Nerve Damage After Surgery: What Are Your Treatment Options?
In this article:
One of the biggest issues we see after surgery is scarring around the nerves (1). The most common symptoms of nerve damage after surgery are usually numbness, tingling, burning, muscle weakness or atrophy. Many times the symptoms are temporary, for example, many patients have nerve problems after surgery that only last for a few weeks to months (2,3). If they last longer than a few months, then they’re placed into the permanent nerve damage category and will likely need to be treated.
What Happens When Your Nerves Are Damaged?
Think of a nerve as a garden hose. If you constrict one area, less water comes out. This is what happens when scar tissue forms around a nerve after surgery. The scar tissue constricts the nerve which reduces the transport of critical chemicals that the nerve needs to stay healthy.
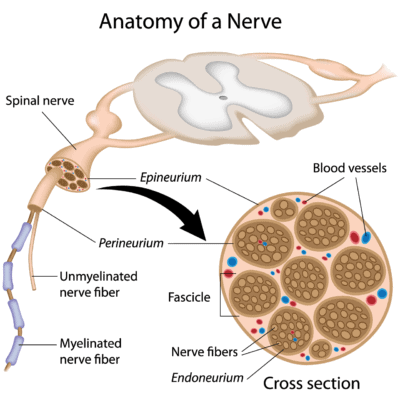
A nerve can also be damaged by killing some or all of its fibers. The image below shows that a nerve is made up of bundles of neurons (nerve cells) called fascicles. Groups of these fascicles make up the bigger nerve (4). In addition, the nerve is surrounded by a fatty sheath (myelin) that acts like an insulator covering a wire. When this sheath gets damaged there can also be a problem with nerve function.
Alila Medical Media/Shutterstock
There are three types of nerve damage:
- Neurapraxia: damage to the covering of the wire, or myelin sheath
- Axonotmesis: damage to the wire itself, or the neurons
- Neurotmesis: the nerve is torn or cut in half
How Common Is Nerve Damage After Surgery?
Somewhere between 0.5% and 2% of patients will have permanent nerve damage after surgery. Temporary nerve injury is much more common, especially in spine surgeries. See below for the nerve-related side effects of several common procedures:
- Hip replacement: 0.2% to 0.6% (5)
- Low back fusion surgery (transient nerve injury lasting less than three months): 50% to 62% (2,3)
- Shoulder replacement surgery: 21% had temporary nerve damage, 2% had permanent nerve damage (6)
What Tests Show Nerve Damage?
There are a few tests to consider if you or your doctor suspect nerve damage after surgery:
EMG/nerve conduction study
This is an electrical test of the nerve’s function. One issue is that it is highly specific but has low sensitivity. This means that it will usually only pick up nerve damage that is more severe (7).
Ultrasound imaging of the nerve
This test can determine if the nerve size shows swelling and/or constriction. It works about as well as a nerve conduction study and is less invasive (8).
MR neurography
This is a very specialized MRI scan that’s tuned to show the nerves (9).
How Long Does It Take for Nerves to Repair After Surgery?
Most episodes of nerve damage after surgery last for a few weeks to a few months. If they last longer, then the rate of nerve regrowth is about an inch a month. Therefore, if the nerve is able to regrow, a nerve injury in the back could take years to regenerate the entire nerve from your back to your foot (10). However, many times scarring in or around the nerve prevents regrowth (11).
What Helps With Nerve Pain After Surgery?
Treatment options for nerve damage and pain after surgery include:
- Orthobiologics (e.g. platelet-rich plasma — PRP)
- Physical therapy may help.
- Medications that are commonly used to treat nerve damage after surgery include:
- Neurontin (Gabapentin) (12)
- Lyrica (Pregabalin) (13)
- Elavil (Amitriptyline) (14)
- Topomax (Topiramate) (15)
- Ultram (Tramadol) (15)
Ultrasound-Guided Nerve Hydrodissection With Orthobiologics
How can you break up scar tissue around nerves? Obviously, since the scar tissue was caused by surgery, using surgery to get rid of it can be a problem. However, there’s a new way to help nerves heal and get rid of the scar tissue called ultrasound-guided nerve hydrodissection with orthobiologics. In this procedure, a nerve is visualized with ultrasound. This is used to guide a small needle to inject fluid around the nerve to break up the scar tissue.
In this procedure, which builds off our published work on treating spinal nerves with platelets, we inject the patient’s own platelet-derived growth factors that can assist nerve repair through cytokines like NGF, PDGF, and IG-1 (17,18). To see how this works on the median nerve in the carpal tunnel, see the video that follows.
Does this work? I cover two cases below.
Tanya’s Story
Tanya had a plastic surgery procedure on her gluteal area and ended up with a severe infection that caused scarring around the sciatic nerve. This basically gave her a dead leg. So when I met her she was wearing a special brace to walk and had significant numbness and severe pain down the leg. She could barely go up or down a flight of stairs. I performed the ultrasound-guided nerve hydrodissection with orthobiologics procedure a total of four times over the course of a year. I treated the entire length of the nerve, starting in the low back using fluoroscopy guidance, then turning to ultrasound-guided injections to treat the sciatic nerve down to the tibial and peroneal branches in the leg and foot. Where is she today? She no longer wears the brace, has gotten sensation back, and has limited pain. She does 30-inch box jumps in CrossFit and is planning on competing in a bodybuilding competition!
>> Find out how Tanya is doing in 2021.
Ivy’s Story
Ivy had a bad IV stick in her hand during which they injured the cutaneous branch of the ulnar nerve. Regrettably, she developed complex regional pain syndrome (CRPS) type 2 with pain so severe that she couldn’t have anyone touch the hand most days. This made it very difficult to work with kids as a nurse practitioner, as they often grabbed that hypersensitive hand.
I performed the ultrasound-guided nerve hydrodissection with orthobiologics procedure a total of four times over about a year, injecting all around the nerves in the hand, the ulnar nerve at the wrist and elbow, and the nerves in the neck. Her grip strength went from negligible to normal. Today she has very little pain most days and can see kids without a problem. This is especially remarkable because there are so few treatment options for patients once severe CRPS sets in.
The upshot? Nerve damage after surgery that doesn’t go away after a few months can be devastating. However, newer nonsurgical nerve repair techniques may be able to help.
__________________________________________________
References
(1) Tos P, Crosio A, Pugliese P, Adani R, Toia F, Artiaco S. Painful scar neuropathy: principles of diagnosis and treatment. Plast Aesthet Res. 2015;2:156-64. doi:10.4103/2347-9264.160878
(2) Liang JQ, Chen C, Zhao H. Revision Surgery after Percutaneous Endoscopic Transforaminal Discectomy Compared with Primary Open Surgery for Symptomatic Lumbar Degenerative Disease. Orthop Surg. 2019;11(4):620–627. doi:10.1111/os.12507
(3) Mueller K, McGowan J, Kane S, Voyadzis JM. Evaluation of retraction time as a predictor of postoperative motor dysfunction after minimally invasive transpsoas interbody fusion at L4-L5. J Clin Neurosci. 2019 Mar;61:124-129. doi:10.1016/j.jocn.2018.10.108
(4) King R. Microscopic anatomy: normal structure. Handb Clin Neurol. 2013;115:7-27. doi:10.1016/B978-0-444-52902-2.00002-3
(5) Fleischman AN, Rothman RH, Parvizi J. Femoral Nerve Palsy Following Total Hip Arthroplasty: Incidence and Course of Recovery. J Arthroplasty. 2018 Apr;33(4):1194-1199. doi:10.1016/j.arth.2017.10.050
(6) Lädermann A, Lübbeke A, Mélis B, Stern R, Christofilopoulos P, Bacle G, Walch G. Prevalence of neurologic lesions after total shoulder arthroplasty. J Bone Joint Surg Am. 2011 Jul 20;93(14):1288-93. doi:10.2106/JBJS.J.00369
(7) Khambati FA, Shetty VP, Ghate SD, Capadia GD. Sensitivity and specificity of nerve palpation, monofilament testing and voluntary muscle testing in detecting peripheral nerve abnormality, using nerve conduction studies as gold standard; a study in 357 patients. Lepr Rev. 2009 Mar;80(1):34-50. https://www.ncbi.nlm.nih.gov/pubmed/19472851
(8) Emril DR, Zakaria I, Amrya M. Agreement Between High-Resolution Ultrasound and Electro-Physiological Examinations for Diagnosis of Carpal Tunnel Syndrome in the Indonesian Population. Front Neurol. 2019;10:888. doi:10.3389/fneur.2019.00888
(9) Schwarz D, Kele H, Kronlage M, Godel T, Hilgenfeld T, Bendszus M, Bäumer P. Diagnostic Value of Magnetic Resonance Neurography in Cervical Radiculopathy: Plexus Patterns and Peripheral Nerve Lesions. Invest Radiol. 2018 Mar;53(3):158-166. doi:10.1097/RLI.0000000000000422
(10) Recknor JB, Mallapragada SK. Nerve Regeneration: Tissue Engineering Strategies. In Bronzino JD (ed.). The biomedical engineering handbook (third ed.). Boca Raton, Fla.: CRC Taylor & Francis.
(11) Zhang H, Uchimura K, Kadomatsu K (November 2006). Brain keratan sulfate and glial scar formation. Ann N Y Acad Sci. 1086(1):81–90. doi:10.1196/annals.1377.014
(12) Griggs RB, Bardo MT, Taylor BK. Gabapentin alleviates affective pain after traumatic nerve injury. Neuroreport. 2015;26(9):522–527. doi:10.1097/WNR.0000000000000382
(13) Khan J, Noboru N, Imamura Y, Eliav E. Effect of Pregabalin and Diclofenac on tactile allodynia, mechanical hyperalgesia and pro inflammatory cytokine levels (IL-6, IL-1β) induced by chronic constriction injury of the infraorbital nerve in rats. Cytokine. 2018 Apr;104:124-129. doi:10.1016/j.cyto.2017.10.003
(14) Matsuoka H, Suto T, Saito S, Obata H. Amitriptyline, but Not Pregabalin, Reverses the Attenuation of Noxious Stimulus-Induced Analgesia After Nerve Injury in Rats. Anesth Analg. 2016 Aug;123(2):504-10. doi:10.1213/ANE.0000000000001301
(15) Codd EE, Martinez RP, Molino L, Rogers KE, Stone DJ, Tallarida RJ. Tramadol and several anticonvulsants synergize in attenuating nerve injury-induced allodynia. Pain. 2008;134(3):254-262. doi:10.1016/j.pain.2007.04.019
(16) Centeno C, Markle J, Dodson E, et al. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017;4(1):38. doi:10.1186/s40634-017-0113-5
(17) Sowa Y, Kishida T, Tomita K, Adachi T, Numajiri T, Mazda O. Involvement of PDGF-BB and IGF-1 in activation of human Schwann cells by platelet-rich plasma. Plast Reconstr Surg. 2019 Aug 27. doi:10.1097/PRS.0000000000006266
(18) Sánchez M, Anitua E2, Delgado D, Sanchez P, Prado R, Orive G, Padilla S. Platelet-rich plasma, a source of autologous growth factors and biomimetic scaffold for peripheral nerve regeneration. Expert Opin Biol Ther. 2017 Feb;17(2):197-212. doi:10.1080/14712598.2017.1259409

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
