Why Your Head Feels Heavy
On this page:
- What holds the head on?
- How do you know if you have these problems?
- How do you treat heaviness of the head?
Picture your head as a bowling ball balanced on the end of a stick (the spine). There are muscles at the top of the neck as well as in the front and back which help hold the bowling ball on the stick. When the natural curve in the neck is no longer there due to muscle weakness, this can push the bowling ball forward on the stick, which is why your head feels heavy.
The muscles and ligaments in the spine help provide stability. The ligaments are only one half of the joint stability equation acting like duct tape to hold the body together. The deep muscles take on the other half of the joint stability equation which helps keep the spine aligned while allowing the spine to twist and bend.
What Holds the Head On?
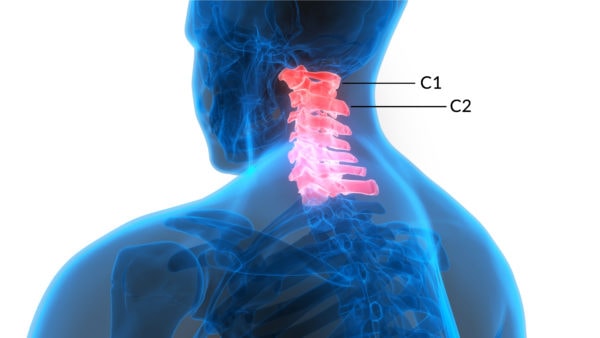
The alar and transverse ligaments are found in the upper neck and are responsible for holding the head on. The alar ligaments reach up from the C2 vertebra and attach strongly to the skull, while the transverse ligaments hold the pivot point of the C2 vertebra tightly to the C1 bone, allowing the head to turn without getting a spinal cord injury.
The accessory ligaments connect C1-C2 and run up the side of the dens (the toot-like process of C2). The vertebrodural ligament (VDL) is a newly discovered ligament at the back of the neck between C1 and C2 that connects straight into the dura (the covering of the spinal cord), hence it’s implicated in headaches.
Magic Mine/Shutterstock
How Do You Know if You Have These Problems?
Many years ago, Jim Elliott, PhD. and I wondered if the deep muscle in the upper cervical spine suffer atrophy as a result of an injury as it does in the low back multifidus muscle in many patients with chronic low back pain. We discovered through upper neck MRIs (Magnetic resonance imaging) that the upper neck muscles do atrophy in patients with head and neck trauma like whiplash or when something hits the head causing upper neck injury.
The research that supports this concept was developed by Jim Elliott, PhD. Basically, the upper neck muscles help to stabilize the head on the neck. When the upper neck is injured (often the facet joints and ligaments get damaged), the muscles shut down and begin to atrophy (1, 2, 3).
As they shrink they can no longer support the head and keep it stable (hence the “heavy head” feeling). This instability of the head on the neck causes the spinal discs, joints, nerves, and muscles to get beat up over time-leading to headaches. The injury of the upper neck joints and ligaments that began the atrophy can also cause headaches.
When I see a traumatic neck injury patient with headaches, I ask the patient to lift their hands above their head. They often can’t do this, or it’s difficult. I then hold their head still with my hands, acting like their upper neck stabilizer muscles.
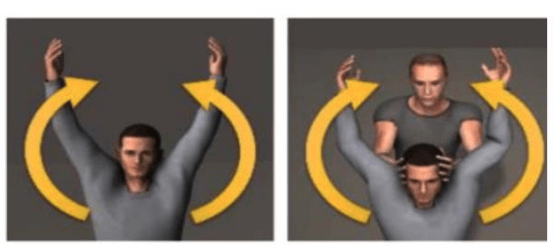
When they try again, it’s often easier for them to lift their arms when someone stabilizes the head. Why? The stabilization of the head gives the upper trapezius a solid base of support to pull from as the arms are lifted. Without that support in a patient with atrophied and weak upper neck muscles, the upper trapezius works harder to both stabilize the head and lift the arms.
Another way to help determine the cause of a patient’s head feeling heavy is through an MRI or DMX (Digital Motion X-ray). An MRI can visualize the alar, transverse, and accessory ligaments. If the doctor wants to see the accessory ligaments, they are harder to visualize so a 3T magnet will help MRI machines come in various field strengths which tie back to the quality of the picture and the best you can get right now is a 3T (4, 5).
A DMX is a newer study DMX stands for Digital Motion X-ray. This means that the doctor will place you in a seated position and ask you to move your neck around while a video x-ray is taken and recorded. Your doctor may use this to see if the neck bones move too much. This can indicate that the ligaments holding the neck bones together may be damaged.
How Do You Treat Heaviness of the Head?
First, you have to get rid of the pain in the damaged joints-we use biologic injections like platelets and stem cells to help the joints. Sometimes the ligaments have to be injected as well to help strengthen the neck and relief some pain.
A slow and gentle strengthening program is a good place to start (we start the patient using an adapted iPad game where their head movements have to guide a ball through a maze). The patient can then transition into a program where there’s more force used. We like the BTE Multi-cervical unit for this part.
If neck strengthening doesn’t help, the next step could be injecting the ligaments with stem cells. There is a new procedure that can directly inject the ligaments that hold the head on. That’s called the PICL procedure. During a PICL procedure, bone marrow concentrate that contains a stem cell fraction is injected into the CCJ (cranio-cervical junction) ligaments.
In order to reach these ligaments, the procedure is performed through the back of the throat. While a patient is under full anesthesia, a mouth piece is placed to help keep the mouth open and tongue depressed during the procedure. The back of the throat is then injected with local anesthetic to keep the patient as comfortable as possible. In order to get a good view of these ligaments, the injections are guided with real time x-ray to ensure the correct ligaments are being injected.
_____________________________________________
References
(1) Elliott JM, Pedler AR, Jull GA, Van Wyk L, Galloway GG, OʼLeary SP. Differential changes in muscle composition exist in traumatic and nontraumatic neck pain. Spine (Phila Pa 1976). 2014 Jan 1;39(1):39-47. doi:10.1097/BRS.0000000000000033
(2) Elliott JM. Are there implications for morphological changes in neck muscles after whiplash injury? Spine (Phila Pa 1976). 2011 Dec 1;36(25 Suppl):S205-10. doi:10.1097/BRS.0b013e3182387f57
(3) Elliott JM, O’Leary S, Sterling M, Hendrikz J, Pedler A, Jull G. Magnetic resonance imaging findings of fatty infiltrate in the cervical flexors in chronic whiplash. Spine (Phila Pa 1976). 2010 Apr 20;35(9):948-54. doi:10.1097/BRS.0b013e3181bb0e55
(4) Yuksel M, Heiserman JE, Sonntag VK. Magnetic resonance imaging of the craniocervical junction at 3-T observation of the accessory atlantoaxial ligaments. Neurosurgery. 2006 Oct;59(4):888-92; discussion 892-3. doi:10.1227/01.NEU.0000232661.24547.06
(5) Krakenes J, Kaale BR. Magnetic resonance imaging assessment of craniovertebral ligaments and membranes after whiplash trauma. Spine (Phila Pa 1976). 2006 Nov 15;31(24):2820-6. doi:10.1097/01.brs.0000245871.15696.1f

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.