The Artificial Disc Replacement Hustle
Medicine is often more about marketing than reality. One area where masterful marketing has overtaken reality is the promise of an artificial disc. Let’s explore the hype and the reality today.
The Promise of the ADR
Both fusion and disc replacement surgery are performed in patients with DDD (Degenerative Disc Disease). DDD is when the disc loses height, bone spurs develop, degenerative instability takes hold, and often nerves get banged into causing pain. This happens in both the neck and the low back.
ADR stands for Artificial Disc Replacement. The idea is that spinal fusion is a dumb idea because it stops all motion and transfers those forces to the spinal segments above and below leading to ASD (Adjacent Segment Disease). However, if the surgeon can install something that moves, that problem will be solved. Sounds good, right? Hence the industry that brought you a $3 screw made in China, Vietnam, or India that sells for $1,000 to a US insurance company has created ADR devices.
The problem with ASD is that it usually means more surgeries down the road. So basically we’re fixing one problem and causing another. Given that in my patients, the whole reason for choosing disc replacement over fusion is to avoid more surgeries, if these ADR devices don’t change that rate, then they might as well get a fusion.

Credit: Shutterstock
To learn more about ASD, see my video below:
Reality
This quick literature review is from this past blog on ADR side effects. The first study that hit me on a search of the US National Library of Medicine search was a 5-year randomized controlled trial of disc replacement versus fusion in the neck. It concluded that there is no difference in the rate of ASD between the procedures (1).
Then I found these studies:
- This study demonstrated that the way the spine bones moved is changed by ADR (2). Meaning they don’t move in the way they were designed.
- This high-level meta-analysis concluded that a reduction in ASD can’t yet be proven when ADR is compared to fusion (3).
- This Swedish registry study also concluded no difference in ASD rates between ADR and fusion at 5 years (4).
Now compare those studies showing that ADRs don’t prevent ASD to this 2018 recent review of the literature that seemed to be a glowing review of the technology (5). However, the supervising author on this one is a US neurosurgeon, so I looked up his page on the ProPublica website to see if he had received money from device manufacturers. Sure enough, he’s listed as receiving more than a million dollars in device-company payments.
There are other studies comparing specific ADR devices to fusion, which all seem to show better results. However, most of these seem supported by a specific manufacturer of a specific device. I wanted to look up more physicians involved in these studies, but it seems like most of the device-company-sponsored studies are performed in China, making those physicians and their payments outside of the reach of US Internet searches.
Even those studies aren’t all glowing. Take, for example, this 5-year study performed on the Prestige-LP device (6). This seemed to show that the Prestige artificial disc was better than a fusion spacer in terms of a reduction in ASD (8.3% vs. 22%). However, exactly one-third of patients who got the Prestige device had heterotopic ossification as a side effect of the device. What’s that? Very concerning abnormal bone growth.
New Research
It’s been a while since I looked into this area, so let’s highlight the results of a recently published study. This is a continuation of a follow-up from a randomized controlled trial of the ProDisc-C ADR device (7). The lead author of this paper received $410,509.61 in payments from drug and device companies in 2021 alone compared to the average physician getting paid $3,829 by these companies. 2020 was a bad year in that he only received $117K versus $3,306 for all doctors. Finally, 2019 was a banner year in which he received $540,958 compared to the average US physician receiving $3,816. I think you get the idea, this spine surgeon is not a stranger to the device industry.
Forgetting about total payments from the companies that make drugs and devices to surgeons who author these papers, let’s dive into the substance of the research. The paper claims that the ADR device performs much better than fusion in terms of ASD:
The translation? ADR devices are kicking butt and living up to the promise of much less ASD! However, just like many stories told with data, it takes looking under the hood to tell the difference between reality and spin. This is a graph I made with the data from this study:
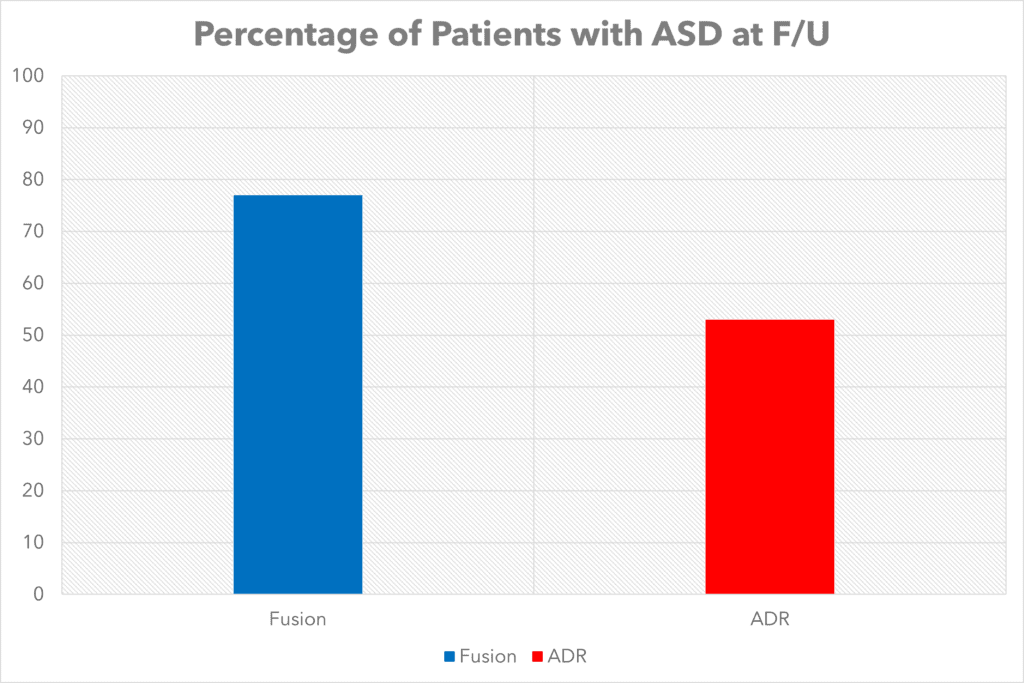
At the 7-year follow-up, 77% of patients with a fusion had ASD while 53% with a Pro-Disc-C ADR device had ASD. So right off the bat, while the ADR patients did better, still more than half of them have what the disc replacement fans claim will be avoided. So the promise of ADR wasn’t fully realized here.
