What You Need To Know About Iliotibial Band Syndrome (ITBS)

Medically Reviewed By:
Iliotibial band syndrome (ITBS) may interfere with daily activities, making simple movements like walking, running, climbing stairs, or standing for extended periods more difficult. Over time, individuals with ITBS may experience reduced mobility and physical activity, which can impact overall health and well-being.
This article explains how ITBS develops, outlines common symptoms, describes diagnostic methods, and reviews options that may promote improved function and mobility.
Understanding The Iliotibial Band And Its Role In Mobility

The iliotibial band (ITB) is a thick band of connective tissue that runs along the outside of the thigh. It helps stabilize the hip and knee joints during movement. Many individuals report discomfort associated with the ITB, which has made activities like foam rolling the outer thigh common in gyms and rehabilitation programs.
The ITB connects to the gluteus maximus and tensor fasciae latae (TFL) muscles near the hip. These muscles support pelvic stability during activities such as walking or running. When one leg supports the body and the opposite foot lifts off the ground, the ITB and its associated muscles help prevent the pelvis from tilting downward.
Weakness in the gluteus maximus or TFL muscles can reduce stabilizing tension along the ITB. Some research in runners suggests that individuals with hip muscle weakness may exhibit altered movement patterns, such as increased hip adduction and knee internal rotation, which can place additional strain on the ITB during daily activities.[1] Over time, this repeated strain may contribute to irritation, tightness, or discomfort along the outer thigh.
Proper nerve function is important in the health of the ITB. Irritation of nerves in the lower back, even without noticeable back symptoms, may weaken the muscles that support the ITB. The L4, L5, and S1 nerve roots send important signals to these muscles, and disruption of these signals can impair stability during movement.
Additional information about the relationship between nerve health and ITB function is available in the video below.
How The IT Band And Vastus Lateralis Interact In ITBS
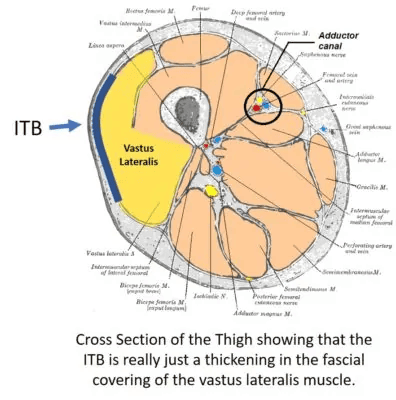
The ITB does not function alone. It works closely with nearby muscles, particularly the vastus lateralis and the biceps femoris. As shown in the diagram below, the vastus lateralis runs along the outer thigh, while the biceps femoris sits behind the ITB.
The fascia, a strong connective tissue that helps maintain structure and support efficient muscle contraction, surrounds the muscles. Fascia also connects neighboring muscles, creating a continuous network that transmits force and movement.
Due to these connections, dysfunction or tightness in one muscle group can affect others. Increased tension in the vastus lateralis or biceps femoris may place additional strain on the ITB, which can contribute to the development or worsening of symptoms associated with iliotibial band syndrome.
What Is Iliotibial Band Syndrome?
ITBS occurs when the ITB becomes irritated due to repeated friction as it moves over the outer structures of the knee. This ongoing rubbing may cause inflammation and discomfort, particularly during activities that involve frequent bending and straightening of the knee, such as running, cycling, or climbing stairs.
Irritation typically develops where the ITB crosses the lateral femoral epicondyle, a bony prominence on the outside of the thigh bone near the knee. Persistent friction in this area can lead to symptoms such as tenderness, aching, or sharp sensations along the outside of the knee or thigh.
Although ITBS often affects one leg, a variation called bilateral iliotibial band syndrome may impact both legs. Bilateral ITBS can make movement more difficult and may slow recovery. While less common, this condition may develop in individuals with biomechanical imbalances or those who perform repetitive activities involving both legs.
Recognizing the differences between unilateral and bilateral ITBS can help individuals identify early symptoms and understand potential contributing factors.
Common Triggers Behind IT Band Tightness And Discomfort
Tightness and discomfort along the outer thigh often result from a combination of structural, muscular, and movement-related factors. Understanding the common triggers behind ITB irritation may help identify areas that could benefit from targeted intervention.
Several factors can contribute to excessive tension or strain on the ITB. These issues may place additional stress on the band itself or on the muscles and fascia that support it. Recognizing these triggers is crucial in managing symptoms and promoting healthier movement patterns.
Common factors that may contribute to ITB tightness and discomfort include:
Overuse And Repetitive Motion
Frequent bending and extending of the knee during activities such as running, cycling, or stair climbing can place repeated strain on the ITB. Without adequate rest or variation in movement, ongoing stress may irritate the surrounding tissues.
