ANOTHER Study Shows Fusion Is an Expensive Tip

Credit: Shutterstock
What if a very invasive spine procedure became common to treat degenerative disease despite a high complication rate and multiple studies showing it was ineffective? This would make little common sense, right? However, that’s what has happened with Lumbar Fusion. Now yet another new study shows it doesn’t work. Let’s dig in.
What Is DDD and Lumbar Fusion?
When the spine ages, it can become degenerative, which means that the discs lose height, the facet joints begin to get arthritic, the discs bulge, and the whole segment gets sloppy. The vertebrae can also begin to slip forward or backward on one another, which is called Degenerative Spondylolisthesis. One of the treatments suggested for this problem is Lumbar Fusion. In this procedure, the degenerative segments are bolted together with screws and rods.
Meet the Complications and ASD
Lumbar Fusion is very invasive and has a complication rate of about 20% (1,2). That means that about 1 in 5 will experience an infection, nerve damage, excessive blood loss, or another condition that requires medical care. That’s VERY HIGH for an orthopedic surgery procedure. For example, the complication rate after knee meniscus procedures is about 3-7% (3).
If you get past the initial complications, there’s another thing to be worried about called ASD. That’s Adjacent Segment Disease or the idea that when you fuse one area the adjacent segments get overloaded and wear out. How often does this happen? 2 years after a low back Fusion, 12% of patients will get ASD (4). From there, 2-4% of patients will get this problem every year after the fusion, so at 5-years later, up to 20% of patients will have ASD (5). To learn more, watch my video below:
The New Research
This new paper was published in the New England Journal of Medicine by Scandinavian authors who randomly assigned patients with Degenerative Spondylolisthesis (slippage of one vertebra on the other) to either Fusion or just Surgical Decompression (6). In the latter surgery, the holes for the nerves are opened by removing part of the disc and bone spurs. After two years, there was no benefit to adding a fusion.
Other Research Supporting this Conclusion
A systemic review has also been published which reviewed the results of 11 studies that compared Fusion to just Decompression surgery (7). After looking at the results of more than three thousand patients, there was no difference in results. Hence, there should be no argument that adding a Fusion for patients with severe DDD and Spondylolisthesis isn’t needed.
Why Is Fusion Still the Most Common Surgery for DDD with Spondylolisthesis?
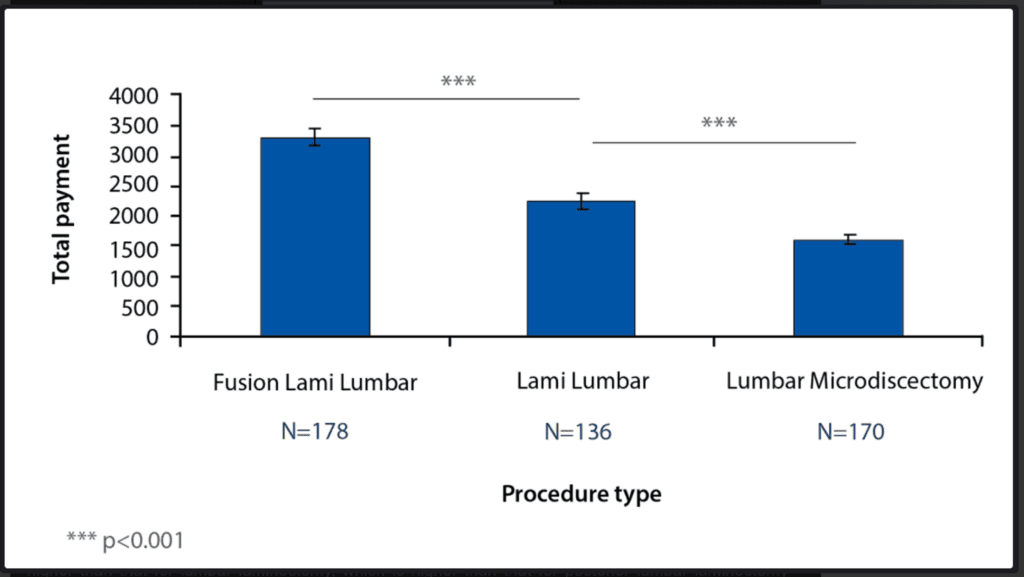
So if we know, beyond any doubt, that fusion for patients with Degenerative Spondylolisthesis doesn’t work any better than just Decompression, why is Fusion so common in these patients? There is only one reason: Fusion is a fantastic business plan. A device company can get a cheap 510K clearance from the FDA on a new Fusion device without any clinical trials. That device is then made in China, Vietnam, or India for tens of dollars and then sold through sales reps for thousands of dollars. Some of that generous profit can get kicked back to surgeons who are also incented by the insurance system to add Fusion. For example, this is from a recent study on how insurance payments (8):
Credit: The Orthopedic Journal at Harvard Medical School
The total payment for Fusion procedures is substantially more (far left) than just Decompression alone (middle and right). However, more time is taken for these procedures, which was not understood by the authors of the paper, as they argued that the payment per minute was better for the non-fusion procedures. All of that is true if you only look at professional services reimbursement by insurers. However, if you add in the additional surgery center reimbursement and fees paid to doctors by hardware companies, in my experience, the extra time is rewarded in other ways outside of professional reimbursement.