When diving into that ASD data, we see that it’s an amalgamation of the degeneration in the levels above and below the ADR device. However, when you break that down, there was only a difference in ASD rate at the level above and NOT THE LEVEL BELOW. That’s a bit like pregnancy, in that if you get ASD, you’re likely going to need additional surgery, so there is no such thing as a little bit pregnant or a little bit of ASD. Hence, it’s likely that the future need for surgery due to the device (fusion or ADR) is the same.
Our authors then begin to play with the ASD progression data a bit by looking at the patients who got ASD by the amount of motion that the ADR device allowed. In ADR devices that allowed more motion, those patients were less likely to get ASD versus those that had less functional motion. However, as I’ve shown above, it doesn’t really matter because your likelihood of needing future surgery is probably the same as a whole. All this tells us is that some patients will get luckier than others and some will fare worse than others.
The conclusions? Even in a company-funded study, done by a guy who is getting paid big bucks by industry, digging deep behind the conclusion tells us that the rate of future surgery is likely going to be similar with a Pro-Disc-C and fusion. At the end of the day, that’s all my patients would care about.
RWD-Real World Data
I have seen more problems with ADR patients than I can count, but this week I captured this visual example of why patients who get these devices likely end up needing as much additional surgery as those who get fused:
If you look at the disc replacement level in the video above and observe how it moves, that’s much different than the normal disc above. As I often say, this isn’t rocket science, you can see what’s happening with your own eyes. The movement at these two levels is not the same.
The upshot? At the end of the day, I still don’t recommend either fusion or disc replacement for most of my patients who have nasty-looking MRI evidence of degenerative disc disease. Every once in a while we’ll see a patient who can’t be treated with interventional orthobiologics who needs surgery, but at this juncture, I can’t tell my patients with a straight face that a disc replacement surgery in their neck or back will be any better than a fusion.
__________________________________________________
References:
(1) MacDowall A, Canto Moreira N, Marques C, Skeppholm M, Lindhagen L, Robinson Y, Löfgren H, Michaëlsson K, Olerud C. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease and radiculopathy: a randomized controlled trial with 5-year outcomes. J Neurosurg Spine. 2019 Jan 11;30(3):323-331. doi: 10.3171/2018.9.SPINE18659. PMID: 30641852.
(2) Wachowski MM, Weiland J, Wagner M, Gezzi R, Kubein-Meesenburg D, Nägerl H. Kinematics of cervical segments C5/C6 in axial rotation before and after total disc arthroplasty. Eur Spine J. 2017 Sep;26(9):2425-2433. doi: 10.1007/s00586-017-5073-z. Epub 2017 Apr 4. PMID: 28378073.
(3) Yang X, Janssen T, Arts MP, Peul WC, Vleggeert-Lankamp CLA. Radiological follow-up after implanting cervical disc prosthesis in anterior discectomy: a systematic review. Spine J. 2018 Sep;18(9):1678-1693. doi: 10.1016/j.spinee.2018.04.021. Epub 2018 May 8. PMID: 29751126.
(4) MacDowall A, Skeppholm M, Lindhagen L, Robinson Y, Löfgren H, Michaëlsson K, Olerud C. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease with radiculopathy: 5-year outcomes from the National Swedish Spine Register. J Neurosurg Spine. 2018 Nov 2;30(2):159-167. doi: 10.3171/2018.7.SPINE18657. PMID: 30485205.
(5) Chang CC, Huang WC, Wu JC, Mummaneni PV. The Option of Motion Preservation in Cervical Spondylosis: Cervical Disc Arthroplasty Update. Neurospine. 2018 Dec;15(4):296-305. doi: 10.14245/ns.1836186.093. Epub 2018 Dec 14. PMID: 30545210; PMCID: PMC6347355.
(6) Gao X, Yang Y, Liu H, Meng Y, Zeng J, Wu T, Hong Y. A Comparison of Cervical Disc Arthroplasty and Anterior Cervical Discectomy and Fusion in Patients with Two-Level Cervical Degenerative Disc Disease: 5-Year Follow-Up Results. World Neurosurg. 2019 Feb;122:e1083-e1089. doi: 10.1016/j.wneu.2018.10.231. Epub 2018 Nov 9. PMID: 30415055.
(7) Spivak JM, Zigler JE, Philipp T, Janssen M, Darden B, Radcliff K. Segmental Motion of Cervical Arthroplasty Leads to Decreased Adjacent-Level Degeneration: Analysis of the 7-Year Postoperative Results of a Multicenter Randomized Controlled Trial. Int J Spine Surg. 2022 Feb;16(1):186-193. doi: 10.14444/8187. Epub 2022 Feb 17. PMID: 35177528.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.