Headaches and Neck Pain or Cervicogenic Headache
Headaches and neck pain are often linked but also often ignored by many physicians. This is called cervicogenic headache. What causes this problem and how can it be helped? Let’s dig in.
Why Does My Neck Hurt and Give Me a Headache?
As you develop in the womb, your head and upper neck develop together, forever linking pain in one to the other (1). Hence, the upper neck joints, discs, muscles, and nerves can cause pain that goes into your head (headaches). When this happens it’s called cervicogenic headache. Figuring out which of these is causing the pain and why is key to getting rid of these headaches.
What Are the Things that Cause Cervicogenic Headache?
There are a number of damaged or injured structures in your neck that may be causing a cervicogenic headache:
- Upper neck facet joints
- Irritated occipital nerves
- Pinched upper neck spinal nerves
- Upper neck discs
- Muscle trigger points
- Damaged upper neck ligaments
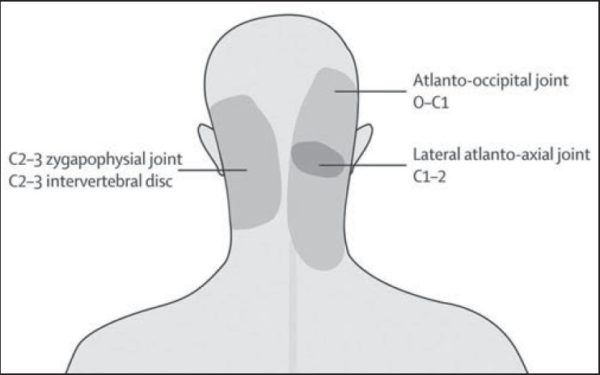
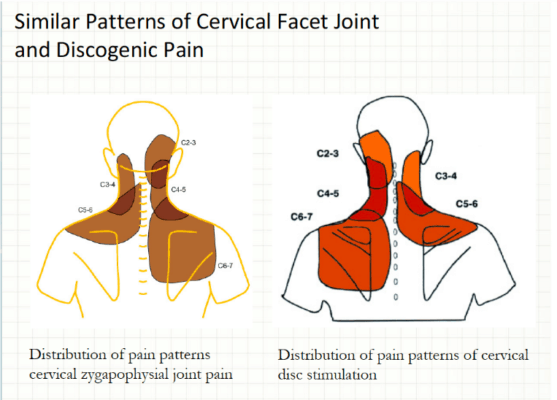
There are two facet joints in the neck at the back of each spinal level. They are about the size of your small finger joints and can be injured through trauma or become arthritic like any other joint. The C0-C3 joints refer pain to the head (see the diagram) (2). These joints can be injected using fluoroscopy to guide the needle into the joint. Each specific joint can be numbed to see if this reduces the headache pain. These are commonly called facet blocks or injections. The nerve that takes the pain from the C2-C3 joint which is called the medial branch can also be numbed, which is called a medial branch block.
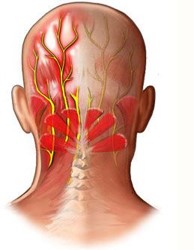
There are a number of nerves at the back of the head and these are often called occipital nerves. They are usually named the third, greater, and lesser occipital nerves. The third occipital nerve comes out close to the midline, the greater comes out on the side of the upper trap, and the lesser comes out behind where the sternocleidomastoid muscle inserts into the head. When irritated by the surrounding muscles or injured, they can refer pain to specific places in the head such as behind the eye and the back of the head (3). To see if these nerves are causing cervicogenic headaches, numbing injections using ultrasound guidance can be performed to determine if they take away the headache.
The C1-C3 spinal nerves also can cause cervicogenic headaches. They exit the spine on the side and the C3 nerve can get pinched if there is a bulging disc at C2-C3. The higher spinal nerve can be irritated by bone spurs and/or if the upper neck is unstable (craniocervical instability). The nerves supply different parts of the head, so they refer pain to different spots (4). To make this diagnosis, the spinal nerves need to be numbed using a selective nerve root block to see if this takes away the headache.
The neck discs act as shock absorbers between the neck bones. They can become painful all by themselves, a condition known as discogenic pain. The C2-C3 disc can refer pain to the back of the head. The only way to diagnose this is a discogram, a procedure where dye is injected into the disc using x-ray guidance and then the disc pressured to see if causes cervicogenic headaches (5).