What if I Need Spine Surgery?
There is no doubt that there are some patients who can’t be treated any other way outside of spine surgery. The good news is that in our experience, about 80% of those who are told they need Fusion can be treated with orthobiologics. However, that other 20% will need some sort of surgical procedure. In that case, the evidence is clear, you don’t need a Fusion. Hence, you need to find a surgeon who will perform a Decompression surgery and skip the hardware.
The upshot? Lumbar Fusion is more of an expensive tip than an effective surgical procedure. It’s time that surgeons begin phasing it out for DDD. Will that happen? Likely not anytime soon due to the financial incentives built into the system. Hence, you need to be your own advocate armed with blogs like this one when you look for a surgical procedure that only involves Decompression.
_______________________________________
References:
(1) Mahesh B, Upendra B, Vijay S, Kumar GA, Reddy S. Complication rate during multilevel lumbar fusion in patients above 60 years. Indian J Orthop. 2017 Mar-Apr;51(2):139-146. doi: 10.4103/0019-5413.201704. PMID: 28400658; PMCID: PMC5361463.
(2) Hrabalek L, Adamus M, Gryga A, Wanek T, Tucek P. A comparison of complication rate between anterior and lateral approaches to the lumbar spine. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(1):127-32. doi: 10.5507/bp.2012.079. Epub 2012 Sep 5. PMID: 23073535.
(3) Salzler MJ, Lin A, Miller CD, Herold S, Irrgang JJ, Harner CD. Complications after arthroscopic knee surgery. Am J Sports Med. 2014 Feb;42(2):292-6. doi: 10.1177/0363546513510677. Epub 2013 Nov 27. PMID: 24284049.
(4) Zhong ZM1 Deviren V, Tay B, Burch S, Berven SH. Adjacent segment disease after instrumented fusion for adult lumbar spondylolisthesis: Incidence and risk factors. Clin Neurol Neurosurg. 2017 May;156:29-34. doi: 10.1016/j.clineuro.2017.02.020.
(5) Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM. Adjacent Segment Disease in the Cervical and Lumbar Spine. Clin Spine Surg. 2017 Apr;30(3):94-101. doi: 10.1097/BSD.0000000000000442.
(6) Austevoll IM, Hermansen E, Fagerland MW, Storheim K, Brox JI, Solberg T, Rekeland F, Franssen E, Weber C, Brisby H, Grundnes O, Algaard KRH, Böker T, Banitalebi H, Indrekvam K, Hellum C; NORDSTEN-DS Investigators. Decompression with or without Fusion in Degenerative Lumbar Spondylolisthesis. N Engl J Med. 2021 Aug 5;385(6):526-538. doi: 10.1056/NEJMoa2100990. PMID: 34347953.
(7) Dijkerman ML, Overdevest GM, Moojen WA, Vleggeert-Lankamp CLA. Decompression with or without concomitant fusion in lumbar stenosis due to degenerative spondylolisthesis: a systematic review. Eur Spine J. 2018 Jul;27(7):1629-1643. doi: 10.1007/s00586-017-5436-5. Epub 2018 Feb 5. PMID: 29404693.
(8) Wang R, et al. The Orthopedic Journal at Harvard Medical School. Volume 16 • June 2015. http://www.orthojournalhms.org/16/article31_36.html

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
