Pain in the Back of The Heel?
As a physician who practices interventional orthopedics, I see many patients each month with pain in the back of the heel. What are the common causes of this problem? How can it be fixed? Let’s dig in.
What’s in The Back of the Heel that Could Cause Pain?
Calcaneus
The bone at the back of the heel is called the calcaneus. It supports half of your weight as your heel contacts the ground. It’s an incredibly dense bone, but it’s also possible to bruise it or fracture it if enough direct force is applied. While an x-ray would show a fracture, an MRI would be needed to detect if the bone is bruised. If the bone is bruised, usually a boot is used to protect the area for a few weeks to months (1). If that doesn’t work, other treatment options include taking medications to increase bone density (bisphosphonates), shock wave therapy, or injecting bone marrow concentrate (2) into the problem area in the bone. If all of that fails, surgery can be performed either for decompression or bone grafting.
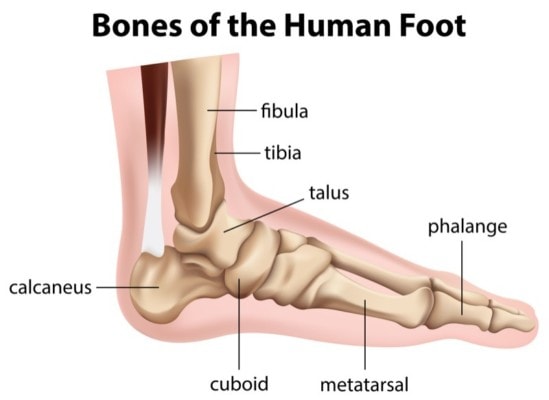
BlueRingMedia/Shutterstock
Achilles Tendon
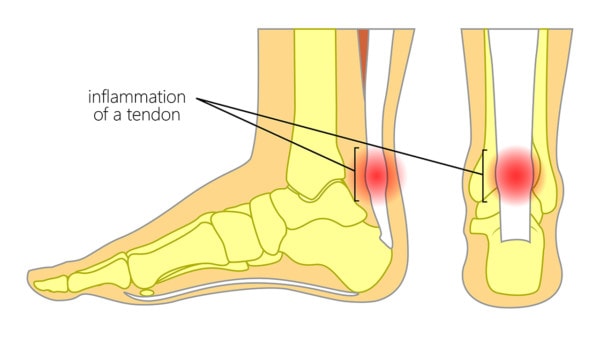
Inflammation in the Achilles tendon. Aksanaku/Shutterstock
The Achilles tendon is the heel cord that travels from your calf muscle and attaches to the calcaneus bone. It’s responsible for transmitting force as you walk and run and also helps to point your foot. The Achilles can be completely torn, but more often there are small partial tears or swelling in the tendon (also called a tendon strain). The spot where the Achilles inserts into the calcaneus can cause back of heel pain. The tendon actually goes behind the bone here (different than the image above).
If the tendon develops swelling and degeneration (known as tendonitis) or has a small tear at the back of the heel, there are a number of treatment options (3). One is simply several weeks to months of rest and placing the foot in a boot that doesn’t allow ankle movement. If the tendon has smaller partial tears or is degenerated, then shock wave therapy may be recommended (4). Another common treatment these days is ultrasound-guided platelet-rich plasma (5). Healing time after a PRP injection is usually 1-3 months and this approach has the added advantage of research that demonstrates new collagen and a stronger tendon. It’s much less common that you would need surgery, but if you do, several different approaches are used.
Heel Bursa
On either side of the Achilles tendon, at the back of the heel, there is a bursa, or lubricating sac. This allows the tendon to slide against the calcaneus and soft tissues. It can become swollen and when this happens it’s called heel bursitis, although this is less common than Achilles tendonitis. The symptoms of heel bursitis are often pain at the back of the heel, or local swelling in the area after activity. Oftentimes physicians will inject steroids into this area, but the concern is that this could cause damage to the tendon cells (16). In our experience, a better solution in an injection of PRP, which can help tendons heal rather than hurt tendon tissue. Other options include immobilizing the foot and ankle in a boot, or physical therapy.
