What Is Degenerative Scoliosis?
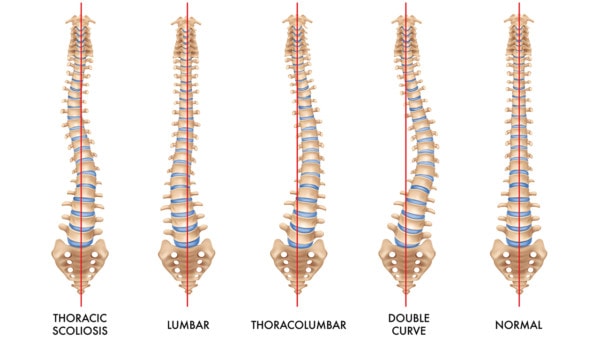
Types of scoliosis. Macrovector/Shutterstock
Degenerative scoliosis can become a big issue as people age. Today we’ll cover what this is and how we can help. We’ll also go over a patient who has had such a significant recovery without surgery that she’s almost hard to recognize now. Let’s dig in.
What Is Degenerative Scoliosis?
Degenerative means the arthritic wear and tear we all get as we age. Scoliosis means a side bend in the spine. Hence, degenerative scoliosis is when arthritis and degenerative disc disease cause the spine to bend sideways. This is also known as adult-onset scoliosis to differentiate it from the type of scoliosis commonly seen in adolescents during a growth spurt.
Degenerative scoliosis tends to cause not only back pain but also nerve pain down the leg. This happens when the facet joints on the inside of the curve get big and arthritic and the discs bulge, which can irritate nerves and cause sciatic symptoms down the leg. The back pain is often worse on one side and extends into the ribs. Patients may notice that their ribs are turned in one direction or the shoulder on one side is higher than the other.
What Is the Treatment for Degenerative Scoliosis?
Degenerative scoliosis can be treated with physical therapy or chiropractic, but when that fails to help, the patient is usually headed toward a multi-level fusion. While these patients can be treated with things like epidural steroid injections or radiofrequency ablation, these injection-based procedures usually fail to yield long-term results. When this doesn’t work, next up is often a fusion surgery. This is where the spine is bolted together with screws and rods. However, the problem here is that adjacent segment disease is often an issue. See my video below to learn more about that topic:
Can Degenerative Scoliosis be Reversed?
In short, no. Once this process begins, while certain types of injections discussed below may slow its progress, the only way to try to straighten the spine would be by using fusion surgery with long rods. However, straightening a young spine where the bones have yet to change shape is easier. In degenerative scoliosis, the shape of the bones has already changed, so there is really no practical way to straighten the spine, even with surgical fusion.
Can Degenerative Scoliosis Be Treated Without a Big Spine Surgery?
Lumbar fusion is a major surgery that carries with it significant risks of complications. As discussed above, a few non-surgical options are available, so let’s go over the most common ones offered:
- Epidural Steroid Injections – An injection of a high dose steroid into the area around the nerves to reduce nerve swelling and irritation.
- Steroid injections into facet joints – In this procedure a high dose steroid is injected into one or more painful and arthritic facet joints.
- Radiofrequency ablation – A probe is used to burn away the nerves that take the pain from the facet joints (1).
The issue with steroid injections is that they can damage the local tissue (2). In addition, in my clinical experience, none of the listed non-surgical approaches is very successful in helping patients avoid surgery.
A New Approach to Treating Degenerative Scoliosis
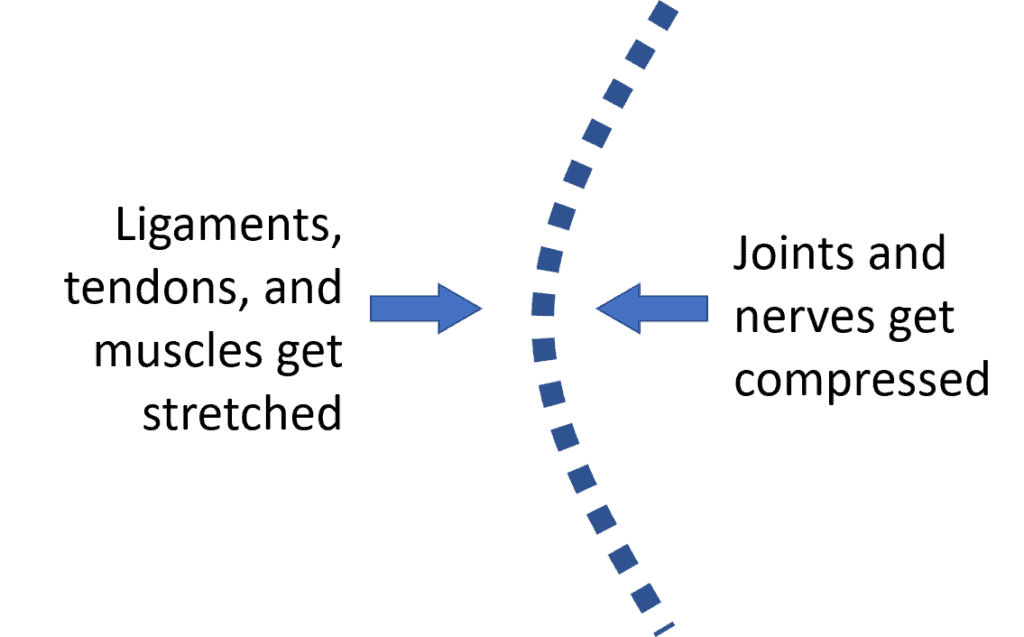
When the spine side bends, there is one side that’s compressed and one side that gets stretched. Hence, on the side of the compression (concavity), the joints and holes for the nerves (foramina) get extra forces which cause the joints to become big and arthritic and the spinal nerves to become irritated leading to sciatica. On the side of the stretching (convexity), the tendons get pulled on which leads to them getting beat up.