This irritation can increase tightness, contribute to inflammation, and lead to symptoms along the outer thigh. Over time, accumulated strain may promote the development of ITBS.
Muscle Imbalances
Muscle imbalances around the hip and thigh can create uneven forces that strain the ITB. Weakness in muscles such as the gluteus maximus or gluteus medius may cause other structures to compensate, increasing tension along the ITB during movement.
Over time, these imbalances may irritate the tissues surrounding the ITB, leading to tightness, discomfort, and reduced mobility. Strengthening the supporting muscles can promote better alignment and help reduce strain along the outer thigh.
Overpronation Of The Foot
Overpronation occurs when the foot rolls inward excessively during walking or running. This altered movement pattern can disrupt the alignment of the leg and hip, placing additional strain on the ITB.
As the foot collapses inward, the knee may shift medially, which can increase tension along the ITB. Over time, this mechanical stress may contribute to irritation, tightness, and discomfort along the outer thigh, particularly during repetitive activities.
Weakness In The Hip Abductors
The hip abductors, including the gluteus medius and gluteus minimus, play a critical role in stabilizing the pelvis during movement. Weakness in these muscles can reduce support for the hip and knee, placing additional tension on the ITB.
When the hip abductors fail to maintain proper alignment, the pelvis may drop toward the unsupported side during walking or running. This imbalance can increase strain on the ITB and may contribute to tightness, irritation, and discomfort along the outer thigh.
Pre-existing Iliotibial Band Tightness
Tightness in the ITB can develop gradually due to previous injuries, chronic muscle imbalances, or repetitive activities. When the ITB remains tight over time, it may become more vulnerable to irritation and strain during everyday movements.
Pre-existing tension can limit the ITB’s ability to glide smoothly over the structures of the hip and knee. This restriction may contribute to ongoing discomfort, reduced flexibility, and an increased likelihood of developing symptoms associated with ITBS.
Signs And Symptoms To Be Aware Of
Recognizing the signs and symptoms of ITBS is essential in identifying the condition early and addressing contributing factors. Symptoms often develop gradually and may worsen with continued activity.
Irritation of the ITB typically causes discomfort along the outer thigh or knee. In some cases, symptoms may limit mobility or reduce participation in physical activities. Early identification can help guide management strategies and may lower the risk of further irritation.
Common signs and symptoms of ITBS include:
Dull Ache, Burning, Or Tenderness
Individuals with ITBS often report a dull ache, burning sensation, or tenderness along the outer side of the knee or thigh. These symptoms may intensify during physical activities that involve repetitive knee motion, such as running, cycling, or climbing stairs.
Localized tenderness is often noticeable when pressing along the length of the ITB, particularly near the knee. In some cases, discomfort may continue during periods of rest, especially following extended activity.
Clicking, Popping, Or Snapping Sensation
A clicking, popping, or snapping sensation along the outside of the knee is a common symptom associated with ITBS. These sensations often occur as the ITB moves over nearby bony structures during activities that involve repeated knee bending and straightening.
The snapping feeling may become more noticeable with repetitive movements such as running, squatting, or climbing stairs. Although it may not cause significant discomfort initially, ongoing friction can contribute to irritation and increased symptoms over time.
Pain Radiating Down The Leg
In some cases, ITBS may cause pain that radiates from the outer hip or knee down the side of the leg. This discomfort often follows the path of the ITB and can vary in intensity based on activity level.
Radiating pain may worsen during repetitive knee movements, prolonged standing, or downhill walking and running. If left unaddressed, ongoing discomfort can alter movement patterns and place additional strain on surrounding structures.
- Side-Of-Knee Pain: Pain on the side of the knee may result from ligament injuries, iliotibial (IT) band syndrome, or meniscus issues. Accompanying symptoms can include tenderness, swelling, and discomfort, often worsening with movement or prolonged activity. Read More About Side-Of-Knee Pain.
- Knee Locking Up: Knee locking may result from a meniscus tear, cartilage damage, or joint inflammation, causing temporary immobility or stiffness. It can make bending or straightening the knee difficult, sometimes accompanied by pain or swelling. Read More About Knee Locking Up.
When To Seek Medical Attention
While many cases of ITBS may improve with activity modification and rehabilitation, some situations require medical evaluation. A physician should assess persistent symptoms that do not respond to rest, stretching, or strengthening exercises.
Medical attention is also recommended if pain intensifies, radiates beyond the thigh or knee, or interferes with daily activities. Signs of significant swelling, redness, or warmth that do not improve may suggest more advanced tissue irritation that requires further investigation.
In addition, symptoms that suggest nerve involvement, such as numbness, tingling, or weakness in the leg, should be evaluated by a physician. Early assessment may help guide management strategies and reduce the risk of long-term mobility limitations.