Nerves
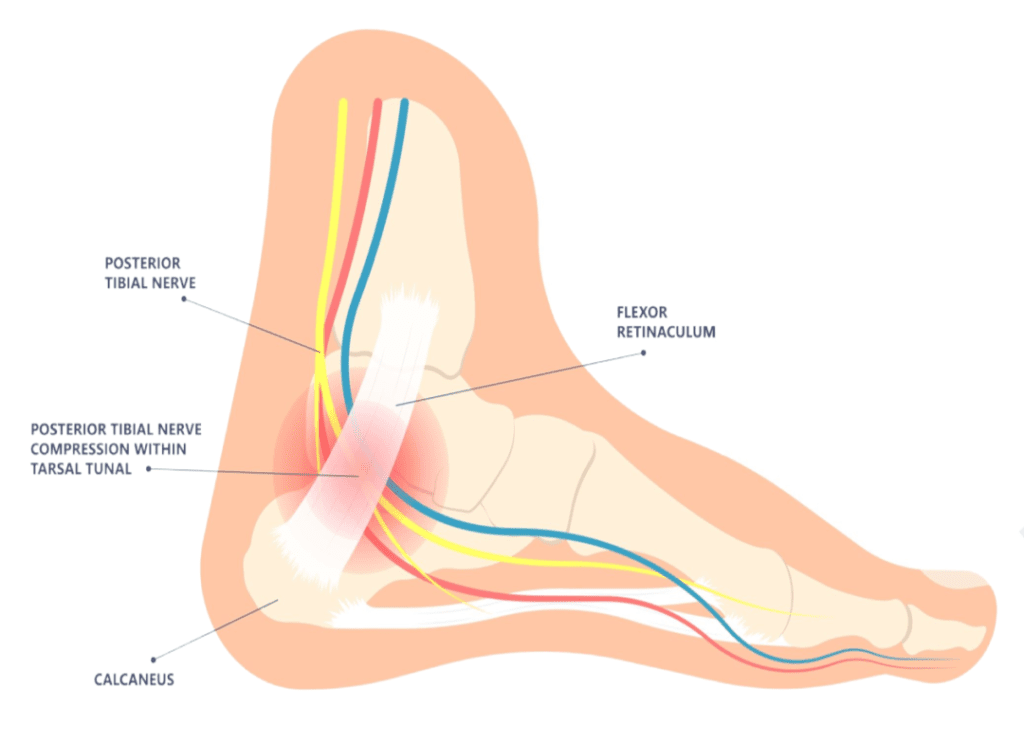
If the pain in the back of the heel is more burning or tingling, then you may have an entrapped nerve. As the diagram to the left shows, the posterior tibial nerve (in yellow bellow) runs down the inside of the ankle and sends a twig called the medial calcaneal branch to the back of the heel. The nerve passes under a tough fibrous band through an area called the tarsal tunnel. The nerve can be entrapped here and cause pain in the back of the heel or even numbness (6). This can happen because of swollen tendons that also pass through here or scar tissue that has formed from an old trauma.
Treatment for this problem is usually non-surgical. Myofascial release in physical therapy or strengthening of the muscles around the ankle may help. Other treatments which may help would include trigger point dry needling of the tibialis posterior or flexor hallucis longus muscle. We often use platelet lysate obtained from the patient’s own blood which contains growth factors that can help nerve healing (8). This is injected around the entrapped and scarred nerve using precise ultrasound guidance in a process called nerve hydrodissection. This nerve treatment technique has also been used for carpal tunnel syndrome and can improve the ability of the nerve to move freely (7). If all else fails, surgical release of the tarsal tunnel or calcaneal branch can be performed, but complication rates can be high (9).
