What’s Causing Your Side-of-Knee Pain? Let’s Focus on the Outside
On this page:
- Why does the side of my knee hurt?
- Ligaments
- Muscles and tendons
- Meniscus
- Nerves
- Knee arthritis
- What painkiller is best for knee pain?
Do you have pain on the side of your knee? All kinds of things may be going through your mind, but what could actually be causing it? Many things, including the tendons, the meniscus, the bone, or even the nerves can cause side of knee pain. In fact, the pain may not even relate to the knee itself as it may be from elsewhere. Today we’ll focus on the outside of the knee. So let’s explore.
Why Does the Side of My Knee Hurt?
The side of the knee has many structures that may hurt. We can place these into a couple of big categories:
- Ligaments
- Muscles and Tendons
- Meniscus
- Nerves
- Arthritis
Ligaments
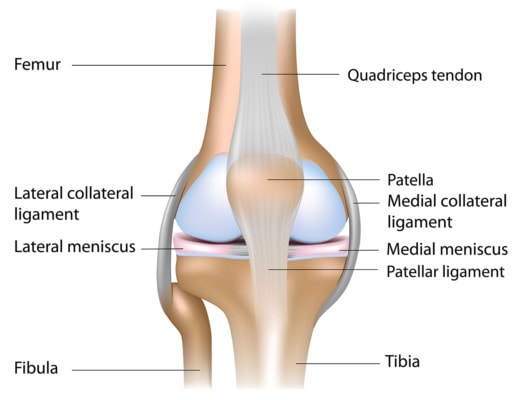
The outside of the knee has two main ligaments, the LCL and the ALL. These act like pieces of duct tape that hold the outside of the knee together. The LCL keeps the outside of the knee from gaping. The ALL is a newly discovered ligament that actually mimics the function of the ACL.
Hence, it helps to reduce rotation of the leg bone and reduces that bone’s ability to shift forward. While ligaments themselves may or may not be tender with injury, when the ligament is damaged, it allows too much motion, which can cause arthritis in the knee if left untreated. Importantly, most ligaments don’t require surgery but can be healed through precise injections of orthobiologics, like platelet-rich plasma or stem cells.
The LCL, or lateral collateral ligament, and the MCL, or medial collateral ligament, support side-to-side motion and stability in the knee. Front and back motion and stability are supported by the ACL, or anterior cruciate ligament, and the PCL, or posterior cruciate ligament.
While an acute injury to these ligaments due to sports, for example, can cause knee pain, it is also common for the ligaments to be lax due to an unaddressed old injury. The LCL and MCL live on the sides of the knee, so if you have a loose LCL, you may feel pain on the lateral, or outer side, of the knee, while if you have a loose MCL, you may feel pain on the medial, or inner side, of the knee.
There’s a test you can perform at home that can help you determine if you have laxity in either of the side knee ligaments. The test involves rotating the tibia (lower-leg bone) on the femur (the upper-leg, or thigh, bone). Learn more about this test and how to perform it by watching my video below:
If you do have loose knee ligaments, it’s important to address them as soon as possible as, over time, the instability in the knee joint created by the lax ligaments may lead to not only more knee pain but also knee arthritis with swelling.
What is the treatment for these ligaments? The average orthopedic doctor or surgeon doesn’t typically look for these knee ligament instabilities; he or she is typically focused only on the ligament condition or injury that can be operated on.
Again, we want to steer clear of surgery in most cases. Precise image-guided injections of your own platelets can help tighten up the knee ligaments, which should help relieve your knee pain, and your interventional orthopedics physician can accomplish this with precise image-guided injections.
Muscles and Tendons
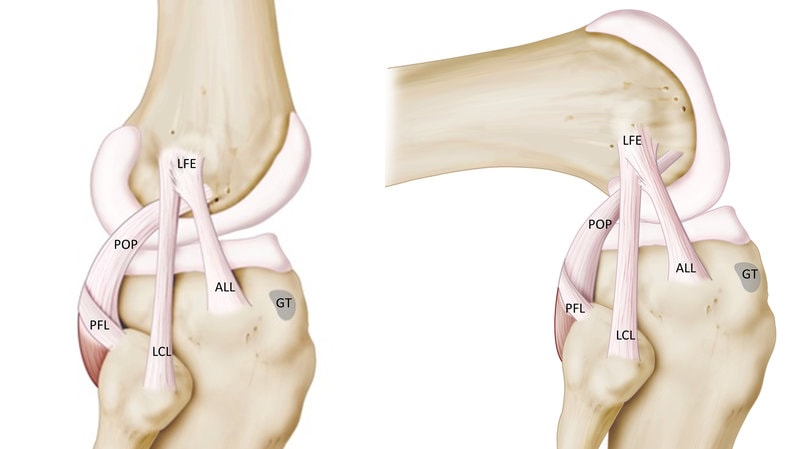
Studiovin/Shutterstock
There are actually a few key tendons on the side of the knee that may cause pain. The first you can actually see in the image above, labeled as “POP.” That’s the popliteus muscle at the back of your knee, which sends its tendon to the outside of the knee, under the ligaments we just discussed. This tendon often hurts when using that foot to take a boot or shoe off the opposite leg.
