Is Your Bladder Pain A Sign Of Lower Back Trouble?

Medically Reviewed By:
The connection between interstitial cystitis (IC)—also known as painful bladder syndrome (PBS) or bladder pain syndrome—and lower back pain is often overlooked. This is because treating the bladder and the lower back involves two different specialties: urology and spine care.
However, research published in the International Urogynecology Journal and Pelvic Floor Dysfunction reveals that up to 65% of individuals diagnosed with IC also experience lower back pain. Unfortunately, many patients are referred to multiple specialists, as few physicians have the comprehensive expertise to make this link.
When Is Your Bladder Pain Related To Your Low Back Nerves?
Many individuals experiencing persistent bladder pain assume it is due to a urinary tract infection or another common condition. After undergoing tests, they may receive an IC diagnosis, typically given when other identifiable causes are ruled out.
However, the situation often changes when these individuals experience lower back flare-ups, such as sciatica. Patients who receive epidural injections, sometimes with growth factors from their own blood platelets, to treat their back pain often find unexpected relief from bladder pain.
This realization highlights the connection between the bladder and the lower back. Nerve issues in the spine contribute to bladder discomfort, and recognizing this link is essential for accurate diagnosis and effective treatment.
Unfortunately, many individuals undergo extensive medical evaluations and receive treatments that fail to address the root cause of their pain, an underlying lower back issue, particularly involving nerve-related conditions.
The Connection Between Bladder Pain And The Lower Back
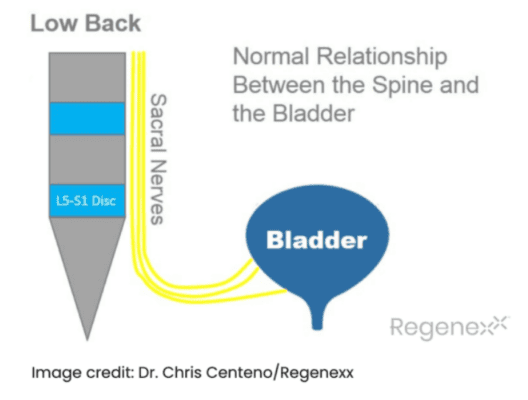
The diagram below shows the sacral nerves coursing by the L5-S1 disc in the lower back, which then travel toward the bladder and act as a conduit for bladder sensation. When functioning normally, these nerves allow sensation from the bladder to reach the brain.
The diagram below illustrates what occurs when an L5-S1 disc bulge or herniated disc places pressure on the sacral nerves. These irritated nerves can cause spasms and pain in the bladder wall.
Additionally, they may create a false sensation of bladder fullness, leading to increased urinary frequency. This occurs because the nerve signals responsible for bladder sensations are disrupted by the irritation of the sacral nerves.

