Making Sure You Get the BMC Injection You Paid For…

Last evening was my youngest son’s high school prom. As all of the parents met at somebody’s house for pictures, I spoke to a mom about a “stem cell” procedure she had done on her knee. On the one hand, she was lucky, in that she got most of what she paid for, on the other, she failed to get the highest quality treatment possible. Hence, this morning, let’s go over all of the parts of this procedure so you can get the highest possible quality procedure.
Bone Marrow Concentrate and Knee Arthritis
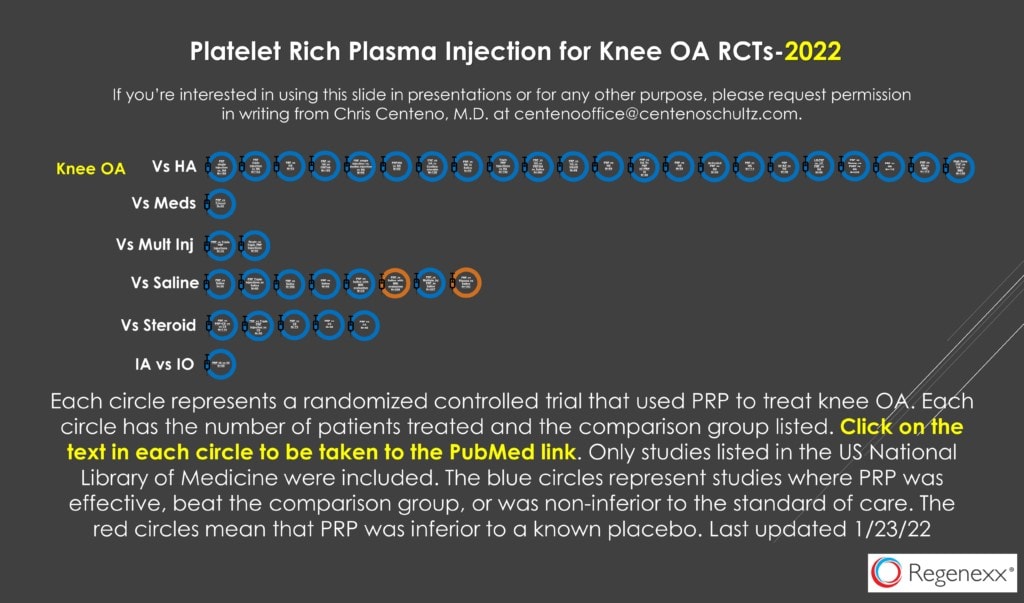
Knee arthritis is one of the better-studied problems as far as response to orthobiologic injections. Meaning we have two dozen or so randomized controlled trials (above) about the use of platelet-rich plasma and several (including our published study) on the use of bone marrow concentrate (BMC) (1-3). BMC is when the doctor takes bone marrow aspirate from the patient and pulls out the stem cell containing fractions and re-injects that material. This is what our mom at the party had done about 5 months ago.
A Talk with a Mom
The mom I spoke to was an ultra-runner, meaning she ran long distances and had patellofemoral arthritis. She had tried to get into see me, but I was too booked so she went to another local clinic with sooner availability and got a BMC knee injection. The good news is that when I went through all of the components of what she should have gotten, she could have done far worse with her choice. However, it didn’t work, so we began discussing whether she had received all of the components of the highest possible quality procedure. As I went through this quickly with her, I thought it was time for another blog, as she was bummed that in my expert opinion she received a solid, but not excellent quality procedure.
Breaking It All Down
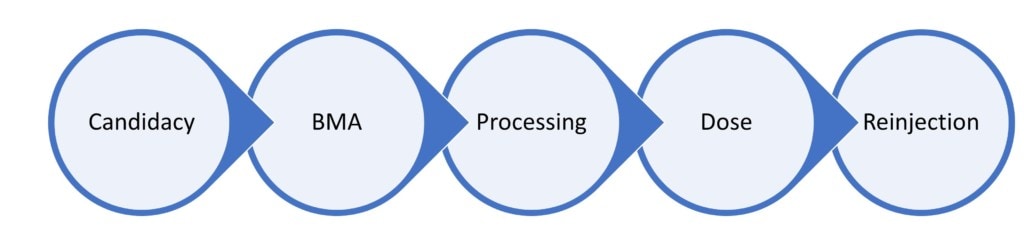
In the diagram above, I’ve broken down a knee BMC procedure into its component parts. As I go through this, I will break those parts and pieces down further. These are candidacy, BMA, processing, dose, and reinjection.
