Should We Be Cementing Fractured Back Bones?
This is an interesting blog for me to write. On the one hand, I have colleagues that perform vertebroplasty to treat thoracic compression fractures and say that it can be amazing, older people get rolled in and walk out. On the other hand, the idea of bone cement, an artificial substance to glue bones back together has never made much sense, and I’ve seen serious complications from its use. So rather than taking a side in this one, I’ll just report what the research just uncovered.
Vertebroplasty: Cementing Fractured Back Bones
Verterbroplasty is a percutaneous procedure in which a thick needle (called a trocar) is inserted deep into a fractured vertebra (backbone) and through the needle, bone cement is injected into the bone. Once injected, the cement spreads and hardens. The idea is primarily to reduce pain while also stabilizing the fractured bone. Vertebroplasty is commonly done when osteoporosis results in compression fractures in the vertebrae, but it can be done for other conditions or injuries that might cause a compression fracture in the back bone, such as cancer.
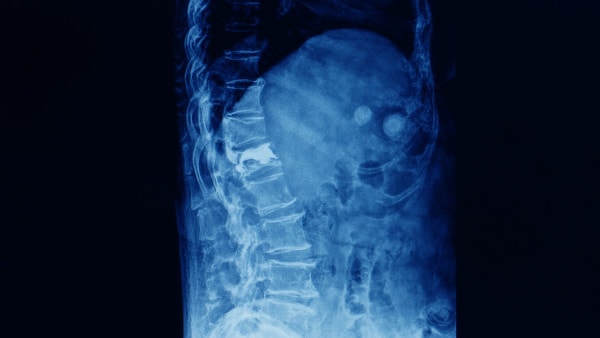
Compression fracture of the spine treated with vertebroplasty. Yok_onepiece/Shutterstock
Another procedure that might be recommend for compression fractures in vertebrae is a kyphoplasty. When talking about cementing fractured back bones, you need to be familiar with this term as well because a kyphoplasty is basically a vertebroplasty with a balloon inserted and inflated to raise the fractured bone space first. Once the space is raised, cement is then injected into the bone, just like with the verterbroplasty.
Today’s feature study focuses on compression fractures due to osteoporosis and how they respond specifically to vertebroplasty.
What Is Osteoporosis?
Osteoporosis is a bone disease that occurs when bone density decreases and bones become fragile. They can become so fragile that even a mild fall, which wouldn’t damage normal bone, can severely fracture osteoporotic bones. Osteoporosis and compression fractures of the vertebrae are most common in post-menopausal aging women whose bones have become weak after many years of inactivity and hormonal imbalances. So how does verterbroplasty fare when treating osteoporotic compression fractures in the back? Let’s review the study.
Vertebroplasty No Better than Fake Surgery for Osteoporotic Back Bone Fracture Pain?
The purpose of the new study was to determine if verterbroplasty relieved pain better than a fake surgery in patients with compression fractures due to osteoporosis. The double-blind randomized controlled trial consisted of 180 patients who had compression fractures in one, two, or three vertebrae. About half underwent vertebroplasty (cement injections into their back bones) while the other half (the control group) received a sham procedure. “Double-blind” means, to eliminate bias, during the study neither the patients nor the researchers knew which patients were placed in which group. The mean pain score for the vertebroplasty group prior to the procedure was 7.7 out of 10. The control group mean score was 7.9.
The results? While the vertebroplasty group did experience significant pain relief, so did the sham surgery group. One month after surgery, the verterbroplasty group mean pain score was 3.3 compared to the control group at 3.7. At 12 months scores were 2.7 and 3.2 respectively. Researchers concluded that vertebroplasty (cementing the fractured back bones) relieved pain no better than the sham procedure, and therefore they did not support it as a treatment for compression fractures in the vertebrae due to osteoporosis.
What to Do and Not to Do for Osteoporosis
The ideal solution is to stay proactive about your musculoskeletal health throughout life to minimize your risk of developing compression fractures in your back due to osteoporosis. Staying active, eating healthy food, and keeping your hormones in balance will provide a good foundation. In addition bone-nurturing supplements can provide extra support. Studies have suggested curcumin suppresses oxidative stress and is beneficial for building bone (increasing bone-forming cells) and alleviating bone density loss.
Unfortunately, osteoporosis may already be a disease you are struggling with, and if so, there are a few things you shouldn’t do. First, Prolia, a drug prescribed for osteoporosis, has been linked to rebound fractures once the drug is stopped, suggesting that it may actually damage mesenchymal stem cell, or the cells that make bone. So if you are already taking this drug, consult with your physician if you wish to stop taking the drug. Second, don’t fall prey to vibration plate therapy, which manufacturers claim will increase your bone mass. Many studies have found these machines, costing thousands of dollars, do no such thing.
Another bad move for attempting to treat osteporosis is IV fat stem cell treatments. If someone suggests this treatment for osteoporosis, this is a scam. While bone marrow stem cells have the appropriate tissue properties for treating bone, fat stem cells are from a different tissue and do not have the same level of bone-building advantages. In addition, injecting stem cells intravenously (IV) results in the majority of the stem cells becoming trapped in the lungs; very few pass out of the lungs and end up in the bone.
The upshot? I’m not sure what to make of this one. As I said, I have colleagues who report that patients have significant pain relief with vertebroplasty. On the other hand, in this study, the placebo group also reported remarkable pain relief, so is what they’re witnessing a placebo effect? Unsure. In the meantime, as I’ve said, I’m not a fan of bone cement, so I’ll continue to avoid performing this procedure.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.