How Quickly Do You Resolve Inflammation?
Credit: Shutterstock
Inflammation is a complex subject. On the one hand, it’s how we heal and on the other hand, it’s increasingly how many of us die. So today we’ll explore the concept of resolving inflammation after a procedure and what that tells us about overall health and metabolic problems. Let’s dig in.
What Is Inflammation?
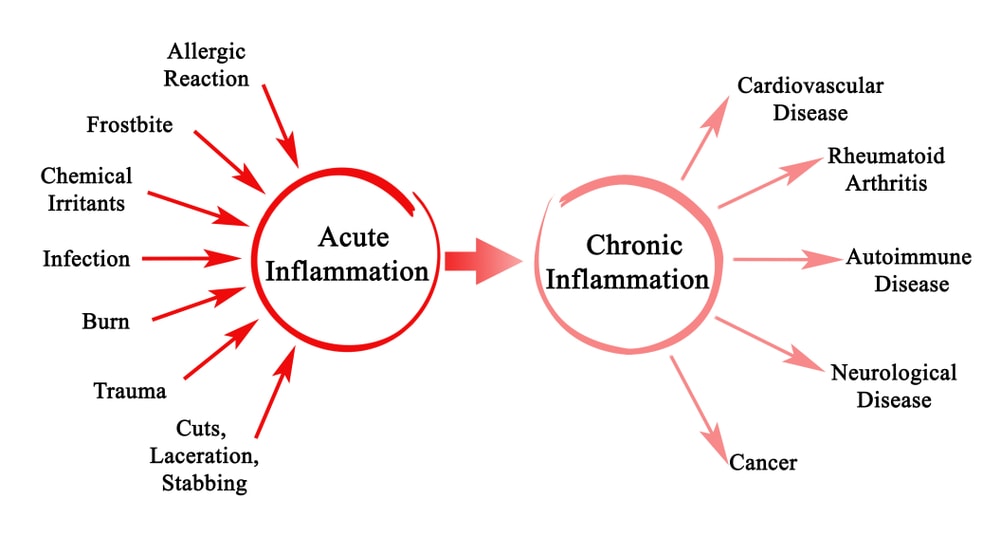
When we get injured, our body sends loads of cells to help repair the damage. Those cells cause swelling which is called acute inflammation. This is how we heal. The problems start when the area doesn’t heal and the body keeps throwing these cells at the problem, that’s called chronic inflammation. That type of inflammation is increasingly how many in industrialized nations die. It’s bad for blood vessels, joints, the heart, the brain, you name it.
Resolving Inflammation
One of the more impressive things as a doctor to observe is how quickly young people heal. For example, I’ve injected platelet-rich plasma into countless under 20-year-olds who are back to full activity by the time we older folks are just getting the swelling to calm down. Part of why this happens is the speed at which they resolve inflammation. Meaning for a day or two the area is inflamed and then the swelling leaves as quickly as it appears. That’s called resolving inflammation (1).
For us older folks (over the hill people over the age of 35 or so), inflammation tends to resolve more slowly. In some people, it doesn’t resolve at all and becomes a chronic problem.
Blocking vs Resolving
It’s important to note here the big differences between blocking inflammation versus resolving it. For example, an NSAID drug like Motrin prevents the inflammatory cascade from getting rolling. This is an issue because inflammation is how we heal, so we want it early on in the healing process, and blocking it can cause problems. Resolving inflammation means that the repair job is done or as done as it can be and then the body recognizes that it’s time to flip the inflammation “off switch”.
