PRP Injection Didn’t Help? Is All PRP Created Equal?
The use of platelet-rich plasma, or PRP, is becoming increasingly common in more medical practices. So much so that we’re beginning to see treatment failures where a PRP injection didn’t help. Why? One reason is that all PRP isn’t created equal. In fact, there are really big disparities, yet most patients don’t understand these stark differences. So let’s take a deep dive into this topic this morning.
Why Write This Blog?
I get pinged all the time by patients who state that they tried “PRP,” but a PRP injection didn’t help, so what’s next? The first question is whether they got a high-quality or a low-quality PRP treatment. To understand the difference, you first need to realize that PRP isn’t just one thing. So let’s first delve into what PRP is and the different types.
What Is PRP?
PRP stands for platelet-rich plasma, which is when platelets are concentrated from whole blood. Your blood contains platelets, which have healing growth factors inside them, and these are what not only help clot a wound but also heal that damage. By increasing the number of these healing platelets through a centrifugation protocol, doctors hope to be able to enhance healing.
The Two Main Types of PRP
There are two main types of PRP—red and amber. You can notice these color differences pretty easily when the doctor has the PRP in the syringe. Here are the major differences:
Red—leukocyte rich (LR)—has many red and white blood cells.
Amber—leukocyte poor (LP)—has few red and white blood cells.
What’s the main difference? While this is a hotly debated topic in medical circles, based on a number of studies, the red PRP seems to be less effective in treating tendons and joint arthritis. The amber type seems to be more effective. In addition, in our experience, amber PRP causes fewer flare-ups in patients. Why? When the body sees a bunch of red blood and white blood cells, it believes a major injury has occurred and sends the area tons of inflammatory cells, which shows up as swelling. In some patients, this may not be a bad thing, but in other patients, the inflammation can spin out of control.
Differences in Concentration
One of the interesting debates in the world of PRP is, how many platelets do you need? Is more concentrated PRP better? Or is less concentrated fine?
We at Regenexx have a unique perspective here. We began using platelets to grow stem cells in the lab very early on, back in 2005. We noticed pretty quickly that the higher the concentration of platelets in the culture, the better the stem cells grew. This was especially true with the cells of older patients. Hence, we went with higher platelet concentrations and saw great results.
How high of a concentration do we use? Most bedside machines can only concentrate cells to 3–7 times over their baseline concentration in blood (3–7X). Our flexible lab platform can concentrate up to 20X. In fact, in older patients, we routinely use concentrations of up to 10–14X. This has enabled us to successfully treat patients with our PRP who have failed other less-concentrated or red PRP therapies.
To give you an idea of how hot a debate this is right now, a few years ago, a researcher published a paper that seemed to show that higher concentrations of stem cells were bad for healing tendons. However, our research team immediately noticed that the experimental design of this study was poor. Hence, we re-created the study and fixed the bad research methods and continued to find that higher concentrations of cells produced better results in experimental models of tendon healing, especially in older patients. For more info, see my video below:
[VIDEO=267]
This research performed by our lab team has now been accepted for publication, so, hopefully, we’ll have that for you soon.
Putting It All Together
So you want to be injected with amber PRP to treat the most common orthopedic problems. In addition, you want a high concentration of platelets. This is our concentration guideline based on age: 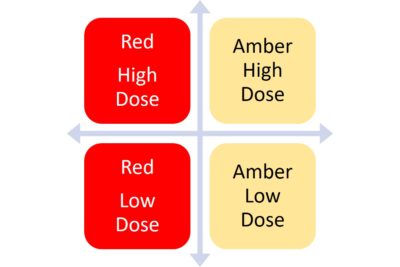
Under 35: 5X
35–45: 7–10X
45–65: 10–14X
65+: 14–20X
The chart to the left will help you visualize all of this. So you want “Amber High Dose,” but high dose depends on your age. So the usual amber PRP from a bedside machine might be fine if you were 25, but not if you’re 55.
What + How + Where
So we’ve focused on what’s injected, but also recognize that how and exactly where it’s injected also makes a tremendous difference. So let’s focus on “How” first and then “Where” second. Let’s begin drilling down.
What do I mean by “How”? This means all the stuff you need to know to avoid hurting tissue while you’re injecting something to help tissue. For example, many doctors use the local anesthetic known as Marcaine (bupivacaine). This stuff kills many local cells dead, so injecting it with PRP is just plain dumb. Despite this, many doctors perform a PRP injection this way. Another example is injecting a high-dose steroid. This also kills cells dead, but many doctors inject this before they use PRP or inject it with PRP.
How about “Where”? By this, I mean the exact placement of the PRP into the damaged tissues. Most doctors inject PRP blind (meaning without guidance). This makes little sense as if the platelets aren’t placed into the damaged tissue, how is that supposed to work? You might think all of this is easy, but it’s not. Meaning, only about 1% or less of orthopedic surgeons would know how to use ultrasound imaging or fluoroscopy to place the PRP in the right spot. Even interventional spine doctors will often struggle to place it in the right spot in the peripheral joints, like the knee or shoulder. Even in the spine, most of these doctors also aren’t knowledgeable about how to deploy the PRP to get the maximum benefit. To see what I mean, watch my video below:
[VIDEO=214]
The upshot? Not all PRP is created equal, which is one reason it can fail. So when your doctor says that he or she can inject you with PRP, there’s a lot to know as a patient to see if this plan is maximizing or minimizing your likelihood of success.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.