To the right, you see the back of the leg and the outside hamstrings muscle called the biceps femoris, which attaches to the outside leg bone called the fibula. This muscle can get tight and pull on this area, leading to the tendon getting degenerated and worn. Pain here tends to be lower in the outside of the knee or in the back of the outside of the knee. This would get worse when you try something like hamstring curls in the gym. Irritated low back nerves can also cause this problem, so if you have any back issues, take note.
Another really common cause of side of knee pain is the iliotibial band, or ITB. This starts way up at the side of the hip and travels down to attach on the outside front of the knee. If you’re someone who constantly needs to roll the side of your leg or “ITB,” then this pain could be caused by a worn tendon attaching at that spot.
To learn more about the ITB and what causes that issue, watch my short video below:
Meniscus
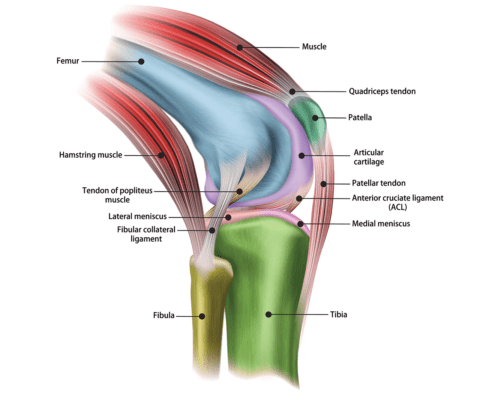
Alila Medical Media/Shutterstock
The side of the knee also contains the joint line, and cushion that’s called the meniscus. This is a figure-8 like structure that changes the shape of the otherwise flat tibia leg bone to match the curved femur or thigh bone. Hence, it acts as protection of the cartilage on the ends of the bone.
The meniscus can tear due to trauma when you’re young, or can tear just due to wear and tear as you age. While tears in patients under 30 due to trauma can cause pain, most tears detected on MRI in patients over 35 are like wrinkles, meaning they happen with normal aging and likely aren’t a source of pain.
While an MRI might show a meniscus tear in your knee joint, it can’t tell you if that meniscus tear is the diagnosis for your knee pain symptoms. Unfortunately, all too often, meniscus tears seen on MRI are the diagnosis determined for knee pain; however as previously stated, knee meniscus tears, especially in middle age and beyond, are as common as wrinkles (1). Many people have knee meniscus tears who have no knee pain, so we can’t assume in those who do have knee pain that a knee meniscus tear seen on an MRI is the diagnosis for the pain.
Once an MRI does confirm a knee meniscus tear, what should you do about it? First, don’t agree to treatment that involves surgery just based on your knee MRI. Meniscus repairs are one of the most common orthopedic surgeries performed today, and your doctor may recommend it for your tear or injury, yet if your doctor has not examined your back to rule out an irritated nerve condition, surgical treatment on the knee may not do you much good. Second, if you are middle age or older, meniscus tears are to be expected, so surgery in these cases should also be avoided (2). Let’s review a few issues associated with treatment that involves knee meniscus surgery:
- Studies have found that meniscus surgery is no better than physical therapy on pain symptoms and function outcomes (3).
- Meniscus “repair” is rarely a repair; it is actually an excision of pieces of the meniscus (i.e., meniscectomy), which may leave the cartilage in the knee joint vulnerable and more prone to arthritis symptoms, such as pain and swelling (4).
- Another study found that people without a diagnosis of arthritis who undergo meniscus surgery fare no better than those who have a sham surgery.
While there might be an occasional extreme case of knee pain with a meniscus tear that may need surgical treatment (such as knee locking due to the tear), these situations aren’t very common.
Nerves
Sometimes knee pain, including either the inner side (medial) of the joint or the outer side (lateral) of the joint, is actually due to an irritated nerve in the spine (6). Many people don’t realize that the nerves that exit the lumbar spine branch into the legs, reaching the knees, ankles, feet, and even the toes.