How To Diagnose ITBS
Diagnosing ITBS typically begins with a detailed clinical evaluation. A physician considers the individual’s medical history, activity level, and specific symptom patterns. Common steps in the diagnostic process include:
- Medical History Review: Identifying the onset of symptoms, activity patterns, and any previous injuries.
- Physical Examination: Palpating the ITB to assess tenderness, particularly near the knee.
- Movement Testing: Evaluating alignment, stability, and symptom reproduction during activities such as walking, squatting, or single-leg exercises.
- Imaging Studies: Using ultrasound or MRI to help rule out other conditions and assess for tissue irritation or inflammation.
An accurate diagnosis focuses on detecting ITB irritation and identifying biomechanical factors that may contribute to ongoing symptoms.
Common Treatment Approaches To ITBS
Managing ITBS often involves a combination of strategies designed to reduce irritation, improve flexibility, and address underlying biomechanical factors. Early intervention may help prevent symptoms from becoming more persistent or severe.
Treatment plans are typically customized based on symptom severity and contributing factors. A variety of non-surgical options are available to promote improved function and help reduce strain on the ITB. Common treatment approaches for ITBS include:
RICE Method
Physicians often recommend the RICE method—rest, ice, compression, and elevation—during the early stages of ITB irritation. This approach may help manage inflammation and reduce undesirable symptoms after activities that place strain on the outer thigh.
Applying ice to the affected area, using compression wraps, and elevating the leg can assist in minimizing swelling. Resting from aggravating activities allows tissues to begin recovering and may help reduce further strain on the iliotibial band.
Orthotics
Orthotic devices may help improve foot and leg alignment in individuals with ankle or foot biomechanical issues that contribute to ITBS. Custom or over-the-counter orthotics can provide additional support, particularly for individuals with overpronation or structural imbalances.
By promoting better foot mechanics, orthotics may help reduce excessive strain on the knee, hip, and ITB. Improved alignment can support healthier movement patterns during walking, running, and other physical activities.
Surgery
Physicians typically recommend surgery for ITBS only when non-surgical treatments fail to provide lasting symptom improvement. Surgical options aim to reduce tension in the ITB and address chronic friction near the knee.
Procedures may include percutaneous release, open release, ITB Z-lengthening, or arthroscopic techniques. The choice of procedure depends on the severity of symptoms, the degree of tissue tightness, and the presence of structural abnormalities that affect the ITB.
Non-Surgical ITBS Relief With The Regenexx Approach
For individuals experiencing persistent ITBS symptoms, procedures using Regenexx lab processes offer non-surgical approaches that address both symptoms and contributing factors. These treatments focus on promoting better tissue health and supporting improved function.
The Regenexx evaluation process begins with a hands-on examination and a detailed review of lumbar spine MRI imaging. This comprehensive assessment helps identify whether low-level nerve irritation in the lower back may affect the ITB.
When nerve irritation is identified, a physician in the licensed Regenexx network may precisely inject advanced fourth-generation platelet lysate around the irritated nerve using fluoroscopic guidance. Additional information about this approach is available in the video below.
In addition to addressing nerve irritation, attention is directed toward the ITB and the vastus lateralis (VL) muscle. Physicians in the licensed Regenexx network use a high-dose platelet-rich plasma (PRP) formulation to help support tissue repair.
Unlike standard PRP preparations, Regenexx-SCP injectate provides a more concentrated and customized solution. Further details about this advanced approach are available in the video below.
Persistent ITB symptoms often involve hidden lumbar nerve irritation, even when obvious back discomfort is not present. A repeated need for foam rolling or stretching may suggest an underlying issue that affects nerve and muscle function.
Physicians in the licensed Regenexx network focus on identifying and addressing the true sources of iliotibial band problems. Early evaluation and intervention may help reduce long-term strain and support improved stability and mobility.
Take The Next Step To Getting Leg Pain Relief
Persistent outer thigh pain, tightness, or discomfort can limit mobility and affect overall quality of life. When symptoms continue despite rest, stretching, or strengthening, it may indicate an underlying issue that requires more targeted care.
At locations within the licensed Regenexx network, advanced diagnostic techniques and image-guided procedures are designed to address the symptoms and contributing factors behind ITB irritation. Procedures using Regenexx injectates may help promote healthier, stronger movement patterns by addressing affected nerves, muscles, and soft tissues.
Early evaluation and customized non-surgical interventions may help reduce strain on the ITB and support improved long-term function. Contact a physician in the licensed Regenexx network to learn more about comprehensive options for managing ITBS and supporting healthier mobility.
Get started to see if you are a Regenexx candidate
To talk one-on-one with one of our team members about how the Regenexx approach may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.

Medically Reviewed By:
