New Vermont Bill Would Turn PRP into a Scarlet Letter
Blog Summary:
- A Vermont bill has now incorrectly categorized PRP as “stem cell therapy”
- It seeks to have physicians who use PRP be stigmatized
- We need your help to stop this ridiculous bill
If you remember the Hawthorne novel “The Scarlet Letter” from High School English class, a young woman is made to wear a large red letter “A”. Now a new bill in Vermont wants to do the same thing for doctors who use PRP. Let’s dig in about why you should be VERY concerned about all of this and what you can do this weekend.
The Scarlet Letter
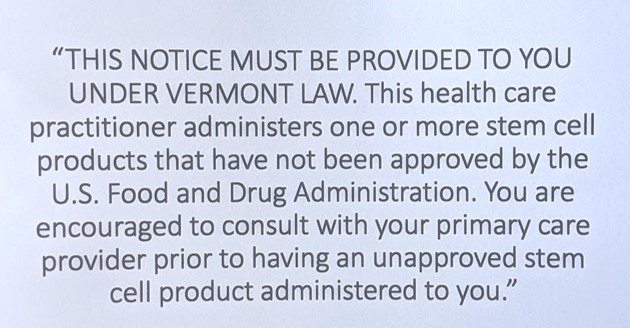
A young woman has broken the law of an early American Puritan colony, so she is forced to wear a large letter “A”. To get your “A” in high school for this class you needed to know that the story is about shaming and social stigmatizing. Now a law in Vermont wants to do the same for physicians using PRP. This bill would make them tape up a sign in 40 point font that suggests that they’re lawbreakers. This is that sign:
The Vermont Bill
How did we get here? If you remember my blog from a few months ago, a Vermont newspaper pushed out a story against stem cell clinics. That effort was being pushed by a pulmonary researcher at the University of Vermont. The story was regrettably poorly written and researched, so it lumped legit orthobiologics in with the chiro clinic crowd wanting to treat ALS with fake stem cell products.
The story seems to have produced a knee jerk reaction by Vermont legislators. The initial bill as I first reviewed it would have made any clinic offering stem cell therapy post a warning sign and use expanded informed consent. The bill botches the legal and regulatory issues around the FDA’s 1271 regulations, but it wasn’t all that different from a California law that was also a mess. What was very different from the California law is that the most recent and final version of the Vermont bill now adds in PRP and classifies it as a rogue stem cell therapy.
This is an Illegal Ad?
This is an ad that will be illegal and could cost a physician his license if this nutty Vermont bill passes:
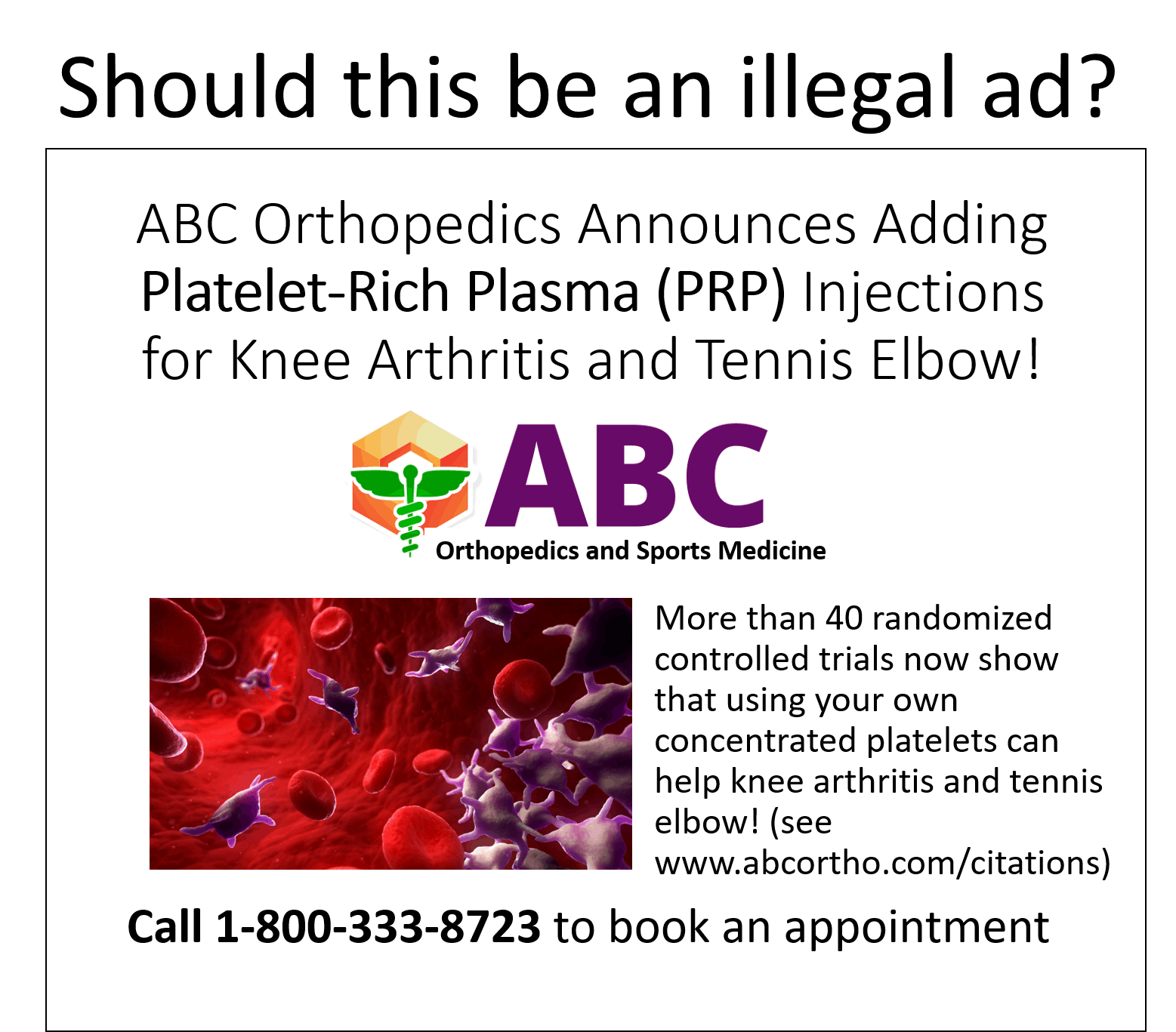
Why? The ad needs to include a disclaimer that PRP is not an FDA approved stem cell therapy! That disclaimer needs to be as big as the biggest font used.
PRP Is a Stem Cell Therapy?
The new version of the Vermont law inserted this new language, “The term also includes homologous use of minimally manipulated cell or tissue products and whole blood, blood derivatives, and blood components, as those terms are defined in 21 C.F.R. § 1271.3…” What’s being done here is to add platelet-rich plasma, a blood product, into the classification of “stem cell therapy”.
Is PRP a stem cell therapy? Nope. PRP stands for platelet-rich plasma and is made by concentrating platelets in plasma using a centrifuge. There are few if any circulating stem cells in PRP. In fact, no credible physician nor scientist working in the field of orthobiologics consider PRP a stem cell therapy.
Why Was this Added?
Behind every legislative bill is a real person or group pushing it. People have agendas. So what’s the agenda here by adding PRP? Simple, universities are in the process of lining up to license their discoveries in the stem cell space or grow cells for treatment in their labs and these FDA approved products will be expensive. Those first or second-generation cell products may not work much better than cheap PRP. However, they will cost 10-20X as much. Hence, the more than 70 randomized controlled trials showing that PRP is effective for many orthopedic problems is a net negative for this crowd. So at the last minute, the university bench scientists have inserted this language that covers PRP. This is merely one business using the legislative process to take out the competition from other businesses. This will have the effect of defrauding consumers because they will be forced to pay 10-20 more for a treatment that works no better than the one that big Pharma (and university bench scientists) want them to use.
PRP has Better Data than Any Injection or Surgical Treatment for Knee Arthritis
There are three principle traditional treatments for knee arthritis, they are corticosteroid injection, hyaluronic acid injection, or knee replacement. How does the research on those therapies stack up against PRP? Let’s dive in.
There are a pair of randomized controlled trials (RCTs) in knee arthritis patients where PRP was compared to steroid injection and was determined to be more effective (1,2). Here are fourteen RCTs where PRP was compared directly to hyaluronic acid injection. In a dozen of those research studies, PRP was found to be better than HA (3-11,13,16,17). A pair of those RCTs concluded that PRP produced similar results to hyaluronic acid injection (12, 15). As of October of last year, I had indexed 27 RCTs showing that PRP was an effective treatment for knee arthritis.
So how many RCTs do we have that show that knee replacement if effective? Just two studies. In fact, unlike many of the studies discussed above, neither of these studies was a higher quality sham control investigation. Meaning all patients knew that they had a knee replaced, which by itself would have a massive placebo effect. Meaning, big surgeries often convince patients they have improved even when the surgery didn’t really help (19).
In one of these two RCTs (18), the results of knee replacement were not very good. Meaning, you had to amputate 5-6 knee joints and replace those with a prosthesis to ensure that a single patient reported at least a lousy 15% functional improvement. Three in four of the patients who were randomized to undergo physical therapy did so well that they canceled their surgery. Hence, when compared to a knee replacement, we have significantly more high-level research demonstrating that PRP is effective.
In conclusion, the idea that Vermont wants to make doctors who treat their knee arthritis patients with PRP wear a scarlet letter is about as nutty as Ben and Jerry’s Chunky Monkey.
What You Can Do Today
If you’re a doctor or a patient who has seen the benefits of PRP, please send emails to Vermont legislators and staff right now. Send emails to:
- Sen. Virginia “Ginny” Lyons, Chair [email protected]
- Sen. Richard Westman, Vice Chair [email protected]
- Sen. Ann Cummings [email protected]
- Sen. Dick McCormack [email protected]
- Sen. Debbie Ingram [email protected]
Here are some talking points (feel free to copy, these also include a discussion of bone marrow concentrate which is also under attack):
RE: Physicians Oppose S.252
- Platelet-rich plasma (PRP) is a blood product created by FDA cleared bedside centrifuges and is used by tens of thousands of physicians nationally to help orthopedic injuries heal.
- Bone marrow aspirate concentrate (BMAC) is created by taking autologous bone marrow aspiration and centrifuging it. It has been used since the 1980s in orthopedic injuries such as fracture non-union and spine surgery.
- I oppose S.252 which would cause platelet-rich plasma, a therapy with more than 70 peer-reviewed randomized controlled trials showing safety and efficacy to be placed into the category of “stem cell therapy”. Your bill does the same with BMC.
- PRP is used widely in orthopedics and recently was awarded coverage by the military insurer TRICARE. That was based on the strength of the published data on knee arthritis and tennis elbow.
- BMC is used widely in orthopedics.
- Neither is a “stem cell therapy”, but autologous blood and bone marrow products that are used in orthopedics to enhance healing and reduce healthcare costs.
- Your bill creates a bizarre circular loop. The FDA has stated that it doesn’t regulate PRP or BMC as a drug and that these are medical procedures regulated by the states under the same surgical procedure exemption found at 21 CFR 1271.15(b). However, your bill requires that FDA approve PRP and BMC, both of which it has stated that it does not regulate.
- Hence your bill turns physicians treating orthopedic injuries with these research-based substances into “scofflaws”. They first must post a sign designed to sow mistrust. That sign doesn’t accurately describe what they do nor the regulatory status of either orthobiologic substance and it misleads patients. They also can’t get either product “FDA approved” as there is no pathway for that FDA approval. If they don’t post the sign they can lose their medical license.
- While I applaud the idea of dealing with bad actors in the “stem cell therapy” space, for these reasons, I oppose S.252 and urge you to start over on this confusing and ill-conceived legislation. This bill will ultimately harm and confuse patients.
These are “First Step” Bills
The bench scientist/ISSCR lobby that’s pushing these bills is trying to get a feel for what they can get passed. Meaning while it may or may not seem like a big deal to post this sign in your lobby, that’s just the beginning. If you look at the California bill, it didn’t include PRP. Yet PRP is a real threat to bench scientist licensed products, so it needs to be taken out eventually. Hence this Vermont bill does include PRP.
What’s next? Expect bills that roll all orthobiologics from orthopedic bone marrow to Mfat to PRP into the “bad actor” category and start to ask for state medical board sanctions for doctors using these products. It’s simply a matter of time.
What can you do long term? Get involved with your local state medical society. We’ve done that in Colorado and have had many discussions with them about the chiro bad actors and differentiating that from orthobiologics. We’ve also done the same in Florida. There was a poorly written bill that the local medical society intercepted because of an involved physician. Regrettably in Vermont, none of that happened.
The upshot? Please send emails to these Vermont legislators and staff who are railroading this bill forward. We all need to get involved if we are going to be able to get rid of the bad actors while preserving orthobiologics.
____________________________________________
References:
(1) Uslu Güvendi E, Aşkin A, Güvendi G, Koçyiğit H. Comparison of Efficiency Between Corticosteroid and Platelet Rich Plasma Injection Therapies in Patients With Knee Osteoarthritis. Arch Rheumatol. 2017;33(3):273–281. Published 2017 Nov 2. doi: 10.5606/ArchRheumatol.2018.6608
(2) Joshi Jubert N, Rodríguez L, Reverté-Vinaixa MM, Navarro A. Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial. Orthop J Sports Med. 2017;5(2):2325967116689386. Published 2017 Feb 13. doi: 10.1177/2325967116689386
(3) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(4) Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee Osteoarthritis Injection Choices: Platelet- Rich Plasma (PRP) Versus Hyaluronic Acid (A one-year randomized clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1–8. Published 2015 Jan 7. doi: 10.4137/CMAMD.S17894
(5) Görmeli G, Görmeli CA, Ataoglu B, Çolak C, Aslantürk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017 Mar;25(3):958-965. doi: 10.1007/s00167-015-3705-6.
