The Orthopedic Center of Excellence vs Changing the Surgical Paradigm
One of the hottest trends this past decade in orthopedic cost savings is the idea of an Orthopedic Center of Excellence approach. However, there are some distinct reasons why this doesn’t save employers as much money as it could. Let’s dig in through the lens of knee surgery.
The COE Concept
The idea behind an Orthopedic Center of Excellence or COE is that a patient who needs a procedure like a knee surgery will get a second opinion at a regional medical center or university. The idea is that the COE is less likely to recommend unnecessary surgery and more likely to follow strict guidelines as to who gets operated. This is a good idea that has saved countless patients from big procedures they didn’t need. However, the concept is not perfect as I’ll show below.
Knee Meniscus Surgery Outcomes
One of the most common orthopedic surgeries in America is arthroscopic partial meniscectomy (APM) for a torn knee meniscus which accounts for almost a million procedures a year and is known to be a waste of money (7). For example, we now have three large randomized controlled trials that all show that no matter the diagnosis, this surgery is ineffective (1-3). The good news is that after exploding APM rates at just under 20% a year through 2010, the number of APM surgeries has started to go down at 7% a year (4).
Because meniscectomy has clearly been shown to be ineffective in many high-level studies, we can use this as a test case to see if the COE concept works. Meaning, if a COE is to an effective cost savings tool, an academic medical center that is a clear COE site should be performing very few meniscectomy surgeries. After all, the idea behind COE is that academic medical centers will follow the research and only perform procedures we know are effective.
Meniscectomy Surgeries and Academic Centers
I don’t want to pick on any single academic orthopedic surgery department, but the Cleveland Clinic posts it’s meniscectomy numbers online and has for years, so it’s an easy one to review. First, it’s clear the Cleveland Clinic would be on anyone’s Orthopedic Center of Excellence list. This is a great orthopedic surgery department that publishes lots of research.
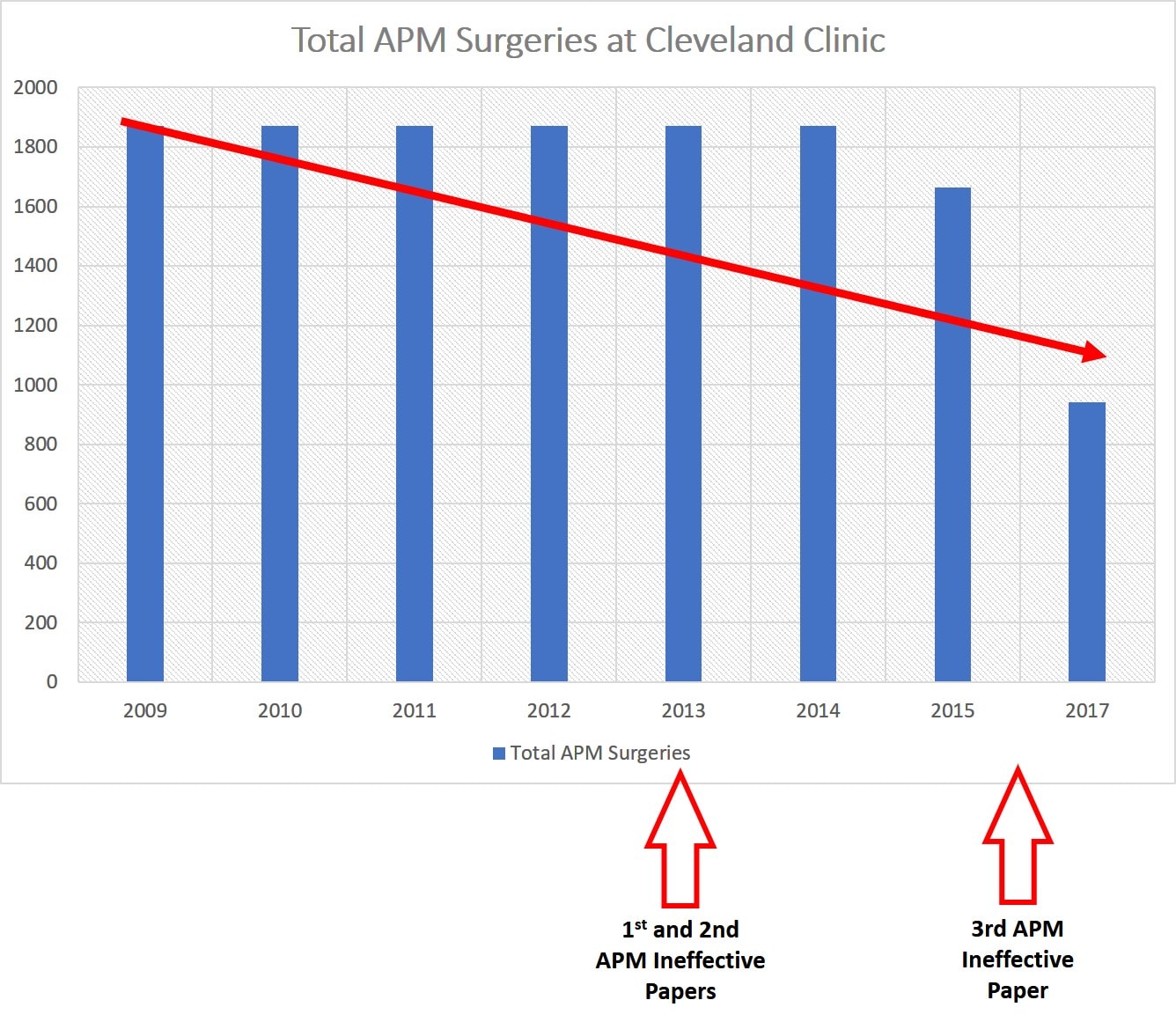
I had previously published a blog that the Cleveland Clinic orthopedic department (up through 2015) wasn’t following evidence-based guidelines when it came to APM. Meaning that based on the two 2013 studies showing that APM didn’t work, the Cleveland Clinic didn’t adjust it’s meniscectomy rates much. For example, if you look at the graph below I have the average number of meniscectomy surgeries at the Cleveland Clinic