What is Platelet Rich Fibrin Matrix? Something New or a Gimmick?
Credit: Shutterstock
I’ve been hearing quite a bit of buzz from patients and others in this space lately about Platelet-Rich Fibrin or Platelet-Rich Fibrin Matrix. Hence, let’s review what this is, how it differs from PRP, and if it’s something new and revolutionary or just a gimmick.
What is Platlet-Rich Plasma?
PRP is made when whole blood is centrifuged. There are many different ways to make PRP by varying the centrifuge speeds, the number of times the blood is centrifuged, and other methods. It’s made from concentrated platelets in plasma and can be manufactured with or without red and white blood cells.
Platelet-Rich Fibrin (Matrix) [PRFM]
Platelet-rich fibrin is created by making PRP and then activating it, usually with CaCl2. This creates a clot and forces growth factors out of the platelets. Usually, this clot is used surgically, as it can be sewn into an area. When this is done, it’s called Platelet-Rich Fibrin. However, a more recent trend is to create the clot in such a way that it can be injected and this is called Platelet-Rich Fibrin Matrix.
What are the stated advantages of injecting a clot? The advocates believe that it traps the platelets where you want them and it provides a healing matrix. However, why is all of this more hype than reality?
Why PRFM is a Gimmick
When PRP is injected, the platelets are naturally activated by free collagen (1). Free collagen means that there has been a local injury to the tissues, exposing collagen fibers from their normal tight bundles. Hence, if the doctor is injecting PRP into an area of injury or degeneration, the platelets are already getting activated and forming a local clot. Hence, activating the platelets with CaCl2 in a test tube before you inject isn’t needed.
There’s another serious problem with artificially pre-activating your PRP. In the study above, when researchers compared pre-activated PRP to naturally activated PRP caused by free collagen, the growth factor release of these two products was dramatically different:
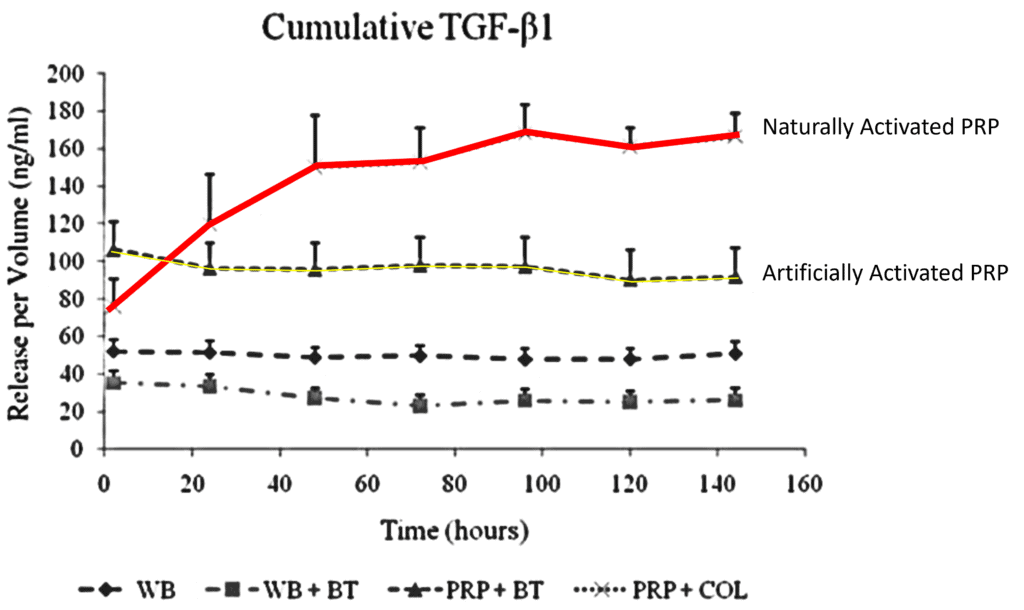
Credit: Harrison S, Vavken P, Kevy S, Jacobson M, Zurakowski D, Murray MM. Platelet activation by collagen provides sustained release of anabolic cytokines. Am J Sports Med. 2011 Apr;39(4):729-34. doi: 10.1177/0363546511401576. Epub 2011 Mar 11. PMID: 21398575; PMCID: PMC3176726.
The graph above shows that naturally activated PRP by collagen (red line) releases far more Transforming Growth Factor-beta (TGF-b) than artificially activated PRP (yellow line). Given that TGF-b is one of the main growth factors involved in healing, it would seem to make sense not to artificially activate your PRP, as you want as much of it as you can get.
In addition, if free collagen activates the PRP, it causes it to clot in the body, already trapping the platelets in the area. In addition, injecting PRP into a tendon or ligament will also trap the platelets locally, as these are fibrous structures. That’s why the standard of care is imaging guidance. Finally, in joints, since you want the PRP to circulate in the joint, having it stay in one spot or another is nonsensical. However, again, you can allow free collagen to activate the PRP if you’re trying to inject it into specific structures within the joint like a meniscus or ACL in a knee.
What if You Want Immediate Growth Factor Release?
We have observed that one of the downsides of PRP is that it can be pro-inflammatory. Obviously, in some patients, that means that injecting it around nerves can cause havoc (while in most patients this is tolerated). Hence, using platelet lysate (PL) for that application can reduce post-injection inflammation. PL is created using various methods to get all of the growth factors out of the platelets, so it has a much higher growth factor content than PRFM which uses one method (activation).
The upshot? IMHO PRFM is simply a way for manufacturers to try to come up with a new gimmick to sell more PRP kits. To the uneducated, it looks like a new thing, but to those who know PRP, it’s just a gimmick that likely reduces helpful growth factor release when compared to just letting the body’s free collagen activate PRP.
__________________________________________________
(1) Harrison S, Vavken P, Kevy S, Jacobson M, Zurakowski D, Murray MM. Platelet activation by collagen provides sustained release of anabolic cytokines. Am J Sports Med. 2011 Apr;39(4):729-34. doi: 10.1177/0363546511401576. Epub 2011 Mar 11. PMID: 21398575; PMCID: PMC3176726.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.