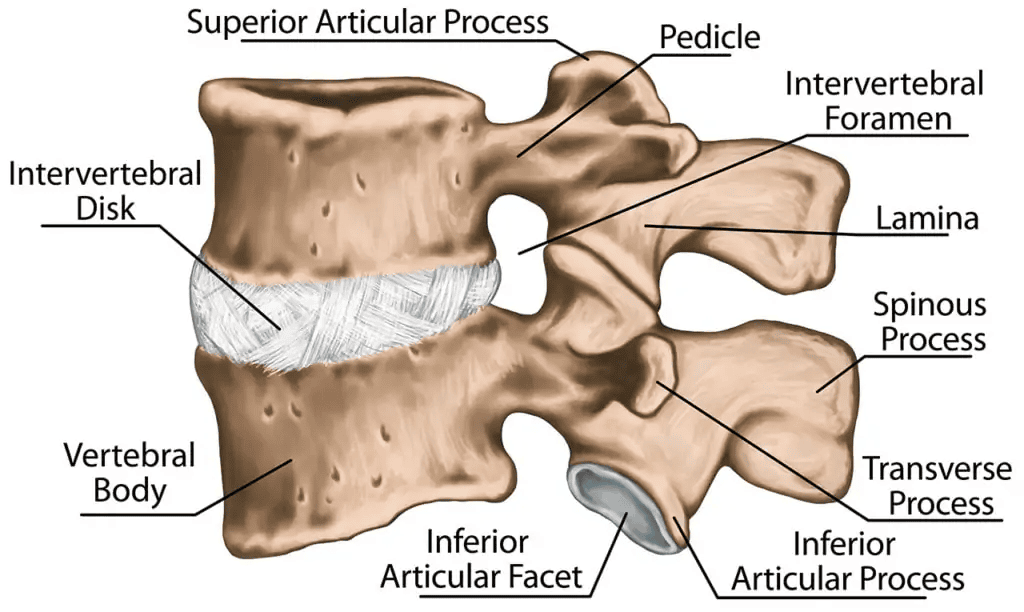
The foramen is a tunnel extending from the spinal canal through which spinal nerves at each level pass. In a healthy spine, these nerves move freely through the foramen, efficiently transmitting sensory signals between the body and the brain. However, when the spine is compromised, conditions such as foraminal stenosis can disrupt this flow of information.
Foraminal Stenosis Vs. Spinal Stenosis
Foraminal stenosis refers to the narrowing of the openings on the sides of the vertebrae, where spinal nerves exit the spinal canal to reach different body areas. In contrast, spinal stenosis involves the narrowing of the central spinal canal, the main passageway through which all spinal nerves travel. Both conditions may result from factors such as herniated discs, facet joint arthritis, or degenerative disc disease.
What Is Foraminal Stenosis?
Foraminal stenosis occurs when the foramen, small passageways between the vertebrae, become narrowed. These passageways allow nerves to exit the spinal column and travel to other body areas. When narrowing occurs, often due to factors such as bulging discs or arthritis in the spinal joints, it can compress the nerves.
This compression may lead to symptoms including muscle tightness, weakness, numbness, tingling, or pain. The location of foraminal stenosis within the spine determines where these symptoms are experienced.
- Cervical spine (neck): Nerve compression in this region can affect the shoulders, arms, hands, or fingers, resulting in symptoms such as tingling fingers or tightness in the biceps.
- Thoracic spine (mid back): Narrowing in this area may impact nerves serving the chest or abdomen, causing discomfort or radiating pain.
- Lumbar spine (lower back): Nerve compression in the lower back can cause numbness or tingling that radiates down the legs or into the feet.
Understanding the common locations of foraminal stenosis provides valuable insight into how and where the condition manifests, supporting accurate diagnosis and effective treatment.
Identifying The Triggers Of Narrowed Nerve Channels In The Spine
Foraminal stenosis often arises from structural changes and external factors affecting the spine’s delicate nerve pathways. These triggers can compress or irritate the nerves passing through the foramen, leading to symptoms commonly associated with the condition.
Recognizing the underlying causes is essential for determining effective treatments and managing the condition’s progression. Below are some of the most common factors contributing to narrowed nerve channels in the spine:
- Aging and degeneration: Natural wear and tear reduce spinal flexibility and narrow the nerve channels over time.
- Herniated discs: Bulging or ruptured discs can press against nerves, causing compression and pain.
- Thickened ligaments: With age, spinal ligaments may stiffen and thicken, reducing space within the spinal foramen.
- Spinal injuries: Trauma to the spine can result in misalignment or swelling that compresses nearby nerves.
Bone spurs: Abnormal bony growths, often linked to arthritis, can form and irritate nearby nerves by narrowing nerve channels. - Osteoarthritis: Cartilage degeneration from osteoarthritis can lead to inflammation and structural changes that reduce spinal space.
- Spondylolisthesis: Misaligned vertebrae that shift forward can compress nerve passages, leading to discomfort or pain.
Symptoms Of Foraminal Stenosis
Foraminal stenosis can cause various symptoms, depending on the location and severity of nerve compression. These symptoms often develop gradually but may worsen, affecting daily activities and overall quality of life. Common symptoms include:
- Localized Pain: Pain at the site of nerve compression, typically in the neck or lower back.
- Radiating Pain: Pain that follows the path of the affected nerve, extending to the arms, hands, legs, or feet.
- Numbness: Loss of sensation in areas supplied by the compressed nerve.
- Weakness: Muscle weakness in the arms, hands, legs, or feet, depending on the nerve involved.
- Limited Range Of Motion: Restricted movement in the neck or back due to pain or stiffness.
How Spinal Nerve Problems Are Diagnosed
Foraminal stenosis, also referred to as neural foraminal narrowing, is diagnosed through a combination of clinical evaluations and imaging techniques to confirm the condition:
- Physical examination: Physicians evaluate pain levels, reflexes, range of motion, and muscle strength to identify signs of nerve compression.
- Symptom assessment: Symptoms are reviewed to determine whether they align with those typically associated with foraminal stenosis, such as pain, numbness, or weakness.
- Diagnostic imaging: X-rays, MRI scans, and CT scans help detect the narrowing of the spaces between spinal bones. Nerve conduction studies may also be performed to assess the impact on nerve function.
Treatment Options Used For Foraminal Stenosis
Managing foraminal stenosis typically involves a variety of conventional treatments aimed at alleviating symptoms, improving mobility, and enhancing overall quality of life. Treatment plans are customized to the severity of the condition and the individual’s specific needs. Below are some commonly utilized approaches for addressing foraminal stenosis:
- Massage Therapy: Massage techniques relieve muscle tension, enhance circulation, and address discomfort associated with the condition.
- Physical Therapy: Strengthening and stretching exercises improve posture, reduce nerve pressure, and enhance mobility.
- Chiropractic Care: Gentle spinal adjustments may help reduce nerve compression and improve spinal alignment.
- Muscle Relaxants: These medications relieve muscle spasms and tension caused by nerve compression, but prolonged use may lead to drowsiness or dependency.
- Oral corticosteroids: Short-term corticosteroid use can reduce inflammation and alleviate nerve-related pain, but prolonged use may cause side effects.
- Epidural Steroid Injections: Targeted injections near the affected nerves provide relief from inflammation and pain, though repeated use carries some risks.
- Surgery: Surgical options, such as laminectomy, foraminotomy, or spinal fusion, aim to relieve nerve pressure by widening spinal openings or stabilizing the spine.
Surgery for foraminal stenosis can involve significant risks and long-term implications, particularly when spinal fusion is included. Spinal fusion can lead to adjacent segment disease (ASD), where the vertebrae above and below the fused section deteriorate over time. Due to this risk, patients are encouraged to seek multiple opinions before proceeding with invasive procedures.
