Only About Half of Hip Arthroscopy Patients Report Long-Term Satisfaction
Hip arthroscopy rates have exploded over the past decade. Despite this, we have little high-level research that this procedure is effective. Now a new study shows more disappointing outcomes. Let’s review.
Hip Arthroscopy Common for Impingement and Labral Tears
Medicalstocks/Shutterstock
The fastest growing orthopedic surgery is hip arthroscopy. The numbers of these surgeries being performed have gone through the roof. Billed as a less invasive option to hip replacement or open hip surgeries, it sounds like a good idea, but hip arthroscopy has many potential complications, and now, a new study shows many patients simply aren’t satisfied long term with the surgery.
Hip Impingement, Labral Tears, and Hip Arthroscopy Defined
The most common problems where hip arthroscopy is the preferred option are hip impingement and labral tears. Hip impingement, short for femoroacetabular impingement (FAI), most commonly occurs when the socket or ball of the hip joint develops a bone spur. Orthopedic surgeons like to go in and shave off these bone spurs, despite the fact that research shows this often isn’t a good idea as some of these typically form to protect the joint. Learn more about bone spurs by watching my short video below:
The hip labrum is a protective and stabilizing structure that forms a lip around the socket of the hip (labrum). It can tear, particularly with normal wear and tear as we age. However, a labrum tear seen on MRI doesn’t automatically mean it’s causing hip pain or that surgery is necessary to repair it; it’s often just an incidental finding.
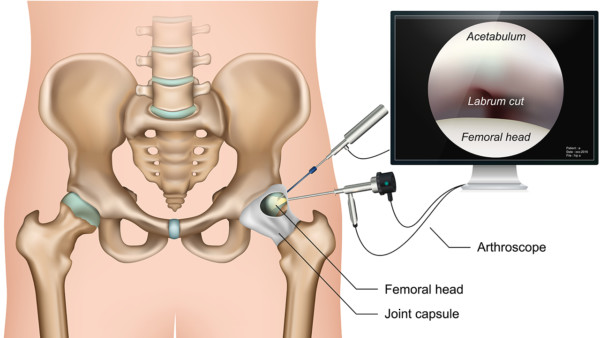
An arthroscopy, literally defined, is a visual examination (-scopy) of the joint (arthro-). This visual examination is accomplished via an instrument called a scope that is inserted through an incision in the skin, subcutaneous tissues, all the way down through the muscles to the joint. Once the scope is in place for visualization of the site, additional incisions are made to create tunnels, or portals, through which surgical tools are inserted to access the joint and perform the surgery. All other complications aside (which I cover below), just this technique alone can lead to pain after the surgery due to tissue damage that I call portal syndrome.
In addition to many studies showing hip arthroscopy for hip impingement and hip labrum tears aren’t a good idea, now it seems almost half of patients who pull the trigger on this surgery aren’t satisfied with the results long term. Let me explain.
Long-Term Patient Satisfaction and Functional Outcomes Lacking After Hip Arthroscopy
The new study consisted of patients with labral tears and hip impingement who underwent hip arthroscopy for these conditions. Long-term (5 year) functional outcomes, risk factors that could lead to hip replacement, and patient satisfaction were investigated. The results? Only 54% of patients were satisfied with their hip arthroscopy at 5 years, and only 52% showed clinically significant functional improvement (met the MCID). In addition risk factors for conversion to hip replacement included higher BMI, certain hip angles, and the greater proportions of osteoarthritis, leading researchers to recommend rigorous selection criteria for hip arthroscopy for hip impingement and labral tears.
More Problems with Hip Arthroscopy
There are many other problems with hip arthroscopy, which I’ve covered over the years. As mentioned already in regards to labrum tears, MRI is not an accurate indicator for the cause of hip pain, but this is also true for hip impingement. Patients who have no pain can have hip impingement on their MRI! So hip impingement, too, is not an automatic indicator of pain. Many more complications of hip arthroscopy for hip impingement, such as nerve damage, metal debris left behind, and worsening hip arthritis, can be found here.
If a hip arthroscopy patient also has hip arthritis with a labrum tear, common in this population, surgical outcomes are poorer. Hip arthritis was a risk factor in today’s feature study, as well, for hip replacement after hip arthroscopy.
The upshot? So we have a surgical procedure that’s invasive and works about half the time? In any other world in medicine, that would be called an ineffective therapy. In orthopedic surgery? It’s the standard of care…

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.