Candidacy
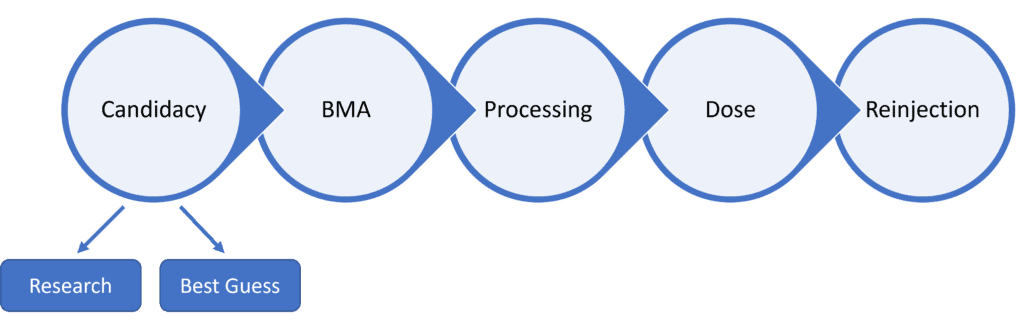
The clinic this patient went to uses a simple bedside centrifuge kit to make BMC. The problem is that NONE of the companies that sell these units has invested any money in looking at who is a good or poor candidate for their product. That’s critical because there are numerous kits on the market and we know from research that what these machines produce is very different (4). That means that in this first category, it was the doctor’s “Best Guess” as to whether her patellofemoral arthritis at her age was a good or poor candidate for the procedure she received.
To date, ONLY Regenexx has done this candidacy research. In fact, we’ve done it not once, but several times over the years. We can do this because we track every consented patient’s outcome in a sophisticated registry and are the only company in the world that has done this since 2005. In fact, for knees, we’re just completing an update of internal candidacy guidelines that relies on the complex review of more than 400 patient MRIs. Not only that, but we are just finishing a standardized synovial fluid test that uses machine learning to pick the best candidates.
CONCLUSION: Here, the patient got shortchanged. The group that she saw had no idea if she’ was a poor or a good candidate based on research they or the machine manufacturer has performed on the product that was injected.
BMA
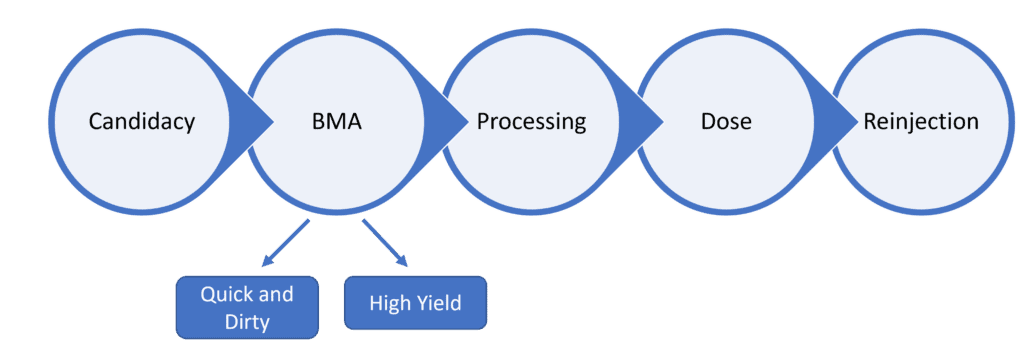
BMA stands for bone marrow aspiration. That’s when the doctor uses a specialized needle to take out what looks like thick blood from the back of the pelvis. This is a critical step because how the doctor does this can make a HUGE difference in the number of stem cells that are re-injected. It’s basically the old saying of “garbage-in/garbage-out”.
There are two main categories here: “Quick and Dirty” and “High Yield”. About 90% of the BMAs being done out there are “Quick and Dirty” and shortchange the patient of cells. That’s because they’re engineered to be fast for the doctor, which means taking a large volume of bone marrow aspirate from one or few spots. This has the effect of massively diluting the bone marrow sample with a HUGE amount of whole blood which has no stem cells. Hence, the BMA placed into the machine for concentration is stem cell poor.
“High Yield” means that the doctor took extra time to get a small volume of bone marrow from many sites. That maximizes the number of stem cells and minimizes the contamination of whole blood. Despite the research on all of this being crystal clear, most doctors still use the “Quick and Dirty” method primarily because the patient will NEVER know the difference (5-7).
