Osteitis Pubis: Pelvic Pain In Active Individuals

Medically Reviewed By:
Pelvic discomfort can interfere with even the most active lifestyles, potentially impacting mobility and daily routines. This type of pain often develops gradually, potentially impacting mobility and daily routines in ways that are hard to ignore.
One possible contributor to persistent pelvic pain in physically active individuals is osteitis pubis—a condition that may affect athletic performance and overall function. Gaining a clearer understanding of its potential causes, symptoms, and management strategies may help individuals take informed steps toward improving mobility and quality of life.
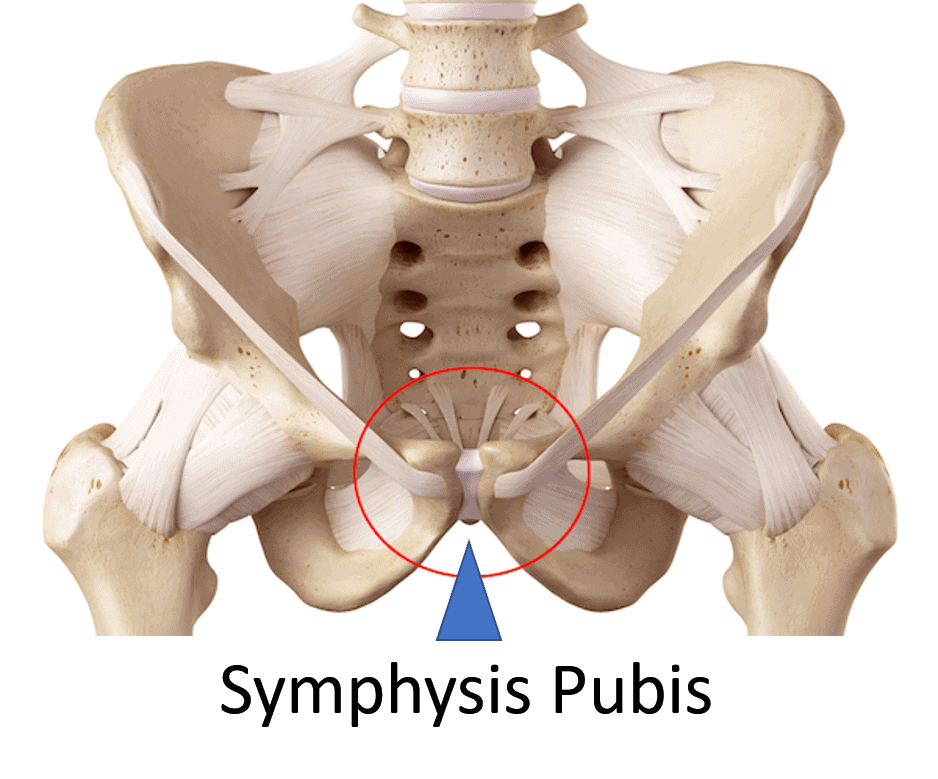
Defining The Anatomical Structure Of The Pelvic Ring
To better understand osteitis pubis, it’s helpful to first explore the anatomy of the pelvic ring and the symphysis pubis. The pelvis is a ring-shaped bony structure that plays a key role in supporting movement and stability in the lower body.
At the back, it connects through two sacroiliac (SI) joints, while at the front, it meets at the symphysis pubis. This interconnected arrangement of bones, joints, and soft tissues helps support body weight, contributes to movement, and provides protection for internal organs.
Taking a closer look at the pelvic ring and the symphysis pubis can offer helpful context for understanding osteitis pubis. The pelvic ring includes two sacroiliac joints at the rear and the symphysis pubis at the front, forming a closed structure that may influence lower body function and stability.

The pelvic ring functions as a single, interconnected structure, which means that changes or stress affecting one area, such as the sacroiliac (SI) joint at the back, may also influence the symphysis pubis joint at the front.
This dynamic relationship highlights the importance of understanding how stress and movement may be distributed throughout the pelvis. Although these challenges are commonly observed in athletes due to repetitive high-impact activity and mechanical strain, similar issues may also occur—though less frequently—in individuals who have undergone bladder or pelvic surgeries.
