Michelle’s Story: Knee Stem Cells for a Knee with Prior Surgery
One of the more common questions I get from prospective patients is whether an old surgery or “bone on bone” arthritis will eliminate their candidacy for a knee stem cell procedure. This is the story of a patient who had prior surgery and recently wrote to me about her progress with a Regenexx stem cell procedure. Let’s dig in.
Michelle’s Story
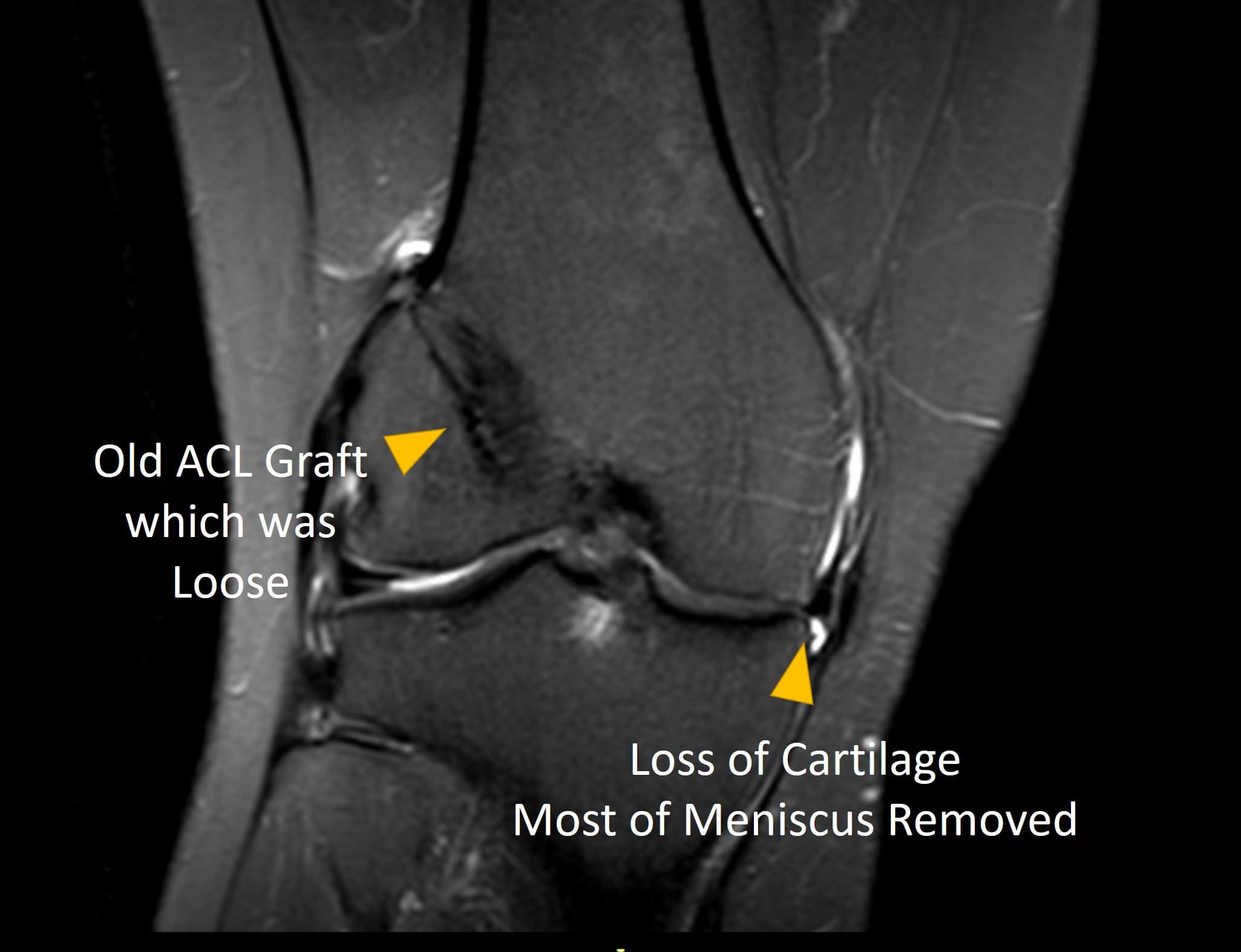
Michelle was a 55-year-old woman who had a one-year history of right knee pain after prior surgery. Her surgery was many years ago and involved a partial meniscectomy, ACL reconstruction, and MCL repair after a “terrible triad” type injury. Her MRI is above. While performing CroffFit exercises, the pain became so severe that she had to stop. When she presented to our Colorado clinic, her ACL was loose and her pain was on the inside of the knee where the meniscus had been removed. Let’s dive into what can happen to operated knees like Michelle’s.
ACL Graft Loosening
Many patients who get ACL reconstruction surgery believe that the procedure goes in and replaces the torn ACL like new. Nothing could be further from the actual truth. In fact, the ACL that’s installed isn’t a ligament, but a tendon. That tendon goes in at a different angle than the original equipment. In addition, there are no functioning position sensors in the artificial ligament, and the two ligament bundles that are normally there to control rotation are absent in most of these grafts.
Another problem with ACL grafts is that they often tear or get loose because they go in at a different angle and aren’t bonded to the bone in the same way that real ligaments are naturally bonded. For example, an ACL tendon graft is anchored to the bone at one spot, and the original equipment has thousands of tiny connections to the bone. This was the case here in that the ACL graft had become loose, causing the joint to be unstable
The Downside of Meniscectomy
In this case, the torn part of Michelle’s meniscus was surgically removed in a procedure called arthroscopic partial meniscectomy (APM). The problem? Multiple studies now show that APM is not effective across multiple clinical scenarios. In addition, removing parts of this important spacer tissue just causes more forces to build up against the bone. Hence, for Michelle, the bone had become progressively more damaged by the lack of a normal spacer.
What Procedures Did Michelle Have?
First, we used Michelle’s own bone marrow and super concentrated the stem cell fraction in that procedure, which is called Regenexx-SD. We inject that bone marrow concentrate using precise x-ray guidance into the damaged ACL graft to get it to heal and tighten. The goal there was to have the old ACL graft provide the stability it was designed to accomplish. Next, we injected that same bone marrow concentrate into the areas of the bone (intraosseous) that were struggling. Both of the above injections were performed using highly precise x-ray guidance. Finally, we injected the bone marrow into the inside of the joint where she was starting to lose cartilage.
How Did Michelle Do?
This is her recent email: “My name is Michelle [last name deleted] and you did a stem cell treatment to my right knee one year ago on August 20th. Firstly, I’m in hopes that this email finds you doing well. Secondly, I want to thank you for helping me keep the active lifestyle I so love. I am doing so much better than when we first met. I no longer have daily pain and swelling. I will say that just recently I have had some minimal pain and swelling but only once needed to ice my knee down. That being said I still believe that I am doing well. We had discussed what I could do post treatment to optimize my results and, if I remember correctly, one of the options was to have PRP injections after one year. If that is the case I would like to make an appointment to have that procedure done. Thank you for your time.”
Is Michelle’s Result Unique?
No, about 1/3 to half of all of our patients with knee arthritis who get stem cell procedures have had prior surgery. We have not detected that these prior procedures reduce their outcome.
Michelle’s ProActive Boster
What Michelle is asking for here is a ProActive booster. That means a super-concentrated platelet-rich plasma shot to boost her results at the one year mark. The goal is to stimulate the stem cells we placed in her joint. That injection will be simple with just a few days of soreness, so it likely won’t have much negative impact on her day to day activities.
The upshot? Michelle did well with our approach to her knee arthritis and got to avoid a partial knee replacement. At a year out, she could use a high-dose PRP booster, which will hopefully keep her results going for many more years to come!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.