The Nitty Gritty
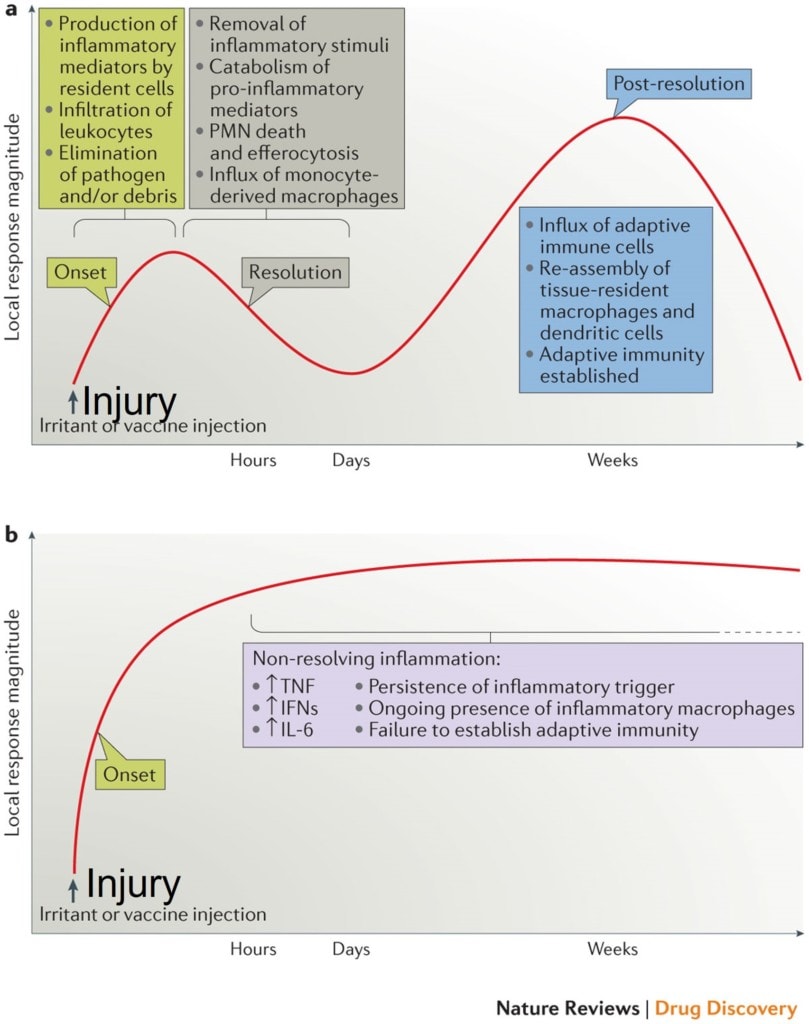
Credit: Nature
Above are slides provided by the journal Nature from an article I’ve cited (1). While this is a mish-mash of complex medical and research terms if you look at the graph above, there are three phases of normal inflammation. In the “Onset” phase the cells and swelling come into the area. In the “Resolution” phase the repair job is done and the body signals that the inflammatory cells can leave. In the third phase called “Post Resolution”, the body resets the local cell mix to what it was before the damage.
You get one bite at this healing “apple”. If things heal completely, you move on. If they don’t, orthobiologic injections like platelet-rich plasma or bone marrow concentrate can give the patient another bite at this apple. In other words, we can kick off the whole cycle again and ramp it up.
Now, look at the graph below. We have the onset phase, but the signal to resolve the inflammation is never sent. Instead, inflammatory chemicals in the body keep the inflammatory fire stoked. In fact, I often explain this to patients using a forest fire analogy. In a young, damp, and healthy forest, if you start a campfire and even if you walk away, there’s not much that’s flammable around the fire, so the fire eventually goes out on its own. That’s our first example of normal inflammation. On the other hand, in a dry forest with no water, that same campfire can cause a huge fire and burn the whole area down. That’s like our second example above of someone who has lots of inflammatory chemicals in their system.
Inflammation and Metabolic Syndrome
Metabolic syndrome means being overweight, having high triglycerides, insulin resistance, and high blood pressure (2). It’s the most common affliction of the first world where we eat too much, consume sugary garbage, and exercise too little. That means that the chemicals above that cause chronic inflammation exist in higher levels in the bloodstream. So people with metabolic syndrome tend to have a poor ability to resolve inflammation.
How Quickly Can You Resolve Inflammation?
As physicians using regenerative medicine products to help patients heal damaged orthopedic tissues, we see this resolving inflammation orchestra every day. Meaning, our older, thin, and fit patients tend to have only short-term inflammatory responses to these injections, much more similar to our younger patients. On the other hand, our heavier patients with metabolic syndrome tend to either take a long time to either resolve inflammation or transit into chronic inflammation.
For example, I reviewed MRIs this week on a patient who clearly has metabolic syndrome and has had chronic inflammation in her knee for years. She literally walks around with 30 cc of extra fluid in each joint. This was made worse on one side by getting a meniscus surgery in 2015. That caused her knee to swell for a solid year. Is this normal? NO! While I’m no fan of meniscus surgeries, having a year of swelling after that type of procedure usually means that there is a distinct issue resolving inflammation. In fact, she recently put herself on an anti-inflammatory diet and her knees feel better despite her arthritis.
Another example that you should be focusing on is your response to the procedures we offer. Meaning, if I or another Regenexx doctor injects PRP into your knee, how long does it swell and hurt? Normal would be a few days and then the swelling is gone and it begins to feel better. Abnormal is that it takes weeks to reduce the swelling and feel better. If you fall into the latter category, then intervention may be needed.
Inflammtion+Healing=Bad Healing
Another issue with not being able to resolve inflammation is that it can lead to bad healing. For example, in cartilage healing, when inflammation persists beyond the first few days, that can lead to dysfunctional cartilage cells (chondrocyte hypertrophy)(4). It’s also believed that chronic low-level inflammation negatively impacts tendon healing (5).
What Can Be Done?
I’ll break this section into three categories:
- Diet and weight loss
- Anti-inflammatory supplements
- Changes to the orthobiologic injection regimen
Diet and Weight Loss
There is what’s called an “anti-inflammatory” diet. This has been shown to reduce the risk of metabolic disease related inflammatory problems like heart failure (3). More research on this diet is being created daily. The Cliff notes:
- Fruits and veggies: Go for lots of color: leafy greens like spinach and kale, broccoli, cabbage, cherries, raspberries, blackberries and many more.
- Whole grains: Oatmeal, brown rice, and other unrefined grains tend to be high in fiber.
- Beans
- Nuts
- Fish
- Herbs and spices: Turmeric, curcumin, garlic, and others.
Intermittent fasting is all the rage right now and can also help reduce whole body bad inflammation (6).
Anti-inflammatory Supplements
These are the big ones I use:
- Curcumin/Tumeric
- High quality fish oil (not the stuff you buy at Target, Walgreens, or Costco) (Also, see this article on fish oil)
- Glucosamine/Chondroitin/MSM
Changes to the Orthobiologic Injection Regimen
Finally, there are things that the physician can do to help guide the resolution of inflammation. Here are some examples:
- Injecting nanogram dose anti-inflammatories at day 3-4 if excess swelling is still present
- Upping the dose of leukocyte-poor PRP in older patients with more inflammation
- Using products like A2M in patients who have a higher risk of not being able to resolve inflammation
The upshot? How quickly you resolve inflammation after a procedure tells us quite a bit about your general health and how much systemic bad inflammation you have. If you have these kinds of issues after procedures, consider diet/weight loss, adding supplements, or discussing with your doctor how your injection regimen can be changed to maximize your outcome.
________________________________________
References:
(1) Fullerton JN, Gilroy DW. Resolution of inflammation: a new therapeutic frontier. Nat Rev Drug Discov. 2016 Aug;15(8):551-67. doi: 10.1038/nrd.2016.39. Epub 2016 Mar 29. PMID: 27020098.
(2) Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract. 2014 Aug;105(2):141-50. doi: 10.1016/j.diabres.2014.04.006. Epub 2014 Apr 13. PMID: 24798950.
(3) Kaluza J, Levitan EB, Michaëlsson K, Wolk A. Anti-inflammatory diet and risk of heart failure: two prospective cohort studies. Eur J Heart Fail. 2020 Apr;22(4):676-682. doi: 10.1002/ejhf.1746. Epub 2020 Jan 23. PMID: 31975476.
(4) Ferrao Blanco MN, Bastiaansen-Jenniskens YM, Chambers MG, Pitsillides AA, Narcisi R, van Osch GJVM. Effect of Inflammatory Signaling on Human Articular Chondrocyte Hypertrophy: Potential Involvement of Tissue Repair Macrophages. Cartilage. 2021 Jun 24:19476035211021907. doi: 10.1177/19476035211021907. Epub ahead of print. PMID: 34165367.
(5) Emanuele Chisari, Laura Rehak, Wasim S Khan, Nicola Maffulli, Tendon healing in presence of chronic low-level inflammation: a systematic review, British Medical Bulletin, Volume 132, Issue 1, December 2019, Pages 97–116, https://doi.org/10.1093/bmb/ldz035
(6) Alam, I., Gul, R., Chong, J. et al. Recurrent circadian fasting (RCF) improves blood pressure, biomarkers of cardiometabolic risk and regulates inflammation in men. J Transl Med 17, 272 (2019). https://doi.org/10.1186/s12967-019-2007-z

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.