Surgical procedures in this region may influence soft tissue tension and pelvic stability, which may lead to compensatory stress on the symphysis pubis.
The symphysis pubis is a joint located at the front of the pelvis and is structured primarily for stability rather than mobility. Unlike highly mobile joints such as the knee or shoulder, it includes a fibrocartilaginous disc between the left and right pubic bones. This design may help the joint absorb stress and adapt to certain physical demands while supporting the overall stability of the pelvic region.
Defining Osteitis Pubis
Osteitis pubis is a condition that may occur when the symphysis pubis joint is subjected to excessive stress or instability, either directly, or as a potential consequence of dysfunction in the SI joints. For example, dysfunction in the SI joints may contribute to broader pelvic girdle instability, which can in turn place increased stress on the pubic symphysis. This ongoing mechanical strain may result in inflammation and discomfort in the joint, potentially contributing to further pelvic instability.
Because it occurs more frequently in athletes and physically active individuals, this condition is sometimes referred to by alternative terms such as sports osteitis pubis. These terms highlight the possible link between repetitive physical activities—particularly running, jumping, or sudden changes in direction—and the development of osteitis pubis.
Key Causes Of Osteitis Pubis
Osteitis pubis may result from various factors that place stress on the pelvic ring, particularly the symphysis pubis joint. While the condition is most commonly associated with athletes, other circumstances may also contribute to its development. Understanding these contributing factors may provide insight into the mechanisms that underlie this painful condition.
- Athletic Strain: High-impact activities such as soccer, running, or other sports involving repetitive motions may place cumulative stress on the symphysis pubis.
- Pelvic Instability: Muscle imbalances or core weakness may contribute to pelvic ring instability, potentially increasing strain on surrounding joints and ligaments.
- Post-Surgical Factors: Abdominal or pelvic surgeries may influence soft tissue tension or joint stability in the pelvic ring, which in some cases may lead to irritation of the symphysis pubis.
- Childbirth: The pelvic ring undergoes natural stretching during vaginal childbirth, which may place stress on the symphysis pubis and SI joints in some individuals.
Risk Factors
Certain factors may increase the likelihood of developing osteitis pubis by placing additional stress on the pelvic ring and the symphysis pubis joint. These contributors can be both mechanical and systemic:
- Physical Activity: High-impact activities such as running, soccer, or hockey involve repetitive movements that may place increased mechanical stress on the pelvis.
- Biomechanical Issues: Poor posture, muscle imbalances, or improper movement patterns may contribute to pelvic misalignment and joint strain.
- Medical Conditions: Pre-existing conditions such as arthritis, pelvic instability, connective tissue disorders, or a history of pelvic surgeries may compromise joint stability and potentially increase the risk of osteitis pubis.
- Pregnancy-Related Factors: Pelvic girdle discomfort during pregnancy—particularly due to hormonal and biomechanical changes—may increase strain on the symphysis pubis, especially following vaginal delivery.[1]
- Higher Body Mass Index (BMI): Elevated body mass has been associated with a higher prevalence of pelvic girdle pain, which could contribute to the development of osteitis pubis.
- Physically Demanding Work: Occupations involving repetitive lifting, prolonged standing, or other physical strain may place increased load on the pelvic joints.
- Emotional Distress: Psychological stress has been identified as a potential contributor to the development and persistence of pelvic pain in some individuals.
- Smoking: Tobacco use has been linked to impaired tissue recovery and may be associated with an increased risk of musculoskeletal pain, including pelvic-related discomfort.
Early Warning Signs And Symptoms
A common symptom associated with osteitis pubis may include pain in the symphysis pubis, located at the front of the pelvis. This discomfort may radiate to the groin, lower abdomen, or inner thighs, which may be related to the involvement of nearby muscle attachments such as the adductors or rectus abdominis.
The pain may be localized to one side or felt centrally within the pelvis, and often becomes more noticeable during physical activity. Movements that may aggravate symptoms can include kicking, pivoting on one leg, running, climbing stairs, hiking, lying on one side, intercourse, or coughing.
Being aware of the following symptom patterns may support earlier evaluation and appropriate management:
- Pain in the Symphysis Pubis: Discomfort felt at the front of the pelvis.