Interestingly, some patients diagnosed with IC experience bladder symptoms without any noticeable back pain. However, irritated sacral nerves can still impact bladder function even without back pain.
Accompanying Symptoms To Look Out For
Bladder pain can have multiple contributing factors and is often accompanied by other symptoms, particularly in the lower back. Recognizing these signs is crucial for an accurate diagnosis and effective treatment.
Bladder pain may occur alongside:
- Lower back pain,
- Tingling, or numbness in the lower back or legs, or
- Unexplained urinary urgency or frequency.
In severe cases, symptoms such as intense back pain combined with loss of bladder or bowel control may indicate a serious condition like cauda equina syndrome, which requires immediate medical attention.
Bladder Symptoms
Bladder pain varies in intensity and may present with:
- Sharp, dull, or radiating pain in the bladder or pelvic region
- Urinary Incontinence or loss of bladder control
- Difficulty emptying the bladder
Associated Lower Back Symptoms
Bladder-related issues may also manifest as:
- Lower back pain: Pain that can range from mild to severe, often experienced as a dull ache or sharp sensation in the lower spine.
- Tingling and numbness in the lower back, legs, or feet: Nerve irritation associated with bladder issues may lead to tingling or numbness, which can extend to the legs or feet.
What Conditions Can Cause Bladder Discomfort?
Bladder pain can result from various underlying conditions, including:
- Interstitial cystitis (IC) – Chronic bladder pain linked to inflammation and nerve irritation.
- Urinary tract infections (UTIs) – Bacterial infections causing bladder inflammation and pain.
- Menstrual cramps – Pelvic discomfort that mimics bladder pain.
- Sexually transmitted infections (STIs) – Infections causing pelvic inflammation and bladder discomfort.
- Multiple sclerosis (MS) – Nerve communication disruption affecting bladder function.
- Spinal cord injury – Damage affecting bladder control and sensation.
- Spinal stenosis – Nerve compression in the lower back leading to bladder symptoms.
- Sciatica or Spinal Tumors – Conditions that may irritate sacral nerves and cause bladder discomfort.
- Muscle tension and spasms: Tight lower back muscles that impact pelvic floor function.
- Herniated Discs: A herniated disc occurs when the soft inner portion of a spinal disc pushes through its outer layer, potentially compressing nearby nerves. Depending on the affected area, this may cause pain, numbness, tingling, or weakness in the back, neck, or limbs. Read More About Herniated Discs.
- Sacroiliac Joint Dysfunction: The sacroiliac (SI) joint connects the spine to the pelvis and helps transfer weight between the upper body and legs. Dysfunction or inflammation in this joint may cause lower back pain, hip discomfort, and stiffness, often worsening with movement or prolonged sitting. Read More About Sacroiliac Joint Dysfunction.
Diagnostic Approach
A thorough evaluation is necessary to determine whether bladder pain originates from a urological condition or an underlying spine issue. Physicians typically use:
Clinical Evaluation
The clinical evaluation for bladder and lower back pain typically begins with a detailed review of the patient’s medical history, focusing on symptom onset and related health issues. A physical examination follows, including a pelvic exam for women to check for abnormalities in the bladder or reproductive organs.
A general physical assessment of the lower back also helps evaluate nerve irritation or musculoskeletal problems. The physicians will also conduct a thorough symptom assessment to identify patterns in pain, incontinence, or urinary issues, which will help guide further diagnostic tests and treatment decisions.
Differential Diagnosis
Differentiating bladder pain from other causes of lower back pain is essential for accurate diagnosis. Bladder pain can often be mistaken for gastrointestinal or gynecological issues, especially in patients with concurrent lower back pain. Misdiagnosis can result in ineffective treatments and prolonged discomfort.
Physicians must assess all potential causes, as bladder pain in individuals with lower back problems may be linked to nerve-related conditions like spinal stenosis or herniated discs. Identifying the true cause is crucial for the most appropriate and effective treatment plan.
Imaging And Laboratory Tests
Diagnostic tools are crucial for determining the cause of bladder pain and related symptoms. Common tests include:
- Ultrasound: Evaluates the bladder and pelvic organs
- CT scan: Detects spinal disc issues and nerve compression
- Urine culture: Identifies infections
- Blood tests: Detect signs of inflammation or infection
Conventional Treatment Options
Treating lower back and bladder pain often requires a multifaceted approach that addresses both the symptoms and the underlying causes.
Conservative Treatments
Conservative treatments are often the first line of defense for managing lower back and bladder pain. These approaches include:
- Physical Therapy: Targeted exercises that strengthen the muscles supporting the spine and pelvic floor, helping to relieve pain and improve bladder control.
- Lifestyle Modifications: Simple changes, such as improving posture, managing weight, and avoiding triggers like heavy lifting, can help alleviate symptoms.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or bladder-specific medications may reduce pain and inflammation, improving bladder and back function.
These treatments are non-invasive and are often effective in managing symptoms without the need for surgery or more aggressive interventions.
Bladder-Specific Treatments
Bladder-specific treatments aim to relieve bladder discomfort and improve function. These include:
- Pelvic Floor Therapy: Exercises that strengthen the pelvic muscles, aiding bladder control and reducing pain, particularly when bladder issues are related to pelvic floor dysfunction.
- Bladder Training: Techniques designed to retrain the bladder, increasing the time between urinations and reducing urgency and frequency.
- Medications For Bladder Control: Medications targeting bladder spasms, overactivity, or inflammation can help alleviate symptoms such as incontinence or frequent urination.
Accurate diagnosis is crucial, as treating bladder pain from conditions like IC without identifying an underlying spinal cause may result in ineffective treatment. Determining whether the pain originates from bladder or spine-related problems is key to successful management.
Minimally Invasive Procedures
For cases where conservative treatments aren’t sufficient, minimally invasive procedures may be the next step, especially when bladder pain is linked to nerve-related issues. Common options include:
- Injections: Steroid or platelet-rich plasma (PRP) injections near the spine can reduce inflammation and relieve bladder pain associated with nerve irritation.
- Nerve Blocks: These injections temporarily block pain signals from irritated nerves, relieving bladder and lower back pain.
These procedures are particularly useful when bladder symptoms are caused by nerve compression or spine-related issues rather than conditions like IC, which would require a different treatment approach. Accurate diagnosis is critical for selecting the appropriate intervention.
Surgical Options
In rare and severe cases, surgery may be necessary to address bladder-specific problems. Conditions such as bladder cancer or large bladder stones may require surgical removal to alleviate pain and restore normal bladder function. Procedures like tumor resection or stone removal are typically used for these conditions.
When conservative treatments fail to relieve bladder pain linked to lower back issues, surgical interventions may be considered. For example, spinal decompression surgery may be recommended to relieve pressure from a herniated disc or spinal stenosis—conditions that can mislead patients into thinking the pain originates from the bladder.
These surgeries aim to decompress nerves and alleviate both lower back and referred bladder pain, which may provide longer-term symptom relief for some individuals.
Exploring Non-Surgical Options for Bladder Pain and Sacral Nerve Irritation
For many IC patients, sacral nerve irritation is an overlooked cause of bladder pain. Physicians in the licensed Regenexx network offer interventional orthobiologic procedures as a non-surgical option designed to support nerve health and function.
Using image guidance, these procedures aim to target areas of nerve-related inflammation with Regenexx lab-processed injectates, such as platelet-rich plasma (PRP) or bone marrow concentrate (BMC). These approaches are designed to support the body’s natural repair processes.
In some cases, physicians may also recommend physical therapy to support pelvic function. This combined approach addresses underlying factors contributing to symptoms rather than solely managing discomfort. Consulting with a physician in the licensed Regenexx network can help determine whether this approach is suitable for your condition.
Accurate Diagnosis Supports Targeted Care
Bladder discomfort linked to lower back issues requires a thorough evaluation to determine the underlying cause. Whether symptoms stem from bladder-specific conditions or nerve-related spinal concerns, identifying the source is key to exploring appropriate care options.
Physicians in the licensed Regenexx network provide non-surgical approaches that may help support nerve function and mobility. Combining interventional orthobiologic procedures and conservative care, these options aim to address underlying musculoskeletal factors contributing to discomfort.
Consult with a physician in the licensed Regenexx network to explore non-surgical approaches that may help support spinal and nerve health.

Medically Reviewed By:
