Understanding Atypical Trigeminal Neuralgia

Medically Reviewed By:
Atypical trigeminal neuralgia (TN2) is a complex and often misunderstood condition that can severely impact an individual’s quality of life. Unlike typical trigeminal neuralgia or TN1, which causes sudden, severe, and sharp facial pain, TN2 presents with constant burning or aching pain that can be harder to diagnose and treat.
This article will guide you through the basics of TN2, explore common misconceptions, and provide insight into how proper diagnosis and treatment can make a significant difference.
Many patients with trigeminal neuralgia explore less invasive treatment options. While brain surgery is sometimes recommended, physicians within the licensed Regenexx network offer alternative therapies that do not require invasive procedures.
This article explores the complexities of this condition as well as a case where a patient was diagnosed with TN2 but, upon further evaluation, did not fit that diagnosis.
What Is Atypical Trigeminal Neuralgia (TN2)?
TN2 is a chronic pain disorder affecting the trigeminal nerve, but it differs significantly from the more well-known form of trigeminal neuralgia. While TN1 is characterized by sudden, sharp, and electric shock-like facial pain, TN2 presents a more constant, dull, or burning pain.
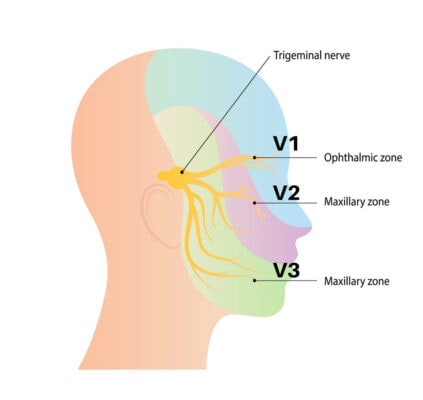
This persistent discomfort can occur in the forehead (V1), cheek (V2), or jaw (V3), corresponding to the three branches of the trigeminal nerve. The intensity of TN2 pain may fluctuate, making diagnosis and treatment more difficult.
TN2 is less responsive to typical triggers, such as light touches or stimulation, which often provoke intense episodes in TN1. Instead, TN2 presents a deeper, more prolonged discomfort, frequently described as an aching or burning sensation. This difference in pain type and duration contributes to the challenges of managing TN2 and often leads to confusion in diagnosis.
Patients with TN1 experience disabling nerve pain that can be shocking, tingling, or hypersensitive. Even mild stimulation from brushing the face can trigger severe pain. TN2 differs from this classic presentation in that the pain is persistent and less episodic. Both conditions, however, involve the hypersensitive trigeminal nerve.
Common names for trigeminal neuralgia include:
- Tic douloureux
- Fothergill disease
- TN (abbreviation)
- Trifacial neuralgia
Understanding the nuances between TN2 and TN1 is crucial for accurate diagnosis and effective treatment.
Classifying Trigeminal Neuralgia
There are two types of trigeminal neuralgia: classical trigeminal neuralgia (TN1), and atypical trigeminal neuralgia (TN2), also known as ATN. Pain associated with TN1 is sudden, intense, and electric shock-like, whereas pain associated with TN2 is more constant and diffused.
TN2 is sometimes used as a broad classification for facial pain that does not clearly align with TN1, which may make it more challenging for patients to receive a precise diagnosis and customized treatment.
- Type Of Pain: TN1 involves sharp, stabbing pain, while TN2 is a constant, burning, or aching pain.
- Duration: TN1 pain occurs in brief episodes, while TN2 causes continuous discomfort with varying intensity.
- Triggers: TN1 pain can be triggered by touching, eating, or talking, while TN2 is less dependent on external stimuli, making it more difficult to manage.
Root Causes Of Atypical Facial Pain In Trigeminal Neuralgia
TN2 may result from several underlying factors that affect the trigeminal nerve differently than TN1. These causes include nerve damage, injury, or compression, leading to chronic facial pain.
Nerve Damage Or Injury
It is common in TN2 for the trigeminal nerve to suffer damage or injury, resulting in chronic pain. This may occur from trauma, dental procedures, or surgical complications affecting the facial nerves.
- Trauma To The Face Or Head: Injuries can damage the trigeminal nerve, resulting in chronic pain resembling TN2.
- Dental Procedures: Dental work, such as root canals or extractions, may inadvertently injure the nerve, causing ongoing facial discomfort.
- Surgical Complications: Procedures near the trigeminal nerve may lead to nerve damage, contributing to persistent pain.
Vascular Compression Of The Trigeminal Nerve
Vascular compression occurs when blood vessels press against the trigeminal nerve, leading to irritation and pain. This is a common cause in TN1 but can also contribute to the development of atypical facial pain.
- Blood vessels pressing against the nerve: Similar to TN1, blood vessels may compress the trigeminal nerve, causing ongoing irritation and pain.
Secondary Conditions Mimicking TN2 Symptoms
Several conditions can mimic the symptoms of TN2, complicating the diagnostic process:
- Craniocervical instability (CCI): This condition occurs when the ligaments holding the head to the upper neck are loose or damaged, irritating the trigeminal nerve.
- Temporomandibular joint (TMJ) disorders: TMJ dysfunction can cause pain that spreads to the trigeminal nerve’s branches, mimicking TN2 symptoms.
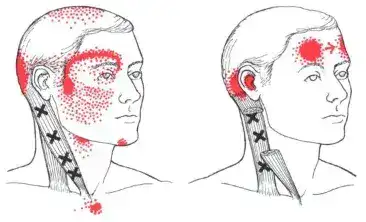
- Trigger points in facial or neck muscles: These are persistent areas in muscles that remain tense and weak, sending pain to different regions. The diagram above shows the referral pattern for trigger points in the sternocleidomastoid muscle, with the left side corresponding to V1 and V2 pain (shown in the previous diagram).
- TCN – transverse cervical nerve (superficial cervical plexus): This nerve complex is located beneath the SCM and provides sensation to the skin below V3 (highlighted in bright yellow as TCN in the previous diagram). Issues with this nerve can sometimes be mistaken for atypical trigeminal neuralgia.
Underlying Nerve Issues Leading to Misfiring
- Nerve degeneration or demyelination: Conditions like multiple sclerosis may damage the protective myelin sheath around the nerve, leading to chronic pain.
- Chronic inflammation: Long-term inflammation, whether from infection, injury, or autoimmune conditions, can lead to persistent nerve misfiring.
Indications And Symptoms Of Atypical Facial Pain
Atypical facial pain in TN2 presents with distinct symptoms that differ from TN1:
- Constant aching or burning pain: This pain is a continuous, dull sensation that may feel like burning. It lingers without change, affecting daily comfort.
- Less intense but persistent pain: This mild but unrelenting pain can disrupt daily activities. It often remains even when at rest.
- Persistent, diffused pain: TN2 is characterized by a more constant, dull, or burning pain that is less sharp but spreads over a larger area than TN1.
- Referred pain: Pain may radiate from the initial site to other areas. It can cause a wider region of discomfort or sensitivity.
- Deeper, prolonged discomfort: TN2 causes a more persistent aching or burning sensation, often lasting longer and creating a deeper sense of discomfort than TN1.
Diagnosing TN2 From Other Conditions
Diagnosing TN2 requires a thorough examination and the exclusion of other potential causes of facial pain. This process involves reviewing the patient’s pain characteristics, using imaging techniques to rule out other conditions, and comparing symptoms with similar disorders like TMJ, migraines, and TN1.
Below are key steps that help in correctly diagnosing TN2.
- Review pain characteristics (type, duration, location): Understanding the kind of pain (constant, aching, or burning), its duration (persistent vs. episodic), and its location (V1, V2, V3 regions) is essential for differentiating TN2 from other conditions.
- Use MRI or CT to rule out other conditions: Imaging such as MRI or CT scans can help rule out other structural issues, such as tumors or vascular compression, that may be causing facial pain. These tests are crucial for ensuring there are no other underlying causes.
- Physical exam for touch sensitivity or pain triggers: A physical exam can assess the patient’s sensitivity to touch or the presence of triggers. In TN2, pain is typically less triggered by external stimuli, whereas TN1 pain may be exacerbated by simple touch or movement.
- Compare symptoms with TMJ, migraines, and TN1: Symptoms of TN2 often overlap with TMJ disorders, migraines, or TN1. Comparing the patient’s pain with these conditions helps narrow down the diagnosis. TMJ-related pain may be more localized to the jaw, and migraine pain typically includes other headache-related symptoms.
- Analyze response to previous treatments: Reviewing how a patient has responded to past treatments, such as medications or dental procedures, can provide valuable clues. If standard treatments for TN1 or TMJ have not been sufficient, TN2 may be a more likely diagnosis.
In a recent case, a patient presented with right facial pain in the V2/V3 region but lacked the typical nerve hypersensitivity associated with TN2. Her pain began after a dental procedure, and her symptoms included occipital headaches, which further complicated the diagnosis.
Through a careful physical examination, it was discovered that her TMJ was tender, and she showed signs of craniocervical instability (CCI) due to hypermobility, which was likely causing her facial pain. This scenario highlights the importance of thoroughly assessing each aspect of the patient’s condition to avoid a misdiagnosis of TN2.
Standard Treatment Of Atypical Trigeminal Neuralgia
Treating TN2 involves medication, less invasive procedures, and, in some cases, surgical intervention:
- Anticonvulsants: Drugs like gabapentin (Neurontin) and carbamazepine (Tegretol) are often prescribed to help calm nerve activity and reduce pain.
- Muscle relaxants: Muscle relaxants can alleviate muscle-related pain, especially if TN2 symptoms overlap with TMJ disorders.
- Botox: Botox can reduce pain by relaxing muscles and blocking nerve signals in the affected areas and can relieve the constant burning or aching pain associated with TN2.
- Gamma knife radiation (or stereotactic radiosurgery): This is a targeted treatment using focused radiation to disrupt pain signals by damaging the trigeminal nerve without incision.
- Balloon compression: In this procedure, a balloon is inserted and inflated near the nerve to compress it, which can relieve pain for an extended period.
- Radiofrequency ablation (RFA): RFA involves using heat from radio waves to destroy a portion of the trigeminal nerve, disrupting the transmission of pain signals.
- Microvascular decompression (MVD): MVD involves relocating or removing blood vessels compressing the trigeminal nerve.
The Regenexx Approach To Atypical Trigeminal Neuralgia
Physicians in the licensed Regenexx network conduct thorough evaluations, including advanced imaging, to assess factors contributing to TN2. Interventional orthobiologic procedures may be considered as part of a personalized care plan to support nerve function and help manage symptoms.
Proper Diagnosis Is Critical For Proper Treatment
A precise diagnosis is essential for developing the most suitable treatment plan for TN2. Because its symptoms can overlap with conditions such as temporomandibular joint disorders, migraines, and craniocervical instability, a thorough evaluation is necessary.
Healthcare providers may use physical examinations, imaging, and a detailed medical history review to identify contributing factors. A comprehensive diagnosis can help determine the most appropriate approach, whether through medications, non-surgical procedures, or other interventions.
Patients may avoid unnecessary treatments and misdiagnoses by accurately diagnosing the condition. Consult with a physician in the licensed Regenexx network to explore interventional orthobiologic options for managing atypical trigeminal neuralgia.
References
(1) Weiss, A.L., Ehrhardt, K.P. & Tolba, R. Atypical Facial Pain: a Comprehensive, Evidence-Based Review. Curr Pain Headache Rep 21, 8 (2017). https://doi.org/10.1007/s11916-017-0609-9
(2) Manzoni GC, Torelli P. Epidemiology of typical and atypical craniofacial neuralgias. Neurol Sci. 2005 May;26 Suppl 2:s65-7. doi: 10.1007/s10072-005-0410-0. PMID: 15926023.

Medically Reviewed By:
