Injecting the C1-C2 Facet Joint Under Ultrasound: A PA with a Scary Big Needle
I’ve been covering non-physician, mid-level providers performing all sorts of procedures for which, IMHO they lack adequate training. Some of these procedures are less risky than others, but this morning we’ll go over a physician’s assistant wielding a very big needle and sticking it into one of the highest-risk areas of the body. Let’s dig in.
The Upper Cervical Spine 101
There’s quite a bit going on in the high upper cervical spine. There’s the major blood supply to the back of your brain called the vertebral artery. There’s also a relatively large unprotected opening that would allow a stray needle to enter the spinal column and potentially cause a nasty high spinal cord injury.
Credit: Shutterstock
Because of these issues, even very experienced and fellowship-trained physicians with a specialty in interventional spine often decline to perform injections in this area. That’s made worse by targets like the C0-C1 facet joint being very technically demanding to access. Hence, if we take a random sampling of board-certified pain management doctors who have performed thousands of other spinal procedures, about half refuse to inject this area. Only a handful would have injected the C0-C1 or C1-C2 facet joints more than a few dozen times in their career. Even fewer do so on a regular basis (more than a few times a year). Hence, few would have developed much expertise in this area.
Mid-Levels and Spinal Injections
A mid-level is not a doctor. This designation for professionals like nurse practitioners and physician’s assistants was created to help with the workload of a supervising physician. That’s because these providers generally have half or less of the years of training of a physician specialist. However, over the past decade, mid-levels have pushed to do more and more, and while in some circumstances that can help the medical care system, in others it can create excessive patient risk that most patients wouldn’t recognize until it’s far too late.
One of those risky areas that we see more and more mid-levels injecting is the spine. On this blog, I’ve reviewed videos of mid-levels and alternative health providers performing spinal injections in ways that are frankly difficult to watch. That’s because the haphazard way in which the procedures are performed puts patients at risk of severe injury or even death. This morning we’ll dive into one of those videos sent to me by a colleague.
The Conext for this Critque
I’ve published on the safe injection of the upper cervical spine in the peer-reviewed medical literature and actively teach practicing physicians and fellows how to perform these and other procedures (1). I believe that I have injected the C0-C1 and C1-C2 joints more times (about 2,000 each) than any other living physician. Because of the nature of my medical practice and its focus on craniocervical instability, I safely inject these joints dozens of times a month or hundreds of times a year.
The Video
This video is found on the website of a prolotherapy clinic that’s run by an M.D. It’s an upper cervical injection performed by a physician’s assistant (PA). Why would an MD have a PA perform this kind of procedure? That’s a good question as there is no way I or many of my trained colleagues would allow a mid-level to inject the high upper cervical spine. What’s even more concerning here is that I know this physician has never had any training in how to safely inject this joint using any modern standard. Hence, having a PA perform a procedure that the supervising physician has no training to perform is a problem.
The name of the video is “Treating C1 Under Ultrasound”. The PA appears to be attempting to inject the C1-C2 facet joint with prolotherapy solution. I use the qualifier “attempting” here on purpose as for an expert in these injections, at no time is it clear to me that the PA documents that she has accurately injected this joint.
The Needle
The context for this upper neck injection begins with the size of the needle being used and how that’s used. A small needle in the hands of an expert where imaging is used to guide it to the right spot on the perfect trajectory becomes a valuable tool. A large needle used the wrong way can permanently damage critical structures.
The needle shown above in a video screenshot is attached to what appears to be a 20 cc syringe. Near as I can tell, it’s at least a 22-gauge 2-inch needle and may be as big as a 21 or 20 gauge 3-inch. If inserted long-axis, meaning at a shallow angle under the ultrasound probe, the risk of using a BIG needle like this could be mitigated. But inserted directly toward the upper cervical spine in a small woman, as you’ll see below (short-axis) is another story.
Short vs. Long Axis
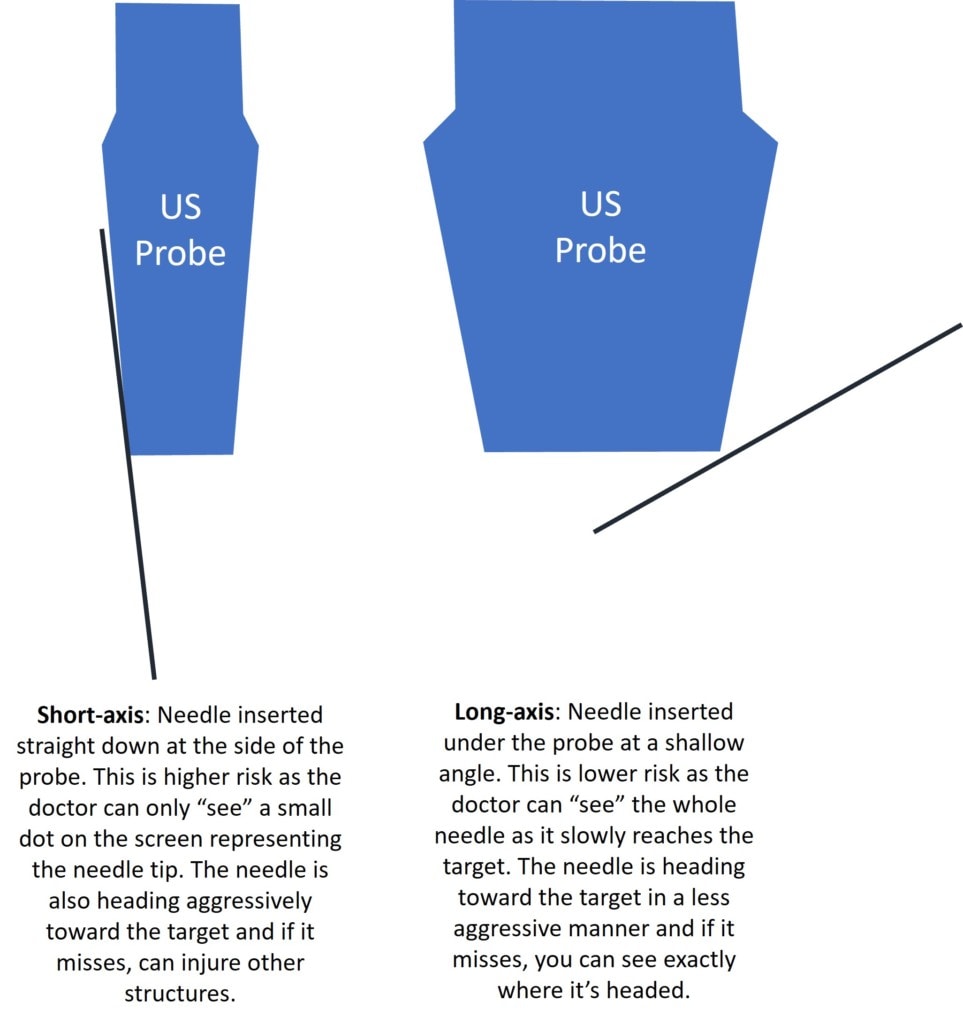
This C1-C2 procedure is being performed with ultrasound guidance. In any ultrasound-guided injection, how the needle is inserted under the probe matters. There are two main techniques: short and long axis. As shown above, if the needle is inserted short-axis as shown in this video, this is a higher risk approach, especially with a big needle in a small patient. That’s because it’s easy for non-experts to lose track of the needle tip as all the provider can see on the screen is a little dot representing the needle. In fact, at times, as shown in this video, you can’t even see that and you instead rely on “jiggling” the needle to see where it is. On long axis (not used in this upper neck injection), as shown above, you can see the needle the whole way and if you miss the target, you have better needle visualization and as such, there’s less risk of hitting something that you shouldn’t (like the vertebral artery). This is also safer in spine procedures as you’re not aiming directly at the spinal canal.
A Dangerous Rookie Mistake on Losing Track of the Needle Tip?
Remember, we’re not dealing here with a physician who went through residency using ultrasound-guided injections and then did a fellowship, but a PA (not a doctor) with a fraction of that kind of education. In addition, as shown above, the short-axis technique being used is far riskier. However, there’s another SCARY part that a non-expert would miss.
A proper short-axis injection uses the angle on the side of the probe, staying parallel with the side as shown below:
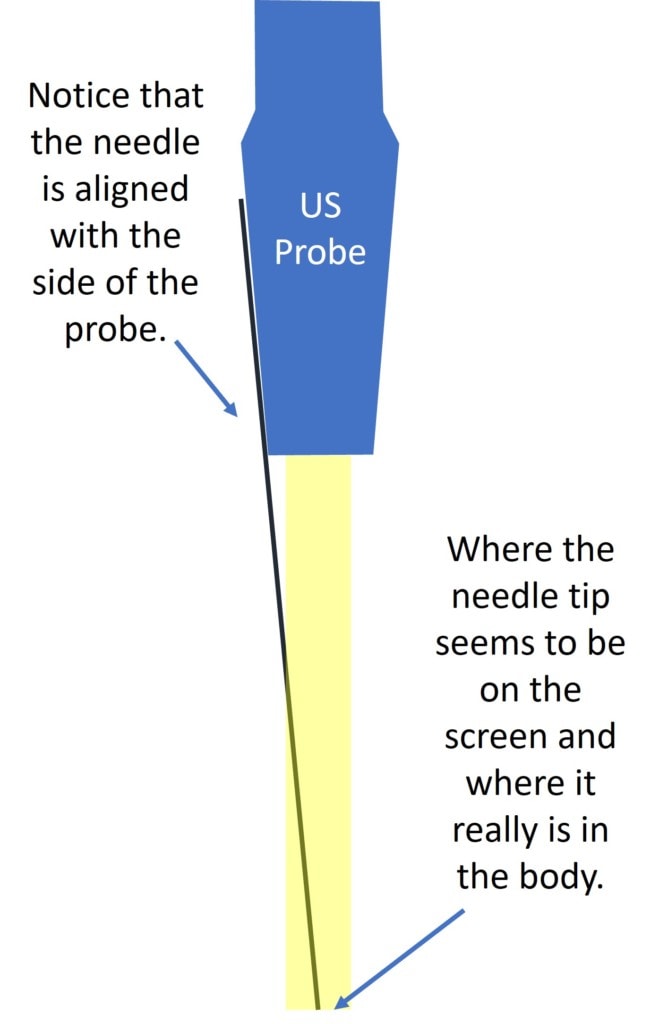
That’s because ultrasound probe manufacturers make the side of the probe so that a needle directed at that angle will end up squarely under the probe. This helps the provider visualize the needle tip at more depths as the needle is almost always in the ultrasound beam. However, after performing many thousands of these injections with a similar probe, our novice “not a physician” in my opinion has made a serious rookie mistake that I have seen countless fellows make:
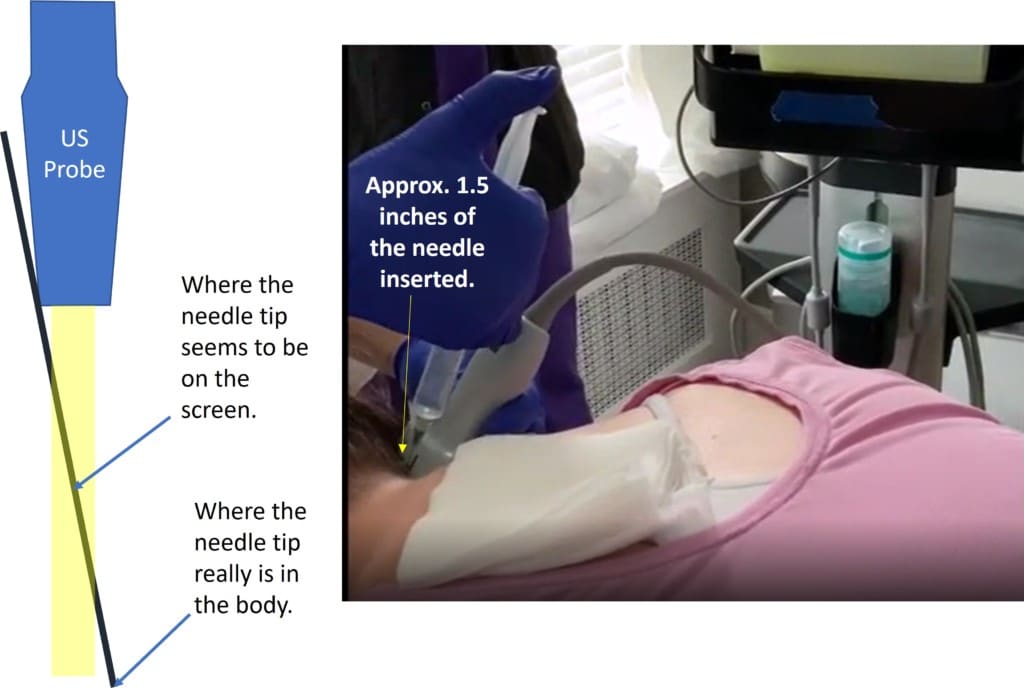
As shown above, the angle of the needle versus the angle of the probe and the depth shows an expert that what the PA thinks is the needle tip is really just an image of the proximal part of the needle. Meaning, that the “not a doctor” has likely lost track of where the needle tip is located in the body. In addition, at this steep angle toward the high upper cervical spine, it’s now a game of Russian roulette as to whether you’re injecting into the vertebral artery and about to cause a posterior circulation stroke or into the spinal cord, about to create a new quadriplegic in a sip and puff wheelchair.
A Risky Angle to Inject the C1-C2 Facet Joint
Again, to quickly review, we have a non-physician provider using a VERY BIG needle, at an aggressive angle toward the high upper cervical spine, who appears to have lost track of where that needle tip is in the body. In the next part of the video, she claims to inject the C1-C2 facet joint but based on a review of the ultrasound imaging, in my opinion, that never happens.
First, note that the injection takes place at about a 30-degree angle off of the midline. This is what the ultrasound probe would see at this angle:
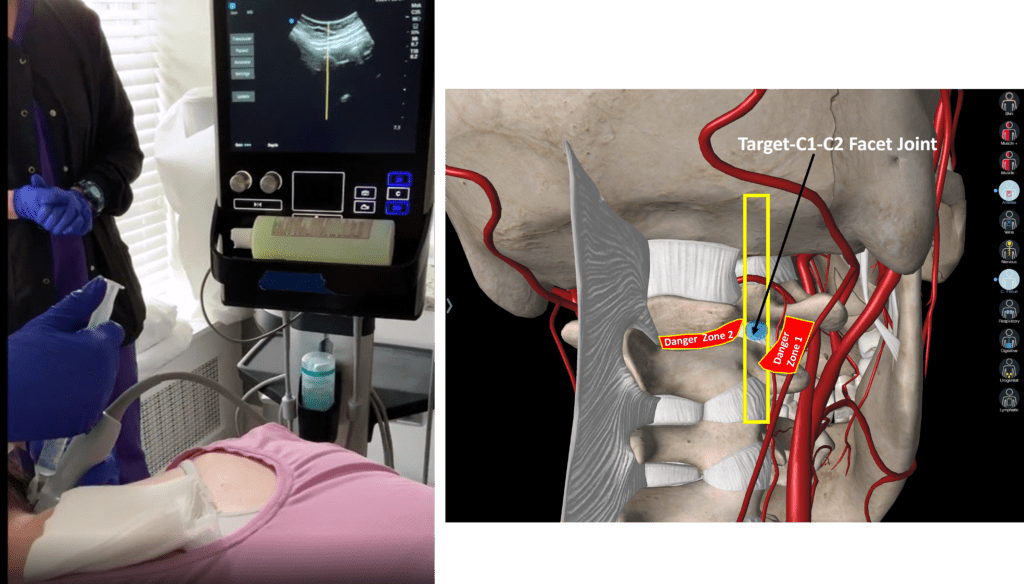
The diagram I created on the right has a yellow box, which is what the ultrasound probe is viewing versus the real anatomy. The target is marked as the C1-C2 facet joint. However, I have marked two very dangerous places where your needle could end up using this angle. One to the right of the C1-C2 joint is the vertebral artery (Danger Zone 1) where an injection of prolotherapy solution could cause a posterior circulation stroke and damage to the back of the brain. The other is just to the left of this narrow window is Danger Zone 2. If the needle strayed here, it could end up in the spinal canal and dura or spinal cord. If intradural (injected inside the covering of the spinal cord), the standard prolotherapy solution with anesthetic would cause a high spinal block, rendering the patient unable to breathe and in need of emergency resuscitation. Also, because prolotherapy solutions are hypertonic, this could also likely cause spinal cord or brain injury. Regardless of how you cut it, coming in at this angle to inject this joint is not a good idea because of these VERY NARROW margins for safety. This risk is IMHO magnified by a needle that’s too big and an approach that’s too aggressive and by the provider likely losing visualization of the needle tip.