Moreover, surgery is sometimes recommended based solely on MRI findings, however, imaging alone cannot reliably identify stenosis as the primary source of pain. Studies estimate that 21% of individuals with spinal narrowing on MRI have no symptoms at all.[1] Additionally, symptoms like back discomfort may not directly stem from stenosis and may instead present in other areas, such as the knee or shoulder.
Studies have shown that physical therapy can lead to long-term improvements in pain and function. One randomized-controlled trial found that patients receiving this multidisciplinary approach experienced significantly greater symptom relief than those without added physical therapy, with benefits lasting up to one year.[2]
Procedures using Regenexx platelet-rich plasma injectates, which use a patient’s own healing agents, may help support the body’s natural ability to heal and provide a less invasive option for managing foraminal stenosis. To better understand the potential complications associated with spinal fusion, see the video: Pain after Back Fusion.
Interventional Orthobiologic Options For Foraminal Stenosis
Physicians within the licensed Regenexx network provide less invasive procedures using Regenexx lab processing to address foraminal stenosis by promoting the body’s natural ability to heal. These procedures focus on managing inflammation and supporting spinal function without invasive surgery.
- Bone Marrow Concentrate (BMC) Injectates: Physicians in the network utilize bone marrow concentrate, which contains specialized cells from the patient’s own bone marrow to help support tissue health, manage inflammation, and address factors contributing to nerve compression in the spine.
- Platelet-Rich Plasma (PRP) Injectates: These deliver concentrated platelets to the affected area, which may help manage discomfort, support tissue health, and promote mobility.
- Platelet Lysate (PL) Injectates: These provide growth factors and anti-inflammatory proprietary methods to deliver rapid nerve pain relief and promote long-term recovery.
By leveraging the body’s natural ability to heal, these treatments can support improved quality of life while minimizing the risks and recovery time typically associated with traditional surgery.
Case Study: Choosing Nonsurgical Treatment For Foraminal Stenosis
Approximately two years ago, a patient began experiencing numbness in their right thumb, which later progressed to severe, sharp pain in the left shoulder blade. Initially believing the issue was shoulder-related, the patient received PRP injections into the shoulder.
However, the symptoms persisted. They also reported cramping, pain in the left biceps and forearm, and shoulder weakness during air travel.
Further evaluation revealed stiffness in the neck, prompting a cervical MRI that identified foraminal stenosis as the root cause of these symptoms. The patient explored non-surgical options before considering more invasive procedures. A physician in the licensed Regenexx network at the Colorado office administered high-dose platelet lysate injections into the foramen and around the affected nerve in the neck.
The results were encouraging. Although it required a few sessions, the patient’s symptoms reduced within weeks. Periodic maintenance injections now help support the condition under control, enabling the patients who opted for the Regenexx approach to maintain full functionality and engage in high-level physical activities without significant limitations.
This case underscores the potential of nonsurgical procedures using Regenexx injectates to help manage foraminal stenosis, supporting patients in preserving an active lifestyle.
*Disclaimer: Patient experiences vary, and no specific outcomes are guaranteed. For more information, visit our national patient registry.
Explore A Non-Surgical Approach Designed To Support Function With Lower Risk
Living with foraminal stenosis does not have to mean enduring constant discomfort or opting for invasive procedures. Physicians in the licensed Regenexx network provide non-surgical treatment options that may support the body’s natural healing processes to help manage symptoms and maintain mobility.
This approach focuses on addressing nerve compression, helping to alleviate discomfort, and supporting function, which may assist individuals in maintaining mobility and resume daily activities more easily.
If you are considering alternatives to surgery, non-surgical options may help support your comfort, recovery, and long-term well-being. With the right treatment plan, relief and an active lifestyle are within reach. Consult with a physician in the licensed Regenexx network to explore treatment options that align with your specific needs and goals.
To talk one-on-one with one of our team members about how Regenexx may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.

Medically Reviewed By:
