Back Surgery Concerns: Stone Age Spine Care…
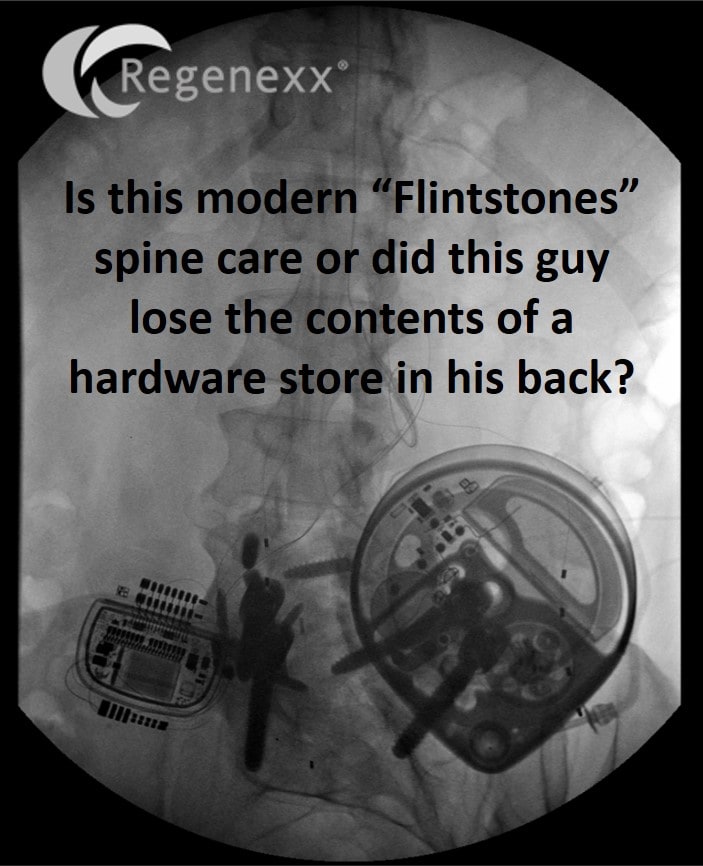
Back surgery concerns? As a clinician who sees patients almost every day, I get inspired by real events to write to help other patients. As a patient myself who has had serious back pain in my life, I know the desperation that can come with severe pain. So this morning I’d like to share an x-ray from a new patient yesterday because it represents what I call “Flintstones” spine care, or the stone age concept that all we need is a new piece of hardware to fix someone’s back.
First, this is the real unaltered x-ray. What happened? Believe it or not, all of this began with a herniated disc at L5-S1 about 8 years ago. That somehow led to a fusion at that level and fancy new “flexible stabilizer” being inserted at L4-L5. Regrettably that new doohickey broke, which then led to fusion surgery at L4-L5. While those surgeries helped some pains, they created new ones as well. So the spinal cord stimulator to the left (looks like a stop watch) was inserted with leads being placed above the fusion. When that didn’t work, the pain pump to the right was placed (looks like a bicycle lock). This machine (inserted under the skin), pumps pain meds directly onto his spinal cord. That initially didn’t work, but some recent medication changes that give the patient copious narcotics and muscle relaxers have resulted in better relief. How much narcotics in an oral equivalent? It’s as if the patient is carrying around a large bottle of narcotic pain pills and munching on these 24-7.
The amazing thing from my exam yesterday was that the pain pump was so efficient (combined with a fentanyl/Duragesic pain patch), that there was no way to tell where his pain was located. Obviously, if he turns all of this off he’s in serious pain with the narcotics only increasing his pain sensitization over time. That means that the longer he has narcotics dripping on his spinal cord, the higher his baseline pain off the narcotics will go.
The upshot? I thought this image would help some patients understand that fusion surgery is usually bad news. In fact, I brought it to my office manager who herniated the same disc about the same time, but because of where he works, has been getting regenerative spine treatments and never needed any surgery. Can we help this patient? Likely, but we’ll have to figure out how to find where he hurts first. In the meantime, please don’t let this be you…

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.