Here’s the MUCH SAFER fluoroscopy approach:
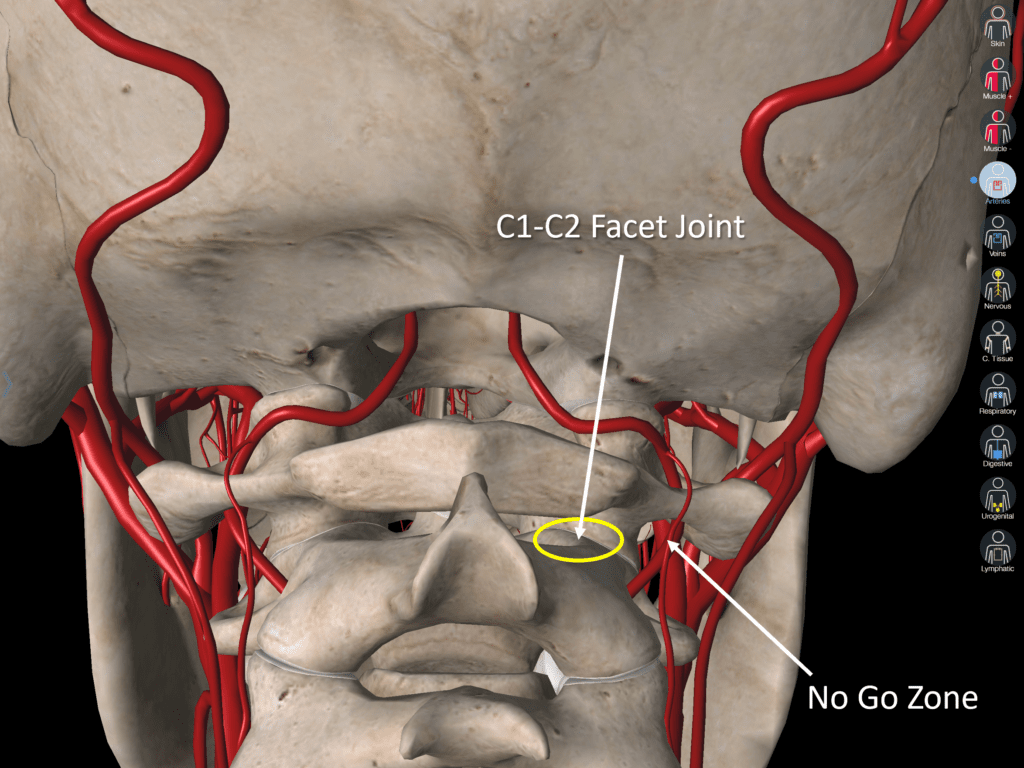
Here I’m not coming in at an angle, but straight (sagittal). By using fluoroscopy, I can see the needle at all times, not just when the ultrasound beam happens to hit it. I can also use digital subtraction angiography (DSA) to make sure I’m not inside the vertebral artery BEFORE I inject (more on that below). Also notice that there is now only one clear “No Go Zone” and a much larger space in which I can safely inject the C1-C2 joint. That spot is no longer a “Danger Zone” because I have the ability to detect that arterial injection using interventional cardiology software. The same holds true if the needle strayed too far left. Here, that’s now less likely because of my safer straight-on entry angle and again further mitigated by the fact that injecting radiographic contrast first (which is innocuous) allows me to reposition the needle out of the medial “No Go Zone” BEFORE injecting something that could injure the patient.
Was the C1-C2 Facet Actually Injected?
If a joint is injected using ultrasound, you can partially observe the fluid disappearing behind the bones and into the joint. This has a very distinctive appearance. Frankly, one of the reasons we never use ultrasound to inject spinal facet joints is that your ability, even in ideal circumstances to make sure the fluid is actually going into the joint is “OK” at best and compromised at worst. Hence, c-arm fluoroscopy is always a better option because you can make sure that the fluid will go into the joint (creating an arthrogram) and nowhere else, which is something that just can’t be done using ultrasound.
Using ultrasound, if you’re not actually injecting inside the joint, you will see the fluid back up outside the joint into the soft tissues, or the fluid is not seen flowing into the joint. For example, after reviewing the ultrasound screen as seen in the video, the first injection the provider undertakes isn’t in the joint because it backs up outside the joint. The second injection after she “walks off” superiorly from C2 doesn’t show the needle tip or the characteristic flow of fluid into a joint. Where did the prolotherapy solution go? Your guess is as good as mine.
No Defined Sterile Field
What you don’t see here is important. There are no sterile towels to mark a sterile field. The prep is a few swipes with some sort of antiseptic. Deep cervical spine injections use thorough chlorhexidine or betadine wash moving out from the center of the sterile field at least 2-3 times. They also use sterile towels to define a sterile field.
How Should This Procedure Be Performed?
Here’s a list of changes that as an expert in this procedure would need to happen to improve patient safety:
- Don’t use a PA to perform a procedure that most highly trained interventional pain management physicians won’t perform.
- Define a sterile field
- DON’T USE ULTRASOUND. This procedure in my opinion can be performed with far less risk using c-arm fluoroscopy and radiographic contrast.
- If you do use ultrasound, do not use a riskier short-axis approach, but switch to a long-axis injection.
- The injection angle should be sagittal and not at an angle to the spine, as this reduces the likelihood of ending up in the vertebral artery by widening the safe injection area and reducing the size of the danger zones. That sagittal angle also creates a backstop of the C1-C2 facet joint with a wide entry rather than the backstop for a stray needle being the spinal canal.
- To perform any high upper cervical injection, Digital Subtraction Angiography (DSA) is the standard of care. This is a software package found on c-arms that are usually used in interventional cardiology. This allows the physician subspecialist to get rid of all background clutter so that the only thing shown as highlighted during the injection is the contrast flowing. If injection into the vertebral artery is detected, the doctor can easily discern this and move the needle before a potentially noxious substance like prolotherapy solution is injected. You don’t have this level of safety control with ultrasound, so it would be very difficult to tell if you were inadvertently in this artery.
- If you can’t clearly observe the contrast being injected enter the joint with a characteristic arthrogram, then STOP your injection IMMEDIATELY! There is nothing on this ultrasound screen that shows that there there is fluid entering a joint.
Why is This Happening?
Why do we see NPs and PAs performing complex spinal procedures that most physicians won’t perform? There is little regulation and oversight in private clinics. For example, while no ambulatory surgery center or hospital would credential a PA for this injection, there are no such standards in most clinics. In addition, state legislatures have increasingly expanded the practice scope for midlevels. Finally, the coursework and hands-on experience that would allow a physician to eventually learn, after several years, to perform this procedure safely, does not exist for midlevels.
The upshot? As I just told my wife, explaining the complex so it’s simple isn’t all that simple. Despite that, I hope that I was able to show you why when I saw this video yesterday, I gasped. Also, why I would never allow one of my fellows to perform a C1-C2 injection in this manner. Nor would I ever agree to train a mid-level to perform any high upper cervical injection. As I always say, you just can’t make this stuff up!
________________________________________________________
References:
(1) Centeno C, Williams CJ, Markle J, Dodson E. A New Atlanto-Occipital (C0-C1) Joint Injection Technique. Pain Med. 2018 Jul 1;19(7):1499-1500. doi: 10.1093/pm/pnx256. PMID: 29092046.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.