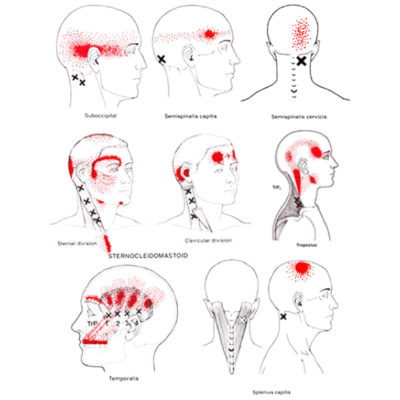
Muscle trigger points can also cause cervicogenic headaches. There are many muscles in your neck including those that stabilize the head on the neck. Interestingly, research has shown that one in particular, called the rectus capitus posterior minor, is jacked directly into the covering of your brain (6). Hence, when it gets problems and becomes tight, this can cause a dural headache. Other muscles have also been shown to have trigger points (areas that are tight and weak and feel like knots) that can also refer pain to your head (7). See the diagram here.
Finally, the neck ligaments help to hold your head on and they can cause cervicogenic headaches as well. For example, the Ventrodural Ligament (VDL) lives in the back of the neck and is also jacked into the dura just like the RCPM muscle above (8). In addition, when the alar, transverse, and/or accessory ligaments are lax or damaged, they can cause craniocervical instability which can lead to cervicogenic headaches (9).
What Does a Cervicogenic Headache Feel Like?
This is a headache often in the back of the head, but also in the forehead or behind the eye that is associated with neck pain. The neck doesn’t always have to hurt when the headache is present, but there is a clear connection between the neck issues and the headache. The upper neck is usually the area that has the most tenderness.
How Do You Treat a Cervicogenic Headache?
The treatment depends on what’s causing the problem. For example, facet pain can be treated by injecting the facet joints using x-ray guidance (11). Platelet-rich plasma can help with facet pain as well (10). Radiofrequency ablation can also help, but is temporary and destroys the nerve that takes the pain from the joint and can have side effects.
The occipital nerve pain and spinal nerves can be treated with nerve blocks or epidural injections (6). Neck disc pain can be treated with fusion surgery, but that risks causing more pain and arthritis above and below the fused levels (13). Another way to treat disc pain is via platelet-rich plasma injection into the discs (12).
Muscle trigger points can be treated with physical therapy or trigger point injections/dry needling (14). Damaged neck ligaments can be treated with prolotherapy or bone marrow concentrate which has shown promise in treating other ligaments (15, 16). Fusion surgery is also possible, but in the upper neck, this is a complication laden procedure (17).
Can a Chiropractor Help with Cervicogenic Headaches?
We have seen good results with chiropractic treatment of cervicogenic headache. Upper cervical specific chiropractors like those trained in the NUCCA or AO technique specialize in this area.
Can Cervicogenic Headaches Cause Migraines?
Migraines are a type of headache that is caused by vascular problems in the brain often associated with nausea, vomiting, and sensitivity to light and sound. Cervicogenic headaches can trigger migraine headaches. However, migraine headaches are often confused with cervicogenic headaches (18).
What Does a Pinched Nerve Headache Feel Like?
As discussed above, upper neck pinched nerves (C2 and/or C3) can cause cervicogenic headaches (19). This can be burning, electrical, or nervy type pain in the back or top of the head. There should be evidence on MRI of a nerve being pinched by a disc bulge or bone spur at these levels. If the spinal nerves are treated with an epidural, this pain will go away, nailing the diagnosis.
Is Cervicogenic Headache Serious?
For the most part no, if the headache is coming from the neck, it’s not serious. One problem that can be serious that causes cervicogenic headache is CCI (craniocervical instability) (20). This means that the ligaments that hold the head on are damaged or loose. This problem is more common in patients with loose ligaments like Ehlers-Danlos Syndrome.
The upshot? Cervicogenic headache is quite real, but the key to fixing it is finding out what’s causing the problem. Like everything in medicine, an exact diagnosis is tied to the right treatment.
________________________________________
References:
(1) Fredriksen TA, Antonaci F, Sjaastad O. Cervicogenic headache: too important to be left un-diagnosed. J Headache Pain. 2015;16:6. doi: 10.1186/1129-2377-16-6
(2) Kirpalani D1, Mitra R. Cervical facet joint dysfunction: a review. Arch Phys Med Rehabil. 2008 Apr;89(4):770-4. doi: 10.1016/j.apmr.2007.11.028.
(3) Gupta R, Fisher K, Pyati S. Chronic Headache: a Review of Interventional Treatment Strategies in Headache Management. Curr Pain Headache Rep. 2019 Jul 29;23(9):68. doi: 10.1007/s11916-019-0806-9.
