Can You Inject Low Back Discs Using Ultrasound?
©Regenexx
The efficacy of orthobiologics or the use of your body’s own platelets or stem cells to heal orthopedic problems depends on accurate placement. Meaning, injecting something like platelet-rich plasma into your body to heal a tendon requires that the platelets be placed precisely into the part of the tendon which has problems. To achieve that, high-level clinics use both real-time x-ray and ultrasound because each has its benefits and limitations. Let’s dive into why that is and review some new research on injecting discs with ultrasound.
Interventional Orthobiologics
What is interventional orthopedics or interventional orthobiologics? This is the precise injection of various substances capable of healing the joints, tendons, ligaments, spine, or muscles through the use of imaging guidance. To learn more, see my video below:
What Is Imaging Guidance?
Imagine that someone paints your front windshield black and asks you to drive down the street. Could you do it? Probably. Maybe you use the side windows and poke your head out every few feet and drive very slowly. But could you do it well? Nope. That’s the point of using imaging guidance when performing injections. To see where the needle is going.
If we use an example, let’s say we want to inject the low back disc. This is the structure that lives between the low back bones (vertebrae). The problem, of course, is that this is a very deep structure that we can’t feel or see from the surface. In addition, there are nerves in the way of a direct injection and if you’re off course because you can’t see, there are lungs and organs that can be inadvertently damaged. Hence, using something that can “see” the disc and the course of the needle from the surface of the skin down to that spot is critical.
Despite this need, we still see clinics that pretend to be injecting deep spinal structures that are impossible to access without imaging guidance through “blind” injections. These are usually non-physician owned clinics that hire a nurse or physician’s assistant to perform injections. Below is an animated gif that goes over what that looks like:
Fluoro vs. Ultrasound vs. Both
Fluoroscopy is the use of real-time x-rays to visualize bony structures and guide a needle to specific spots. Ultrasound uses sound waves and can visualize soft tissues better. However, ultrasound does a poor job of seeing deep structures that are encased in bone. Fluoroscopy shines in this area.
Fluoroscopy is dramatically more expensive than ultrasound. For example, a good “fluoro” unit costs about 120K and must be placed in a room with lead-lined walls. In addition, the machine usually requires an expensive radiology tech to run. On the other hand, a good ultrasound unit costs about 30-40K and needs no special room and can be run by the doctor performing the injection. Hence, we often see clinics that have only ultrasound not because it’s better, but because it’s cheaper.
In addition, the skill sets needed to operate these units are different. For example, fluoro guided spine injections can take years to master and require a knowledge of how specific injection imaging routines are set up. On the other hand, ultrasound-guided injections are usually more focused on the extremities with many physicians who learn these procedures not having much training in spine injections. Hence, it’s uncommon for a physician to possess both skill sets.
Why Both Is ALWAYS Better
Clinics that have both fluoro and ultrasound are almost always a cut above clinics using just one or the other. Why? Take a knee ACL injection. This can be done using ultrasound, but it can’t be done well as getting to all of the fibers of the ligament is just not possible. Hence, if a patient has an ACL tear that can be healed with bone marrow stem cells, you are shortchanging the patient by using ultrasound. However, the injection can be done very nicely with fluoroscopy as you can document that you injected bone marrow stem cells into all the parts of the ligament with issues. To learn more, see my video below:
On the other hand, injecting a torn rotator cuff with stem cells can only be poorly accomplished with fluoroscopy. Why? You just can’t see the damaged fibers of the tendon using x-ray. This is where ultrasound really shines. See my video below:
Spinal Injections: Fluoro vs Ultrasound
The set of physicians who have never learned fluoroscopy and spinal injections has been pushing towards using ultrasound for more and more of these procedures. Why? Fluoro machines are 3-4X as expensive as ultrasound machines. Hence, we’ve seen some physicians move facet injections and epidurals to ultrasound guidance. I’ve always thought this was a bit silly, as while you can perform these injections using ultrasound, you can’t visualize where your cells will go, as that part happens in areas where the ultrasound machine can’t see. However, using fluoroscopy, you can easily see where you cells will go.
As an example, when performing an epidural injection, which is around nerves, it’s common for the small changes in needle position to give optimal or suboptimal results. For example, a needle that is 1 mm too shallow will show a poor spread pattern of contrast (what we use to determine where our cells will go) and 1 mm deeper will show great spread around thew nerves you want to treat. However, using ultrasound, these two injections look the same. This is why I often say that while you can technically perform spinal injections using ultrasound, you just can’t do them well.
The New Research is Pushing this Ultrasound Spine Thing a Bit Far…
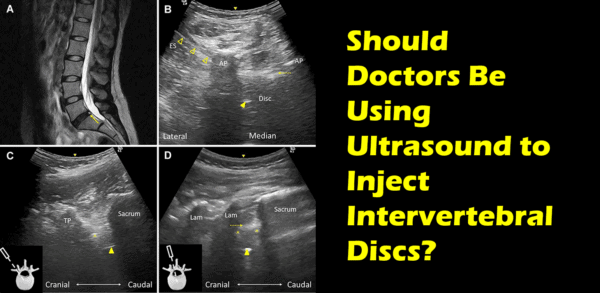
Now that you know that ultrasound isn’t often optimal for deep spinal injection, you’ see why I was flabbergasted by a recent paper out of China where they used ultrasound to inject a spinal disc (1). This is the deepest spinal structure you can inject and there are all sorts of reasons why a very specific trajectory of the needle is critical. Not the least of which is that the spinal nerve is close to where you need to place your needle and it’s obviously great if you can avoid damaging spinal nerves.
Basically, the Chinese physicians use a small window between the low back bones called the interlaminar space to bounce sound waves in and out of the disc. This is pretty hairy as if you move your ultrasound probe a millimeter or more in the wrong direction you’re flying blind. However, the physicians did prove that it was possible to inject the disc using ultrasound. See their video below:
Again, as I have written above, while the fact that someone has shown you can do this doesn’t mean you can do it well reliably. For example, when injecting discs, it’s often very difficult to get the cells to the right spot in the disc. Using fluoro, this means that we often need to adjust the needle to get the contrast to flow to the right spot. This ability again is lost with ultrasound.
The upshot? As you can see, a clinic with both fluoro and ultrasound can use the best of both technologies to get cells exactly where you need them. While you can use ultrasound to place cells and in some applications that’s the better way to go, in some instances like the spine, while it can be done, it can’t be done well. In my opinion, while using ultrasound to inject a disc is clearly possible, it’s likely not the best tool for the job!
_________________________________________
References:
(1) Wu TJ, Hung CY, Lee CW, Lam S, Clark TB, Chang KV. Ultrasound-Guided Lumbar Intradiscal Injection for Discogenic Pain: Technical Innovation and Presentation of Two Cases. J Pain Res. 2020;13:1103-1107 https://doi.org/10.2147/JPR.S253047

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.