While the traditional pain management approaches above focus on finding one thing that’s causing pain, in degenerative scoliosis, it’s often many things that are causing pain. Hence, we developed a procedure that uses precise orthobiologic injections into many structures. So on the side of the concavity, we’re injecting into many facet joints and nerve areas that are getting compressed and on the side of the convexity, we’re injecting into all of those beat-up tendons. Orthobiologics are things like platelet-rich plasma or stem cells that may help these areas heal.
Functional Degenerative Scoliosis Treatment
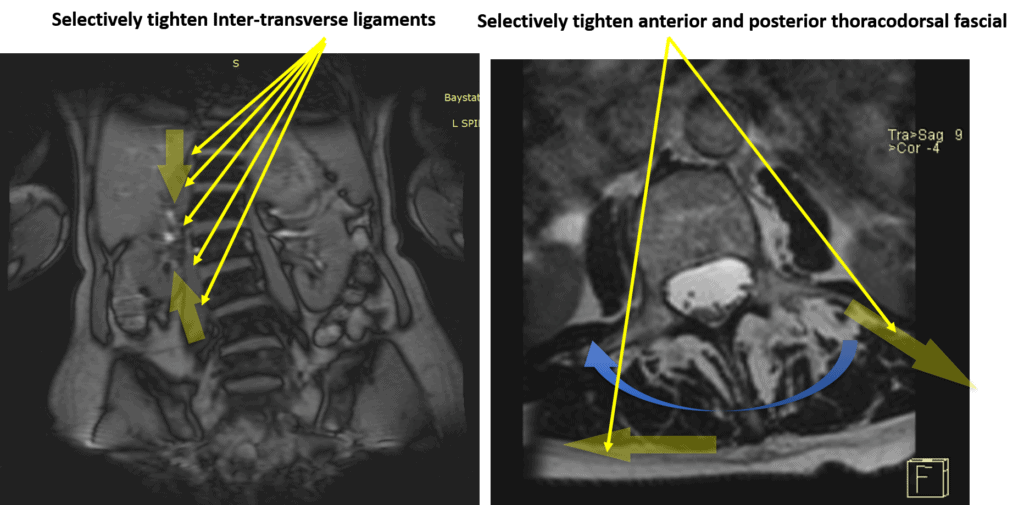
The problem with scoliosis is that the farther its side bent off-center, the more it wants to move in that direction. So while helping areas that hurt is great, what if we could buttress the ligaments and fascia in a precise way to provide support for the scoliosis? That’s the second part of this new procedure. These same orthobiologics can be used in a precise injection to target and tighten the ligaments and fascia.
For example, above on the left, we see a front view of the spine that side bends to the left of the image. There are ligaments there called inter-transverse that are being stretched that can be tightened with injection. On the right, we have a top view of the spine that shows a rotated vertebra. It’s not straight up and down because when the spine side bends in degenerative scoliosis, it also rotates. Here, we can selectively tighten one side of the fascia to reduce its ability to rotate.
To learn more about percutaneous scolioplasty, see my video below:
Patient Results
Freyda is an elderly woman with severe degenerative scoliosis. When she first came to me, she was in a wheelchair. She was just seen prior to her 4th platelet-based percutaneous scioloplasty procedure, which was delayed because of the pandemic. Her longest ability to walk before these procedures was from the elevator to her car in her building. On this trip, she brought her husband who needed a wheelchair in the airport while she walked. She now routinely walks 1/2 to 1 mile for exercise and is doing well. Each procedure has provided additional relief so she wants to continue until she plateaus out in her recovery.
The upshot? Degenerative scoliosis can wreak havoc and cause severe pain. While previously many patients ended up with surgery, we’ve now treated successfully many patients using percutaneous scolioplasty without surgery. Less invasive care means a quicker recovery and fewer complications. So click here to see if you’re a candidate for this breakthrough technology.
___________________________________________
References:
(1) Abejón D, Ortego R, Solís R, Alaoui N, del Saz J, del Pozo C. Trans-facet-joint approach to pulsed radiofrequency ablation of the L5 dorsal root ganglion in a patient with degenerative spondylosis and scoliosis. Pain Pract. 2008 May-Jun;8(3):202-5. doi: 10.1111/j.1533-2500.2008.00191.x. PMID: 18476897.
(2) McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA.2017;317(19):1967–1975. doi: 10.1001/jama.2017.5283

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.