How would you know which was used? This Mom didn’t know and frankly, even if she asked, she would likely never really know the difference. I would need to look at her procedure notes to be able to determine which she got.
CONCLUSION: Unknown which BMA she got, but if it turns out to be “Quick and Dirty” she was short-changed.
Processing
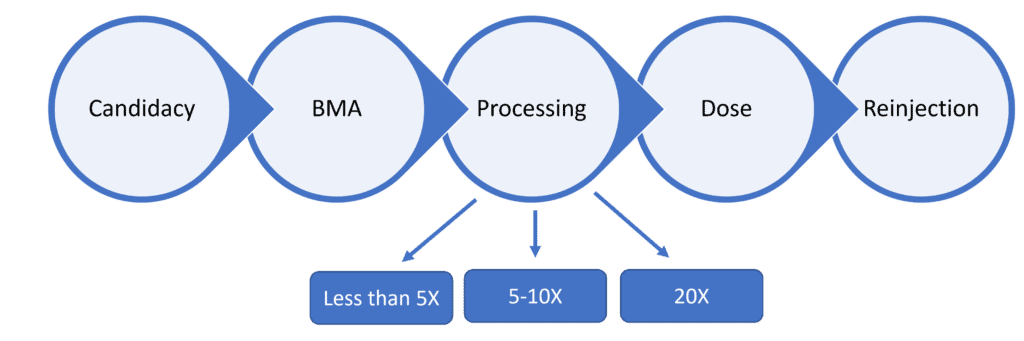
If the quality of the BMA is potentially garbage-in/garbage-out, how concentrated the doctor can get the bone marrow concentrate separates junk from the good stuff. The whole concept here is that the stem cell fractions are CONCENTRATED. Hence, how concentrated matters, especially if you’re older.
The bedside machines used by doctors who haven’t invested in their own expensive in-house lab ALL produce lower concentrations. Most produce less than 5X (5 times concentrated) BMC. One or two machines can get slightly more than that, in the low 5-10X range. If you’re 25 years old this likely won’t make much difference. However, if you’re middle-aged or older, it may make the difference between a successful and failed procedure. Why? Older stem cells tend to grow less quickly, reducing their repair abilities. The way to get over this issue is to deliver more cells per unit volume. Only a properly run on-site lab can get anywhere close to the 20X we routinely deliver every day at our Regenexx sites. When I say “properly run”, a doctor who tries to open an in-house lab usually won’t be able to accomplish these levels. They require the strict oversight we offer at Regenexx to consistently produce a super-concentrated BMC.
Our mom was treated at a place that used a simple bedside kit, so she likely got bone marrow concentrate at less than 5X. She’s 51 years old and a peri-menopausal woman, so for her, the 20X range of concentration would be critical.
CONCLUSION-The patient was likely short-changed here.
Dose
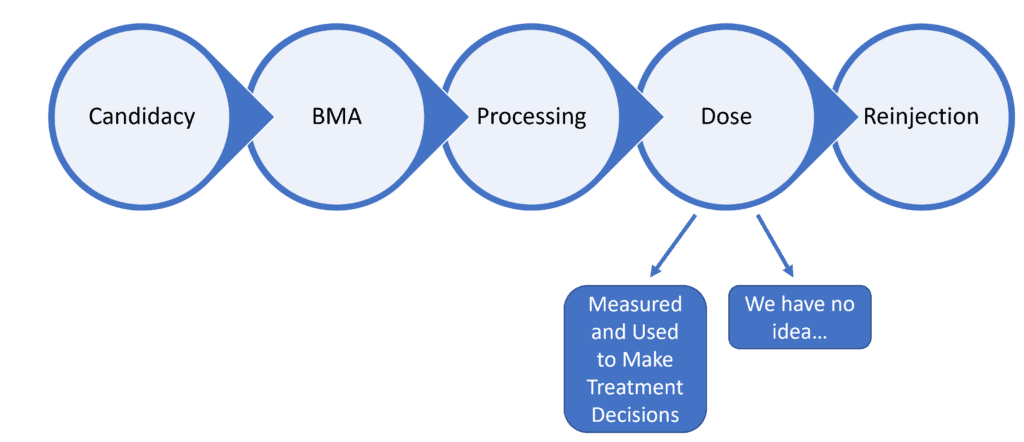
In all areas of medicine, the dose of the treatment you’re giving is CRITICAL. In fact, it’s illegal to sell prescription medications without an accurate and standardized dose. However, 95% of all of the doctors performing knee bone marrow concentrate procedures have NO IDEA of the dose they’re delivering and even if they did, they would have no idea how that impacts the treatment decisions that they should make.
Years ago we began to look at a way to measure the dose of cells and if that corresponded to the clinical outcome of a knee arthritis treatment (8). We established and since have confirmed in other studies that there was a minimum number of cells you shouldn’t go below and if you did, that patient was more likely to fail that procedure. Hence, after that published finding, we began measuring accurate cell doses in EVERY treated patient.
Despite this, if you’re using a bedside kit system, there is no way to get a dose reading. Hence, you’re flying blind. That’s what our mom had done.
How could this have made a difference? Let’s say that she had a 300 million TNCC (Total Nucleated Cell Count). That’s below our published cut-off for our specific procedure, so that would mean that we would need to VERY careful about where the cells were placed. In her case she had them injected into the bone and joint, so that means that one or the other would need to be chosen and then likely a second procedure performed (in the other area) if that first procedure failed.
Let’s say the TNCC was 1 billion. In that case, we can treat the joint, the bone, and ligaments/tendons if needed. We could even throw some of the leftover cells in another joint if required. If the procedure failed at that point, the only next step would be using culture-expanded cells like those that we can access at our licensed Grand Cayman site. Meaning, she likely didn’t fail because the dose was too low.
The upshot here is this clinic had no idea of the dose of the BMC they injected. Hence, they couldn’t act on that information. So did she fail because of a low dose of cells? Did she fail despite the right dose? Nobody knows.
CONCLUSION-Another short change of the patient.
Reinjection
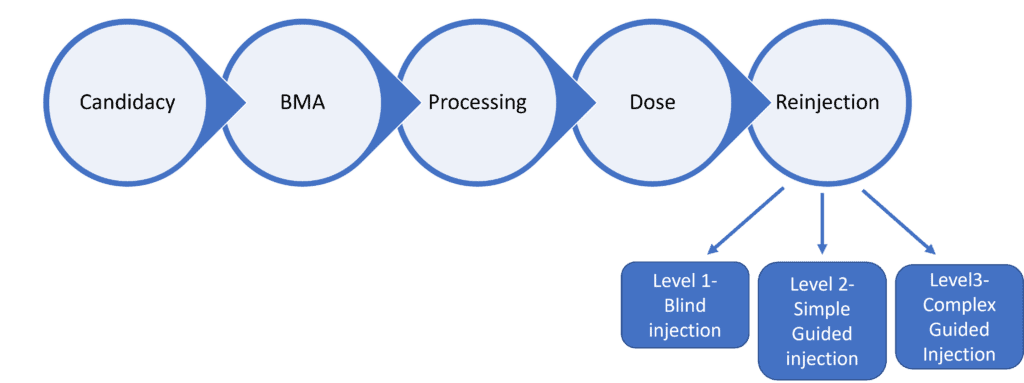
Where the cells go is also critical. This is a HUGE issue and one that patients, after they’ve been informed, generally do understand, but those who don’t do their homework often get the short end of the stick.
We can break this quality metric into 3 levels. In level 1, the doctor doesn’t use imaging guidance like ultrasound or fluoroscopy and just randomly sticks the needle somewhere in the vicinity of the inside of the joint. The doctor isn’t sure the cells got where they needed to be. In 2022, this is BELOW the standard of care. Despite that, this happens about 50% of the time.
In level 2 injections, simple guidance is used to inject the cells inside the joint. The good news is that the doctor knows that they made it there. The bad news is that there is MUCH more to understand about injecting a knee joint.
In Level 3, the doctor uses ultrasound and fluoroscopy to make sure that the cells get into specific structures like damaged bone, bad tendons, and lax ligaments. There’s a HUGE amount of difference here between clinics, with about 5% of the US clinics offering these knee arthritis procedures being firmly in the level 3 zone. However, many clinics that claim to be here aren’t. For example, they may be able to inject into the bone, but fail to use fluoroscopy which would be required for the highest quality injection. Or they may know how to inject a loose MCL ligament using ultrasound but have never learned how to use fluoroscopy to inject a damaged ACL.
The good news is that this is where our mom got better quality care. The clinic seemed to understand that for the best results in knee arthritis patients, you need to inject the damaged bone and the joint. What I don’t know is whether they had the ability to inject other critical structures. To confirm that I would need to review her procedure note and perform my own hands-on exam.
