Spine Fusion-o-mania: Is there a Low back Surgery Success Rate Anymore?
ChooChin/Shutterstock
This past decade has seen an unprecedented explosion in spine fusions. In the meantime, from a clinician’s perspective, the low back surgery success rate has plummeted. This is because, like many things in medicine, this trend has been driven more by the high rates of insurance reimbursement for fusion than medical necessity. Take a gander at the graphs above from a recent Washington Post article. The number of fusion surgeries are up about 600-700% since 2000. The costs of the surgeries have about tripled due to the expensive hardware being implanted. In addition, about half of the surgeries are considered unnecessary. How did we get here?
Low back fusion is a surgery that’s meant to stabilize a grossly unstable spine. For example, someone gets into a catastrophic car crash and fractures their spine, which is incompatible with functioning as a normal human. In this patient, placing hardware to stabilize the spine is a God send as the patient doesn’t need to be immobilized in a bed for 2 months while they heal. However, at some point in the 1980s, a new concept emerged. Smart scientists had figured out that a degenerative spine goes through a period of instability (some extra motion). It was thought at the time (and is still believed in many spine surgery circles), that this type of degenerative instability would benefit from the same type of surgical stabilization with hardware (fusion). In addition, because all of the surgical codes for this surgery already offered generous reimbursement for a catastrophic surgery (with all of the complexity such a surgery may portend like operating on someone in the middle of night while they are barely alive), fusion for degenerative disc disease became a profitable venture.
Now first let me say that I have seen some degenerative disc patients who have tried all other options and are reasonable candidates for a fusion surgery. Having said that, these patients tend to be few and far between, in that many patients who end up with low back fusions today could have been helped in far less invasive ways.
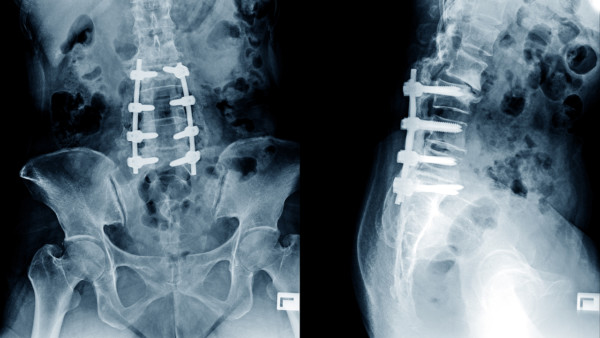
Why do the charts above exist? The article and a recent OIG investigation is about a recent trend that has supercharged the fusion market and dramatically increased fusion rates. I first noticed this trend locally about 10 years ago. A patient showed up to my office with their entire low back from the tailbone to the ribs fused. I was curious as this wasn’t done for scoliosis with rods, it was a surgery that was a massive extension of the 1-3 level fusions I had been seeing for years. These smaller fusions had gotten the reputation of often causing more problems than they fixed, as they severely overloaded the discs above and below the area fused, often causing the patient to need more and more surgery to eventually fuse those areas. Unlike the smaller fusions, this gentleman’s fusion was so massive that almost all of the important low back muscles had died off, leaving a Grand Canyon like ravine in his back. He was consulting with me because the surgery didn’t help and now his upper back was killing him (as all the forces were being transmitted there from the low back fusion).
As more and more of these ‘Mega-fusions” showed up at my office, I figured out the back story behind the massive surgeries. The company that had been creating these long fusion devices had a twist that made it hyper-competitive. The surgeons implanting the devices were partners in the company. In fact, this is discussed in the Washington Post article above and the topic has now been a subject of an OIG investigation. As these Physician Owned Device companies have proliferated (PODs), so has the fusion rate. What the Washington Post article doesn’t bring out is that many of these companies couldn’t enter into the competitive 1, 2, or 3 level fusion market because they were blocked by existing patents, so they went bigger. They submitted patents on these Mega-fusion devices because that’s the section of the market nobody else wanted. These devices fused 4, 5, 6, 7 or more levels. In essence, the entire low back could now be fused in a single surgery.
Why did no big surgical device company want the Mega-fusion device market? The wisdom gained during the 1990s was that anything more than a two level fusion was trouble. This is because the more levels you fuse, the more forces you have to wear out out the levels above and below. As a result, the general wisdom was fuse as little as possible.
When these new POD companies came on the scene, the Mega-fusion was born. These patients are generally harder to treat than prior surgical fusion failures. This is because the sheer number of levels virtually guaranteed that the structures above and below are constantly hammered. In addition, the ability to inject areas in the massive fusion site that may still be painful is technically difficult because of the hardware. Finally, trying to get a good image from an MRI anywhere in that same area is also very difficult, so often the doctor is flying blind.
The upshot? I’m glad POD companies are getting attention. Not because physicians shouldn’t be entrepreneurial, but because these POD device companies spawned one of the dumbest ideas in modern medical history-if fusing 3 levels is bad, fusing 6 must be great! In addition these POD companies have fueled an explosion in walking wounded, fused patients that we pain management doctors will be treating for a very long time.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.