Knee Injections for Arthritis-How recent Research about Hyaluronic Acid shows we have a Problem with our Research System
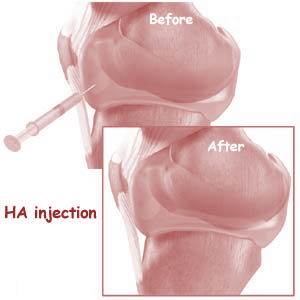
The most common knee injections for arthritis is likely cortisone-which causes severe side effects including death of a significant number of knee stem cells and cartilage cells. The second most common is SynVisc or some other form of hyaluronic acid (HA). HA is an injectable gel that replaces lost lubricating fluid in the knee. I tell my patients that it’s like WD-40. I was surprised to see a new meta-analysis this morning sent to me by one of our network docs seems to show that HA doesn’t work. Huh? For years we’ve seen this stuff work well in many of our patients. Granted it doesn’t repair damaged cartilage and it lasts for only 6-12 months and it has diminishing returns as the arthritis gets worse, but I have had hundreds of patients through the years swear by it. Yesterday we began exploring the concept that our 1960’s regulatory system can’t handle the future of medicine – HA is a great example of how and why it’s broken. So let’s take a small detour this morning before getting back to more of that book chapter on medical innovation.
This research on HA is a great example of how our regulatory and research systems are broken and often no longer serve the health of the American public. Let me explain. Our regulatory system is crazy expensive and HA is a great example that I use in the new book (in another chapter) of one of it’s problems. It’s been more than 15 years and HA has only ever been approved by FDA to treat knee arthritis, despite reams of research showing that it works well in hip arthritis as well. Why? The manufacturers simply can’t afford to start over and repeat the same research for phase 1-3 FDA clinical trials for a new indication for HA (for the hip). As a result, while an insurance company will cover the $1,200-$2,000 cost of HA for knee arthritis, they won’t cover it for hip arthritis. Does that sound nutty? It should-because it is nutty.
There’s another reason why HA isn’t covered for the hip which is aptly demonstrated by the meta-analysis this morning – generalizability. This fancy term means that research findings should “generalize” (read apply) to everyone. At at time when the rest of the world is heading in the direction of everything being customized for everyone, the regulatory and research worlds still follow a 1960’s concept that we’re all the same and hence all of our medications need to work for everyone. Our regulatory system has grown so expensive to complete, that your drug had better to apply to everyone! Forbes has the fully loaded cost of getting a new drug approved in the billions of dollars. Here, the cost would be much less-likely hundreds of millions. However, the reason this FDA approval for hip arthritis never seems to get done is that to repay investors you would need to earn many times that amount. To do this, you need to have a drug that works for almost everyone so that you can sell enough of it to cover FDA approval costs.
HA is a drug that’s likely a net positive for the joint that I and my collegues have seen work well in countless patients. So why then does this big meta-analysis seem to show that it doesn’t work? Well, first, the meta-analysis doesn’t say that – it instead says that it doesn’t work for everyone, which is true. I personally see that when I choose patients carefully who are more likely to respond to HA (they have less severe arthritis, no big swelling in the joint), about 3 in 4 patients respond well. If I were to take all patients that have a diagnosis of “arthritis” and I happened to have a practice that was 80% Medicare with many more patients with severe arthritis, only about half or less of the patients would respond. So the make-up of the patient population you test determines the results with a therapy like HA. Hence when I use it for the right patients, it works well, when some university tests it and happens to recruit the subjects with the most time to complete a study (retired and elderly patients), it doesn’t seem to work. In addition, how you inject it matters. While super-specialists like those in our practice inject it only using imaging guidance to make 100% certain the HA gets into the joint; the average family doctor or orthopedic surgeon injects blind-meaning it doesn’t get anywhere near the joint about 20% of the time.
In conclusion, what this meta-analysis demonstrates is that our regulatory system forces drug companies to make “one size fits all” solutions. Our research system then tests the drugs in “one size fits all” ways – trying to ensure they work for everyone. The media then digests that information so that it appears that a very helpful therapy for many patients doesn’t work (it just doesn’t work for everyone). Again, while the rest of the world is moving toward more customized solutions for the individual, our regulatory system forces companies to focus on a 1960’s “one size fits all” medical solution so that they can exploit big markets to pay those costs. When that solution doesn’t work for everyone, but works well in some, the therapy gets discarded because it can’t pay back the costs of regulation. In the end, the patients that could have benefited, suffer.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.