(6) Montañez-Heredia E, Irízar S, Huertas PJ, et al. Intra-Articular Injections of Platelet-Rich Plasma versus Hyaluronic Acid in the Treatment of Osteoarthritic Knee Pain: A Randomized Clinical Trial in the Context of the Spanish National Health Care System. Int J Mol Sci. 2016;17(7):1064. Published 2016 Jul 2. doi: 10.3390/ijms17071064
(7) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(8) Lin KY, Yang CC, Hsu CJ, Yeh ML, Renn JH. Intra-articular Injection of Platelet-Rich Plasma Is Superior to Hyaluronic Acid or Saline Solution in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized, Double-Blind, Triple-Parallel, Placebo-Controlled Clinical Trial. Arthroscopy. 2019 Jan;35(1):106-117. doi: 10.1016/j.arthro.2018.06.035.
(9) Lana JF, Weglein A, Sampson SE, et al. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016;12(2):69–78. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5227106/
(10) Su K, Bai Y, Wang J, Zhang H, Liu H, Ma S. Comparison of hyaluronic acid and PRP intra-articular injection with combined intra-articular and intraosseous PRP injections to treat patients with knee osteoarthritis. Clin Rheumatol. 2018 May;37(5):1341-1350. doi: 10.1007/s10067-018-3985-6.
(11) Huang Y, Liu X, Xu X, Liu J. Intra-articular injections of platelet-rich plasma, hyaluronic acid or corticosteroids for knee osteoarthritis : A prospective randomized controlled study. Orthopade. 2019 Mar;48(3):239-247. doi: 10.1007/s00132-018-03659-5.
(12) Di Martino A, Di Matteo B, Papio T, Tentoni F, Selleri F, Cenacchi A, Kon E, Filardo G. Platelet-Rich Plasma Versus Hyaluronic Acid Injections for the Treatment of Knee Osteoarthritis: Results at 5 Years of a Double-Blind, Randomized Controlled Trial. Am J Sports Med. 2019 Feb;47(2):347-354. doi: 10.1177/0363546518814532.
(13) Yu W, Xu P, Huang G, Liu L. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med. 2018;16(3):2119–2125. doi: 10.3892/etm.2018.6412
(14) Buendía-López D, Medina-Quirós M, Fernández-Villacañas Marín MÁ. Clinical and radiographic comparison of a single LP-PRP injection, a single hyaluronic acid injection and daily NSAID administration with a 52-week follow-up: a randomized controlled trial. J Orthop Traumatol. 2018;19(1):3. Published 2018 Aug 20. doi: 10.1186/s10195-018-0501-3
(15) Louis ML, Magalon J, Jouve E, Bornet CE, Mattei JC, Chagnaud C, Rochwerger A, Veran J3, Sabatier F. Growth Factors Levels Determine Efficacy of Platelets Rich Plasma Injection in Knee Osteoarthritis: A Randomized Double Blind Noninferiority Trial Compared With Viscosupplementation. Arthroscopy. 2018 May;34(5):1530-1540.e2. doi: 10.1016/j.arthro.2017.11.035.
(16) Lisi C, Perotti C, Scudeller L, Sammarchi L, Dametti F, Musella V, Di Natali G. Treatment of knee osteoarthritis: platelet-derived growth factors vs. hyaluronic acid. A randomized controlled trial. Clin Rehabil. 2018 Mar;32(3):330-339. doi: 10.1177/0269215517724193
(17) Cole BJ, Karas V, Hussey K, Pilz K, Fortier LA. Hyaluronic Acid Versus Platelet-Rich Plasma: A Prospective, Double-Blind Randomized Controlled Trial Comparing Clinical Outcomes and Effects on Intra-articular Biology for the Treatment of Knee Osteoarthritis. Am J Sports Med. 2017 Feb;45(2):339-346. doi: 10.1177/0363546516665809.
(18) Skou S, Roos E, Laursen M, Rathleff M, Arendt-Nielsen L, Simonsen O, Rasmussen S. A Randomized, Controlled Trial of Total Knee Replacement. N Engl J Med 2015; 373:1597-1606. DOI: 10.1056/NEJMoa1505467
(19) (2) Wartolowska K, Judge A, Hopewell S, et al. Use of placebo controls in the evaluation of surgery: systematic review. BMJ. 2014;348:g3253. Published 2014 May 21. doi: 10.1136/bmj.g3253

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.