CONCLUSION-The patient likely wasn’t short-changed here. She got a re-injection toward the higher end of the quality spectrum.
PUTTING IT ALL TOGETHER
As you can see, figuring out whether you got a high, medium, or low-quality procedure to help you avoid a knee replacement requires extensive homework. Some of these things you’ll be able to figure out and some, regrettably, will still remain a mystery. That’s why I founded the Regenexx network back in 2014. The goal was to control ALL of these variables so that we could offer the best possible care. That doesn’t mean everybody gets magically better, it just means we give everyone the best shot possible. That’s why 500 US companies including many Fortune 500 players now offer Regenexx on their health plans because they know we control all of this stuff. No other group offering interventional orthobiologic procedures can make that claim.
The upshot? I hope this breakdown of my conversation with a mom at a party helps you understand that if you want to make sure you’re getting the most for your money, there’s quite a bit to know. One way to make sure that this homework has been done for you is to choose the group that’s been performing these procedures longer than anyone in the United States and has published more lab and clinical research than any other single group worldwide on bone marrow concentrate and other interventional orthobiologic procedures. Regrettably, the only group that qualifies right now is Regenexx.
______________________________________________________
References:
(1) Centeno C, Sheinkop M, Dodson E, Stemper I, Williams C, Hyzy M, Ichim T, Freeman M. A specific protocol of autologous bone marrow concentrate and platelet products versus exercise therapy for symptomatic knee osteoarthritis: a randomized controlled trial with 2 year follow-up. J Transl Med. 2018 Dec 13;16(1):355. doi: 10.1186/s12967-018-1736-8. PMID: 30545387; PMCID: PMC6293635.
(2) Hernigou P, Bouthors C, Bastard C, Flouzat Lachaniette CH, Rouard H, Dubory A. Subchondral bone or intra-articular injection of bone marrow concentrate mesenchymal stem cells in bilateral knee osteoarthritis: what better postpone knee arthroplasty at fifteen years? A randomized study. Int Orthop. 2020 Jul 2. doi: 10.1007/s00264-020-04687-7. Epub ahead of print. PMID: 32617651.
(3) Hernigou P, Delambre J, Quiennec S, Poignard A. Human bone marrow mesenchymal stem cell injection in subchondral lesions of knee osteoarthritis: a prospective randomized study versus contralateral arthroplasty at a mean fifteen year follow-up. Int Orthop. 2020 Apr 23. doi: 10.1007/s00264-020-04571-4. Epub ahead of print. PMID: 32322943.
(4) Schäfer R, DeBaun MR, Fleck E, Centeno CJ, Kraft D, Leibacher J, Bieback K, Seifried E, Dragoo JL. Quantitation of progenitor cell populations and growth factors after bone marrow aspirate concentration. J Transl Med. 2019 Apr 8;17(1):115. doi: 10.1186/s12967-019-1866-7. PMID: 30961655; PMCID: PMC6454687.
(5) Batinić D, Marusić M, Pavletić Z, Bogdanić V, Uzarević B, Nemet D, Labar B. Relationship between differing volumes of bone marrow aspirates and their cellular composition. Bone Marrow Transplant. 1990 Aug;6(2):103-7. PMID: 2207448.
(6) Muschler GF, Boehm C, Easley K. Aspiration to obtain osteoblast progenitor cells from human bone marrow: the influence of aspiration volume. J Bone Joint Surg Am. 1997 Nov;79(11):1699-709. doi: 10.2106/00004623-199711000-00012. Erratum in: J Bone Joint Surg Am 1998 Feb;80(2):302. PMID: 9384430.
(7) Fennema EM, Renard AJ, Leusink A, van Blitterswijk CA, de Boer J. The effect of bone marrow aspiration strategy on the yield and quality of human mesenchymal stem cells. Acta Orthop. 2009 Oct;80(5):618-21. doi: 10.3109/17453670903278241. PMID: 19916699; PMCID: PMC2823327.
(8) Centeno CJ, Al-Sayegh H, Bashir J, Goodyear S, Freeman MD. A dose response analysis of a specific bone marrow concentrate treatment protocol for knee osteoarthritis. BMC Musculoskelet Disord. 2015 Sep 18;16:258. doi: 10.1186/s12891-015-0714-z. PMID: 26385099; PMCID: PMC4575428.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.