for the years 2009-2014 (the clinic just reports one number per year as an average for those years). Then I have the 2015 and 2017 totals. We should have seen a huge plunge in meniscectomy surgeries by 2015, but there was only a very small drop. We do see a bigger drop off by 2017 after the third 2016 study was published showing that APM didn’t work. However, the clinic by 2017 was still performing almost 1,000 of these clearly ineffective surgeries every year!
Let’s explore why an Orthopedic COE site would be slow to change it’s habits once we know that a procedure doesn’t work.
Surgical Conflicts of Interest
There’s an old saying that you should never put the fox in charge of the hen house. In this case, should orthopedic surgeons be in charge of determining whether orthopedic surgery is needed? Let’s explore that a bit.
Clearly, the peer-reviewed research tells us that meniscectomy rates at an academic medical center should be as close to zero as possible. My sense from looking at the Cleveland Clinic surgical rates and these studies is that less than 10% of the initial 1,800 a year who were getting APM surgeries should still be operated by 2017. That’s under 200 of these surgeries per year. However, almost 1,000 procedures were still being performed. There’s also another huge problem in this Cleveland Clinic data. The average age of patients getting APM by 2017 is still over 50 years of age. This is another clear contraindication to performing APM as we know that this surgery in this age group clearly doesn’t work (7).
So why would this be happening? Most academic medical centers incent their physicians no differently than private clinics. They are paid more if they bill more. So while you would expect an academic medical center to rapidly change their practice patterns as the data is published, there are financial reasons why it doesn’t.
Prohibition Never Works
“It is the prohibition that makes anything precious” -Mark Twain
Even if your COE sites do quickly adapt their practices to fit the published research showing that certain procedures no longer work, you have another problem as an employer, prohibition. As we all found out during the roaring twenties, prohibition doesn’t work. Whether it’s alcohol or the war on drugs, telling somebody that they can’t do something just increases the interest in that thing. The same happens with orthopedic surgery. A patient who is sent to a COE site and told they don’t need knee surgery just returns to the same family doctor who has nothing effective to offer. Hence, the patient will eventually find a way to get knee surgery as that’s what they believe will help. Is there a better way? Offer them effective non-surgical care.
Changing the Paradigm
The problem is that meniscectomy isn’t at all unique. It’s just one of many orthopedic surgeries that we know don’t work or don’t work well or where we have little evidence of efficacy that still make up a huge chunk of US healthcare spending (8). In fact, about 80% of the orthopedic surgeries you’re paying for every year fall into this category. Despite the published research, orthopedic surgeons haven’t begun to stop using many of these procedures. Even if they do, telling patients that they don’t need surgery is often ineffective and just makes them angry and resentful. So how can employers deal with all of this excessive spending?
What if we changed the construct all together? What if surgeons were no longer in charge of who gets surgery and newer non-surgical options were offered to patients? That’s what we’ve done with the Regenexx Corporate program. We’ve substituted less invasive and less expensive interventional orthobiologics procedures for more invasive and expensive orthopedic surgical procedures. In some of these plans, the surgeons are no longer in charge of who gets surgery, that decision is made by a non-surgeon. In addition, patients get an effective intervention.
A Cost Savings Study: Knee ACL Repair
For this knee surgery cost savings study we’ve used the data from our randomized controlled trial on success rates for our Perc-ACLR procedure. This procedure uses advanced x-ray guidance to inject bone marrow concentrate into a damaged ACL to promote healing:
We’ve seen great results for years and have published two papers demonstrating MRI evidence of healing of selected ACL tears without surgery (5,6). Below is an infographic with just a handful of the MRI results that we’ve published (click on the image to see a more detailed PDF).
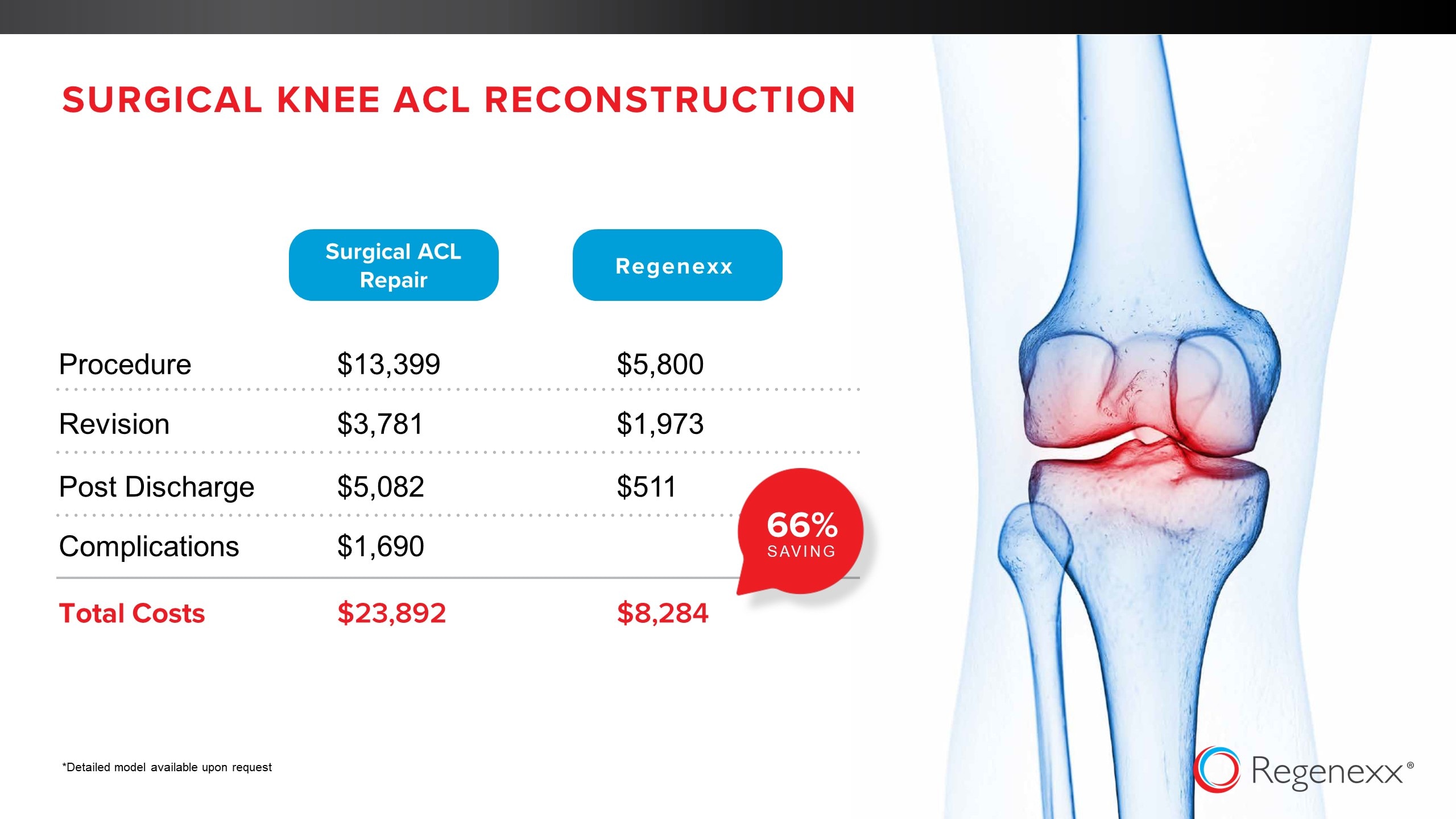
In the cost analysis above, we took the rate of failure of the Perc-ACLR procedure from our RCT data and extensive registry of cases and assumed that 100% of those cases would get ACL reconstruction. We then booked the “all in” costs for both procedures including surgical revisions and complications and rehab. In the end, the Perc-ACLR procedure was still 2/3rds cheaper than surgery. It’s important to note that these savings apply to the approximately 2/3rds of the cases that we would consider candidates for the Perc-ACL procedure.
