Should You Get Gastrocnemius Recession Surgery?
On this page:
- The gastrocnemius muscle
- Gastrocnemius recession surgery
- Open vs. endoscopic surgery
- Gastrocnemius recession recovery
- Gastroc recession success rate
- Complications of the procedure
- Alternatives to gastroc recession
What is gastrocnemius recession surgery? This procedure has become popular for quite a few things, including the treatment of a tight calf, Achilles pain, or plantar fasciitis. Let’s dig in.
The Gastrocnemius Muscle
The gastrocnemius (aka gastroc or calf muscle) is at the back of the leg and connects the heel to the calf to the knee. Meaning, it’s a two-joint muscle that helps to flex the foot downward and extend the knee if the foot is fixed. Its nerve supply comes from the lower part of the low back (S1 and S2). These nerves tell the muscle what to do and how to contract.
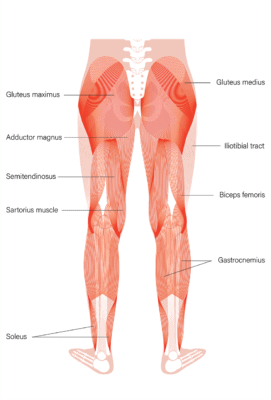
Pikovit/Shutterstock
Gastrocnemius Recession Surgery
Gastrocnemius recession (aka Strayer procedure) is a surgery where the doctor cuts the gastroc tendon and lengthens the muscle and tendon (1). The procedure is usually performed to treat chronic tightness in the calf muscle.
Since this muscle attaches to the Achilles tendon, chronic Achilles pain can also be treated this way. Finally, the Achilles tendon has fibers that also travel to the plantar fascia at the bottom of the foot. So the procedure has also been used to treat plantar fasciitis.
Open vs. Endoscopic Surgery
Open surgery is when the doctor makes a traditional long incision and then cuts the tendon to lengthen it. Endoscopic surgery involves a smaller incision where a scope is inserted and the tendon is cut through that smaller portal. Both procedures seem to work about the same (5).
Gastrocnemius Recession Recovery
Expect the first few days to be painful and to require narcotic pain medications. You’ll be in a boot or similar for several months while the tendon heals properly. You can usually begin touch down weight bearing (touching your foot to the floor) about at 6-12 weeks. After gastrocnemius recession surgery, return to full activity takes on average about 7 months (2).
Gastroc Recession Success Rate
Regrettably, we don’t have gold-standard randomized controlled trials comparing the procedure to a sham operation to show whether gastrocnemius recession is effective (1). For use in Achilles tendon pain, lower-level evidence exists showing some efficacy. However, all of the research published supporting use in other problems is problematic.
Complications of the Procedure
In particular, about 9% of patients never return to their pre-surgery level of activity (2). Complications happen in about 6% of patients who undergo the surgery and can include postoperative infection, non-healing wounds, nerve problems, decreased muscle strength, scar problems, or the inability to walk normally (3).
Endoscopic surgery seems to be associated with fewer complications than open surgery in one study and about the same in another (4,5).
Alternatives to Gastroc Recession
Cutting and then lengthening a tendon is a big surgery. Given that this procedure is increasingly performed to treat a tight calf muscle, Achilles tendinitis, or plantar fasciitis, it’s critical to understand why these problems happen and that there are non-surgical treatment alternatives for all of these issues:
- Tight calf-The S1 nerve in the low back tells the calf muscle how tight or loose it should be. When it’s irritated, the calf can become chronically tight. Hence, the first-line treatment for a tight calf is physical therapy and if that fails, a precise x-ray guided epidural injection around that irritated S1 nerve. In most patients, this takes the problem away. There can also be a disc bulge her pressing on the nerve or too much motion at the L5-S1 back level (degenerative or congenital spondylolisthesis) which can lead to the irritated nerve. Obviously the focus here is fixing the back which fixes the calf. This can usually be done non-surgically.
- Achilles Tendinitis-This is chronic degeneration of the tendon that attaches the calf muscle to the heel. Platelet-rich plasma injections performed using ultrasound guidance will usually get rid of this problem (6).
- Plantar Fasciitis-The plantar fascia is a tight band at the bottom of the foot that extends from the heel forward and supports the arch (7). This fascial band can also become degenerated and again, platelet-rich plasma injections can usually help this problem as well.
As you can see, there are multiple non-surgical ways to deal with the problems that often lead to gastrocnemius recession surgery. In my experience, when treating a tight calf, the Achilles or plantar fascia, oftentimes treating the low back S1 nerve is also required to make the problem resolve. Hence, a gastroc surgery should be your very last option after trying these much less invasive therapies.
The upshot? Gastrocnemius recession is a big surgery that usually doesn’t need to be done as these days there are much less invasive options. If you do need this surgery, make sure you understand the risks and benefits.
__________________________________________
References
(1) Cychosz CC, Phisitkul P, Belatti DA, Glazebrook MA, DiGiovanni CW. Gastrocnemius recession for foot and ankle conditions in adults: Evidence-based recommendations. Foot Ankle Surg. 2015;21(2):77-85. doi:10.1016/j.fas.2015.02.001
(2) Tang Qian Ying C, Lai Wei Hong S, Lee BH, Thevendran G. Return to physical activity after gastrocnemius recession. World J Orthop. 2016;7(11):746-751. Published 2016 Nov 18. doi:10.5312/wjo.v7.i11.746
(3) Rush SM, Ford LA, Hamilton GA. Morbidity associated with high gastrocnemius recession: retrospective review of 126 cases. J Foot Ankle Surg. 2006;45(3):156-160. doi:10.1053/j.jfas.2006.02.006
(4) Harris RC 3rd, Strannigan KL, Piraino J. Comparison of the Complication Incidence in Open Versus Endoscopic Gastrocnemius Recession: A Retrospective Medical Record Review. J Foot Ankle Surg. 2018;57(4):747-752. doi:10.1053/j.jfas.2018.01.009
(5) Phinit P et al. Outcomes of Open and Endoscopic Gastrocnemius and Gastrosoleus Lengthening: A Comparative Study. Arthro: J Arthro Rel Surg. 2015;31(6):e19. doi:10.1016/j.arthro.2015.04.051
(6) Liu CJ, Yu KL, Bai JB, Tian DH, Liu GL. Platelet-rich plasma injection for the treatment of chronic Achilles tendinopathy: A meta-analysis. Medicine (Baltimore). 2019;98(16):e15278. doi:10.1097/MD.0000000000015278
(7) Peerbooms JC, Lodder P, den Oudsten BL, Doorgeest K, Schuller HM, Gosens T. Positive Effect of Platelet-Rich Plasma on Pain in Plantar Fasciitis: A Double-Blind Multicenter Randomized Controlled Trial. Am J Sports Med. 2019;47(13):3238-3246. doi:10.1177/0363546519877181

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.