(4) Bogduk N. The clinical anatomy of the cervical dorsal rami. Spine (Phila Pa 1976). 1982 Jul-Aug;7(4):319-30.DOI: 10.1097/00007632-198207000-00001
(5) Manchikanti L, Dunbar EE, Wargo BW, Shah RV, Derby R, Cohen SP. Systematic review of cervical discography as a diagnostic test for chronic spinal pain. Pain Physician. 2009 Mar-Apr;12(2):305-21. https://www.ncbi.nlm.nih.gov/pubmed/19305482
(6) Gupta R, Fisher K, Pyati S. Chronic Headache: a Review of Interventional Treatment Strategies in Headache Management. Curr Pain Headache Rep. 2019 Jul 29;23(9):68. doi: 10.1007/s11916-019-0806-9.
(7) Sedighi A, Nakhostin Ansari N, Naghdi S. Comparison of acute effects of superficial and deep dry needling into trigger points of suboccipital and upper trapezius muscles in patients with cervicogenic headache. J Bodyw Mov Ther. 2017 Oct;21(4):810-814. doi: 10.1016/j.jbmt.2017.01.002.
(8) Zheng N, Yuan XY, Li YF, et al. Definition of the to be named ligament and vertebrodural ligament and their possible effects on the circulation of CSF. PLoS One. 2014;9(8):e103451. Published 2014 Aug 1. doi: 10.1371/journal.pone.0103451
(9) Henderson FC (2016) Cranio-cervical Instability in Patients with Hypermobility Connective Disorders. J Spine 5:299. doi: 10.4172/2165-7939.1000299
(10) Wu J, Zhou J, Liu C, Zhang J, Xiong W, Lv Y, Liu R, Wang R, Du Z, Zhang G, Liu Q. A Prospective Study Comparing Platelet-Rich Plasma and Local Anesthetic (LA)/Corticosteroid in Intra-Articular Injection for the Treatment of Lumbar Facet Joint Syndrome. Pain Pract. 2017 Sep;17(7):914-924. doi: 10.1111/papr.12544.
(11) Manchikanti L, Hirsch JA, Kaye AD, Boswell MV. Cervical zygapophysial (facet) joint pain: effectiveness of interventional management strategies. Postgrad Med. 2016 Jan;128(1):54-68. doi: 10.1080/00325481.2016.1105092.
(12) Monfett M, Harrison J, Boachie-Adjei K, Lutz G. Intradiscal platelet-rich plasma (PRP) injections for discogenic low back pain: an update. Int Orthop. 2016 Jun;40(6):1321-8. doi: –10.1007/s00264-016-31783.
(13) Virk SS, Niedermeier S, Yu E, Khan SN. Adjacent segment disease. Orthopedics. 2014 Aug;37(8):547-55. doi: 10.3928/01477447-20140728-08.
(14) France S, Bown J, Nowosilskyj M, Mott M, Rand S, Walters J. Evidence for the use of dry needling and physiotherapy in the management of cervicogenic or tension-type headache: a systematic review. Cephalalgia. 2014 Oct;34(12):994-1003. doi: 10.1177/0333102414523847.
(15) Centeno CJ1, Elliott J, Elkins WL, Freeman M. Fluoroscopically guided cervical prolotherapy for instability with blinded pre and post radiographic reading. Pain Physician. 2005 Jan;8(1):67-72. https://www.ncbi.nlm.nih.gov/pubmed/16850045
(16) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246. Published 2018 Sep 3. doi: 10.1186/s12967-018-1623-3
(17) Myers KD, Lindley EM, Burger EL, Patel VV. C1-C2 fusion: postoperative C2 nerve impingement-is it a problem?. Evid Based Spine Care J. 2012;3(1):53–56. doi: 10.1055/s-0031-1298601
(18) Schwedt TJ, Chong CD, Peplinski J, Ross K, Berisha V. Persistent post-traumatic headache vs. migraine: an MRI study demonstrating differences in brain structure. J Headache Pain. 2017;18(1):87. Published 2017 Aug 22. doi: 10.1186/s10194-017-0796-0
(19) Biondi DM. Cervicogenic Headache: A Review of Diagnostic and Treatment Strategies. J Am Osteopath Assoc 2005;105(4_suppl):16S–22S. https://jaoa.org/article.aspx?articleid=2093083
(20) Henderson FC (2016) Cranio-cervical Instability in Patients with Hypermobility Connective Disorders. J Spine 5:299. doi: 10.4172/2165-7939.1000299

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