The upshot? While the Orthopedic Center of Excellence concept can save healthcare dollars and get rid of some unnecessary surgeries, as I’ve shown it’s not perfect. It still clearly suffers from the fact that COE sites themselves, even if they’re academic centers, are still businesses and when clinics are looking at drops in revenue based on research showing that what they do is ineffective, they make those changes slowly to protect revenue. Hence, why not change the paradigm altogether? Why not take the fox out of the role of guarding the henhouse and offer your employees interventional orthobiologics?
________________________________________
References:
(1) Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis [published correction appears in N Engl J Med. 2013 Aug 15;369(7):683]. N Engl J Med. 2013;368(18):1675–1684. doi:10.1056/NEJMoa1301408
(2) Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H, Kalske J, Järvinen TL; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013 Dec 26;369(26):2515-24. doi: 10.1056/NEJMoa1305189.
(3) Sihvonen R, Englund M, Turkiewicz A, Järvinen TL; Finnish Degenerative Meniscal Lesion Study Group. Mechanical Symptoms and Arthroscopic Partial Meniscectomy in Patients With Degenerative Meniscus Tear: A Secondary Analysis of a Randomized Trial. Ann Intern Med. 2016 Apr 5;164(7):449-55. doi: 10.7326/M15-0899.
(4) Anthony Essilfie, Hyunwoo P. Kang, Erik N. Mayer, Nicholas A. Trasolini, Ram K. Alluri, Alexander E. Weber,
Are Orthopaedic Surgeons Performing Fewer Arthroscopic Partial Meniscectomies in Patients Greater Than 50 Years Old? A National Database Study, Arthroscopy: The Journal of Arthroscopic & Related Surgery, Volume 35, Issue 4, 2019, Pages 1152-1159.e1. https://doi.org/10.1016/j.arthro.2018.10.152
(5) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015;8:437–447. https://www.ncbi.nlm.nih.gov/pubmed/26261424
(6) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246. https://www.ncbi.nlm.nih.gov/pubmed/30176875
(7) Stahel PF, Wang P, Hutfless S, et al. Surgeon Practice Patterns of Arthroscopic Partial Meniscectomy for Degenerative Disease in the United States: A Measure of Low-Value Care. JAMA Surg. 2018;153(5):494–496. doi: 10.1001/jamasurg.2017.6235
(8) Lohmander L Stefan, Roos Ewa M. The evidence base for orthopaedics and sports medicine BMJ 2015; 350 :g7835 https://www.bmj.com/content/350/bmj.g7835

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.