Nerve Pain Referred from Elsewhere
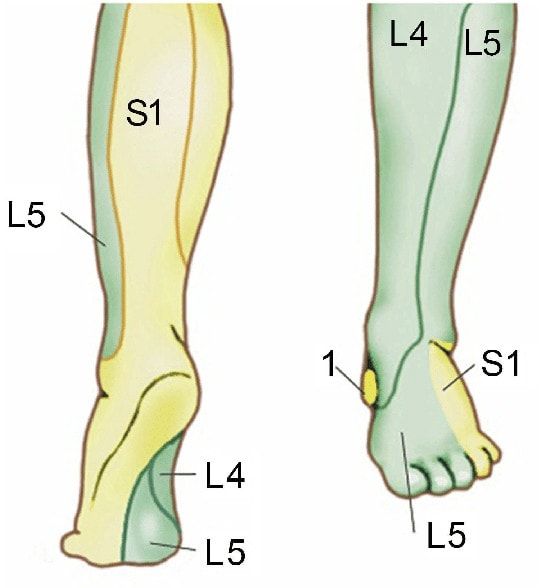
The nerves that travel into the back of the heel begin in the low back. The area on the skin that corresponds to a specific low back nerve is called a “dermatome”. A map of those for the heel is to the right. Note that the S1 nerve goes to this area, so a pinched or irritated S1 nerve in your lower back can cause pain in the back of the heel. In this case, you may or may not have much back pain, so any examination you get by a doctor for your heel should also include a look at your low back.
Treatment for this problem depends on what’s causing the nerve to get irritated but is usually non-surgical. This often starts with physical therapy (10) or chiropractic (11). If that fails, an x-ray guided epidural injection using platelet lysate may be a good bet (12). While back surgery is rare these days, that may be needed in select patients.
Other Pain Referred from Elsewhere
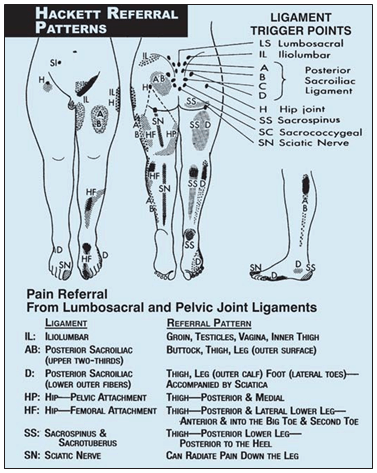
Believe it or not, there are other structures in your low back that can refer pain to the back of the heel. Note that in the image on the left, from a famous book on ligament pain referral patterns by prolotherapy pioneer George Hackett, the back of the heal is labeled “SS” (13). That means that the sacrospinous ligament in the back of the pelvis can refer pain to the back of the heel. This ligament helps to stabilize the sacroiliac joint (SI joint). Treating it is often as simple as a good manual physical therapist or chiropractor. If that fails, then prolotherapy (14) (injecting substances to cause a brief inflammatory healing process) or PRP (15) injections can help heal the damage. Surgery is only rarely needed.
Other structures that can refer pain from the low back and cause pain in the back of the heel are the supra and interspinous ligaments in the low back. These go from backbone to backbone and help keep movement in check when you bend forward. They can be injured in car crashes or other trauma. The pain patterns from those ligaments are on the right. Note that the ligament at L5 causes pain in the back of the heel. Treatment is similar to that described for the supraspinous ligament above.
The upshot? There’s lots of stuff that causes pain in the back of the heel. The big issue is getting a solid diagnosis, which often takes more than a quick 5-minute history and exam. As you can see here, the problem can be local or from your back, so make sure the doctor performs a thorough examination of both areas!
_______________________________________________
References:
(1) Eriksen EF. Treatment of bone marrow lesions (bone marrow edema). Bonekey Rep. 2015;4:755. Published 2015 Nov 25. doi:10.1038/bonekey.2015.124
(2) Harrell DB, Caradonna E, Mazzucco L, et al. Non-Hematopoietic Essential Functions of Bone Marrow Cells: A Review of Scientific and Clinical Literature and Rationale for Treating Bone Defects. Orthop Rev (Pavia). 2015;7(4):5691. Published 2015 Dec 28. doi:10.4081/or.2015.5691
(3) Yang X, Meng H, Quan Q, Peng J, Lu S, Wang A. Management of acute Achilles tendon ruptures: A review. Bone Joint Res. 2018;7(10):561–569. Published 2018 Nov 3. doi:10.1302/2046-3758.710.BJR-2018-0004.R2
(4) Lee JY, Yoon K, Yi Y, et al. Long-Term Outcome and Factors Affecting Prognosis of Extracorporeal Shockwave Therapy for Chronic Refractory Achilles Tendinopathy. Ann Rehabil Med. 2017;41(1):42–50. doi:10.5535/arm.2017.41.1.42
(5) Liu CJ, Yu KL, Bai JB, Tian DH, Liu GL. Platelet-rich plasma injection for the treatment of chronic Achilles tendinopathy: A meta-analysis. Medicine (Baltimore). 2019;98(16):e15278. doi:10.1097/MD.0000000000015278
(6) McSweeney SC, Cichero M. Tarsal Tunnel Syndrome – a narrative review of the literature. J Foot Ankle Res. 2015;8(Suppl 2):P9. Published 2015 Sep 22. doi:10.1186/1757-1146-8-S2-P9
(7) Evers S, Thoreson AR, Smith J, Zhao C, Geske JR, Amadio PC. Ultrasound-guided hydrodissection decreases gliding resistance of the median nerve within the carpal tunnel. Muscle Nerve. 2018;57(1):25–32. doi:10.1002/mus.25723
(8) Sánchez M, Garate A, Delgado D, Padilla S. Platelet-rich plasma, an adjuvant biological therapy to assist peripheral nerve repair [published correction appears in Neural Regen Res. 2017 Mar;12 (3):338]. Neural Regen Res. 2017;12(1):47–52. doi:10.4103/1673-5374.198973
(9) Perera N, Liolitsa D, Scott Hill C, et al. Surgical interventions for entrapment and compression of the tibial and deep peroneal nerves including tarsal tunnel syndrome. Cochrane Database Syst Rev. 2017;2017(6):CD010630. Published 2017 Jun 12. doi:10.1002/14651858.CD010630.pub2
(10) Childs JD, Fritz JM, Wu SS, et al. Implications of early and guideline adherent physical therapy for low back pain on utilization and costs [published correction appears in BMC Health Serv Res. 2016 Aug 26;16(1):444]. BMC Health Serv Res. 2015;15:150. Published 2015 Apr 9. doi:10.1186/s12913-015-0830-3
(11) Goertz CM, Long CR, Vining RD, Pohlman KA, Walter J, Coulter I. Effect of Usual Medical Care Plus Chiropractic Care vs Usual Medical Care Alone on Pain and Disability Among US Service Members With Low Back Pain: A Comparative Effectiveness Clinical Trial. JAMA Netw Open. 2018;1(1):e180105. Published 2018 May 18. doi:10.1001/jamanetworkopen.2018.0105
(12) Centeno C, Markle J, Dodson E, et al. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017;4(1):38. Published 2017 Nov 25. doi:10.1186/s40634-017-0113-5
(13) Hackett, GS. Ligament and tendon relaxation (skeletal disability) treated by prolotherapy (fibro-osseous proliferation): With special reference to occipito-cervical and low back disability, trigger point pain, referred pain, headache and sciatica. Thomas, 1958.
(14) Hauser RA, Lackner JB, Steilen-Matias D, Harris DK. A Systematic Review of Dextrose Prolotherapy for Chronic Musculoskeletal Pain. Clin Med Insights Arthritis Musculoskelet Disord. 2016;9:139–159. Published 2016 Jul 7. doi:10.4137/CMAMD.S39160
(15) Mohi Eldin M, Sorour OO, Hassan ASA, et al. Percutaneous injection of autologous platelet-rich fibrin versus platelet-rich plasma in sacroiliac joint dysfunction: An applied comparative study. Back Musculoskelet Rehabil. 2019;32(3):511-518. doi: 10.3233/BMR-181366.
(16) Nuelle CW, Cook CR, Stoker AM, Cook JL, Sherman SL. In Vivo Toxicity of Local Anesthetics and Corticosteroids on Supraspinatus Tenocyte Cell Viability and Metabolism. Iowa Orthop J. 2018;38:107–112. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6047373/

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.