So an irritated lumbar nerve can be signaled as pain in any structure it supplies along the nerve branch. Evaluating the spine for a potential primary diagnosis for knee pain and symptoms is something a traditional doctor, who typically just focuses on the knee, often doesn’t do.
Poor biomechanics is another common issue that can cause knee pain and symptoms. Watch my video below, which shows my own poor biomechanics that caused my lateral meniscus to become pinched. What caused my lack of knee control in my knee? It was actually caused by a mildly irritated nerve in my low back. I didn’t have much back pain, but over time, the condition caused my stance to lack symmetry whenever I was running.
Knee Arthritis
Arthritis means that the cartilage in your knee is wearing out, and the bones begin to change shape to form what we call osteophytes, also known as bone spurs. When this happens, you can get pain at the side of the knee near the joint line.
For the outside, this could be arthritis between the knee cap and the end of the thigh bone (femur) or the main knee joint where the thigh and leg bones meet. Another possible spot for arthritis is where the side smaller leg bone (fibula) meets the larger leg bone (tibia).
Many patients with arthritis are often offered a steroid shot. DO NOT ALLOW THIS INJECTION as recent high-level research demonstrates that a steroid shot kills the remaining cartilage in the knee (7). Other possibilities include gel shots, like Synvisc or hyaluronic acid. These shots can help cushion the joint and reset the bad chemical environment. They don’t seem to harm cartilage and can help for six months to a year.
Using an injection of your own blood platelets called platelet-rich plasma has been shown to be better than these gel shots at reducing pain and may even help your damaged cartilage. Finally, for more severe arthritis, an injection of your own stem cells may be the answer.
What Painkiller Is Best for Knee Pain?
Seeking interventional orthopedics treatments to address the source of your knee pain and injury should be the specific goal. If a painkiller is needed in the meantime, ditch the nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and swelling and all of their dangerous side effects and opt for supplements that have been shown to be effective for knee pain and swelling in the joint, including curcumin, glucosamine, and chondroitin (8, 9, 10).
What about steroid injections for knee pain and swelling? Just don’t do it! There is a long list of toxic side effects associated with these drugs, including spinal fracture risk, vaginal bleeding, adrenal problems, joint cartilage loss (toxicity to cartilage), diminishing relief with each injection, and so much more (11).
The upshot? You can likely diagnose your own cause of side of knee pain. Just realize that almost everything I’ve discussed above doesn’t require a big surgery to fix. Instead, highly precise injections of our own platelets or stem cells can usually heal these problems with minimal downtime.
However, be cautious out there as you’ll find lots of clinics that know very little about treating these issues and that want to charge big bucks to inject magic amniotic or umbilical cord stem cells in this area and then often IV. This is not legit treatment as these are dead tissues being hawked as live stem cells. So buyer beware!
__________________________________________________
References
(1) Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study). doi:10.1136/bmj.e5339
(2) Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515-2524. doi:10.1056/NEJMoa1305189
(4) Lee DY, Park YJ, Kim HJ, et al. Arthroscopic meniscal surgery versus conservative management in patients aged 40 years and older: a meta-analysis. Arch Orthop Trauma Surg. 2018;138(12):1731-1739. doi:10.1007/s00402-018-2991-0
(5) Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515-2524. doi:10.1056/NEJMoa1305189
(6) Iijima H, Suzuki Y, Aoyama T, Takahashi M. Interaction between low back pain and knee pain contributes to disability level in individuals with knee osteoarthritis: a cross-sectional study. Osteoarthritis Cartilage. 2018;26(10):1319-1325. doi:10.1016/j.joca.2018.06.012
(7) McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA. 2017;317(19):1967-1975. doi:10.1001/jama.2017.5283
(8) Kaufman DW, Kelly JP, Battista DR, Malone MK, Weinstein RB, Shiffman S. Exceeding the daily dosing limit of nonsteroidal anti-inflammatory drugs among ibuprofen users. Pharmacoepidemiol Drug Saf. 2018;27(3):322-331. doi:10.1002/pds.4391
(9) Kuptniratsaikul V, Dajpratham P, Taechaarpornkul W, et al. Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: a multicenter study. Clin Interv Aging. 2014;9:451-458. Published 2014 Mar 20. doi:10.2147/CIA.S58535
(10) Zhu X, Sang L, Wu D, Rong J, Jiang L. Effectiveness and safety of glucosamine and chondroitin for the treatment of osteoarthritis: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2018;13(1):170. Published 2018 Jul 6. doi:10.1186/s13018-018-0871-5
(11) Chon JY, Moon HS. Salivary cortisol concentration changes after epidural steroid injection. Pain Physician. 2012;15(6):461-466.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.