- Radiating Pain: Sensations that may extend to the groin, lower abdomen, or inner thighs.
- Localized Pain: Discomfort that may present on one side or be centered within the pelvis.
- Back Pain When Getting Up From A Chair: Pain when rising from a seated position may be due to muscle stiffness, joint degeneration, or spinal issues. It can cause discomfort in the lower back, often easing with movement but recurring with prolonged sitting. Read More About Back Pain When Getting Up From A Chair.
When To Seek Medical Attention
While some cases of pelvic discomfort may improve with rest and self-care, certain symptoms may warrant professional evaluation. You may consider seeking medical attention if you experience any of the following:
- Severe Or Persistent Pain: Intense discomfort in the pelvis or surrounding areas that does not improve with rest or over-the-counter options.
- Pain That Worsens With Activity: Symptoms that may consistently intensify during movements such as running, climbing stairs, or coughing.
- Difficulty Walking Or Standing: Pain or a sense of instability that may interfere with basic mobility or balance.
- Swelling Or Tenderness: Noticeable swelling, warmth, or tenderness in the symphysis pubis or nearby areas.
- Radiating Pain: Discomfort that may extend to the groin, lower abdomen, or inner thighs and does not improve with self-care.
- Post-Surgical Pain: New or worsening pelvic discomfort following abdominal or pelvic surgery that may limit daily activities.
- Postpartum Discomfort: Pain or instability in the pelvis after childbirth that may affect recovery or caregiving.
If these symptoms are present, consulting a medical professional may help determine the source of symptoms and guide appropriate treatment options. Early evaluation may also help reduce the risk of ongoing discomfort or further complications.
How Is Osteitis Pubis Diagnosed?
Evaluating osteitis pubis typically involves a combination of clinical assessment and imaging studies to better understand the source of pelvic pain and rule out other potential causes.
- Clinical Evaluation: During the physical examination, specific tests may be performed to assess pain levels and evaluate pelvic stability. Symptoms that may be associated with osteitis pubis include:
- Tenderness Over the Pubic Symphysis: Discomfort when pressure is applied to the front of the pelvis.
- Pain With Specific Movements: Discomfort that may worsen with activities like running, pivoting, or climbing stairs.
- Radiating Pain: Pain that may extend to the groin, lower abdomen, or inner thighs.
- Reduced Range of Motion: Limited hip or pelvic movement, which may be related to stiffness or pain.
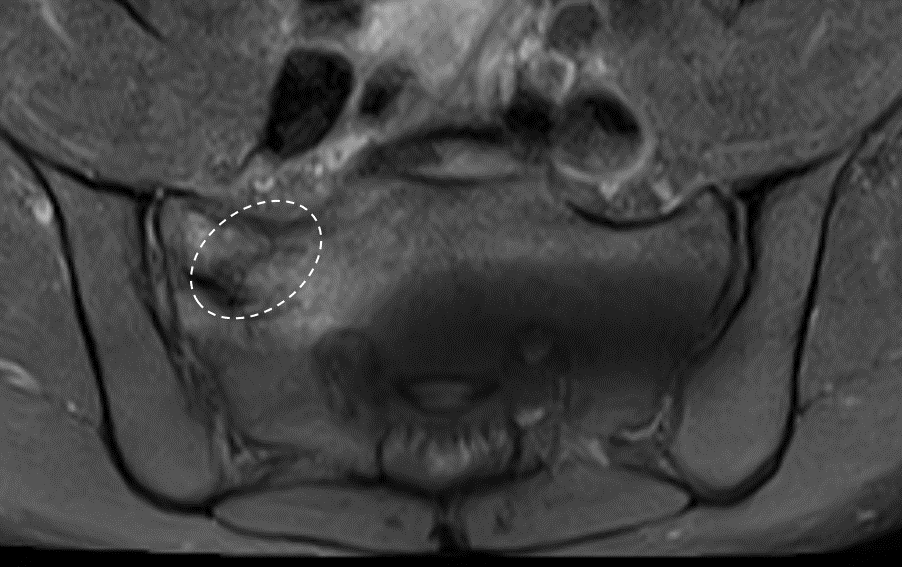
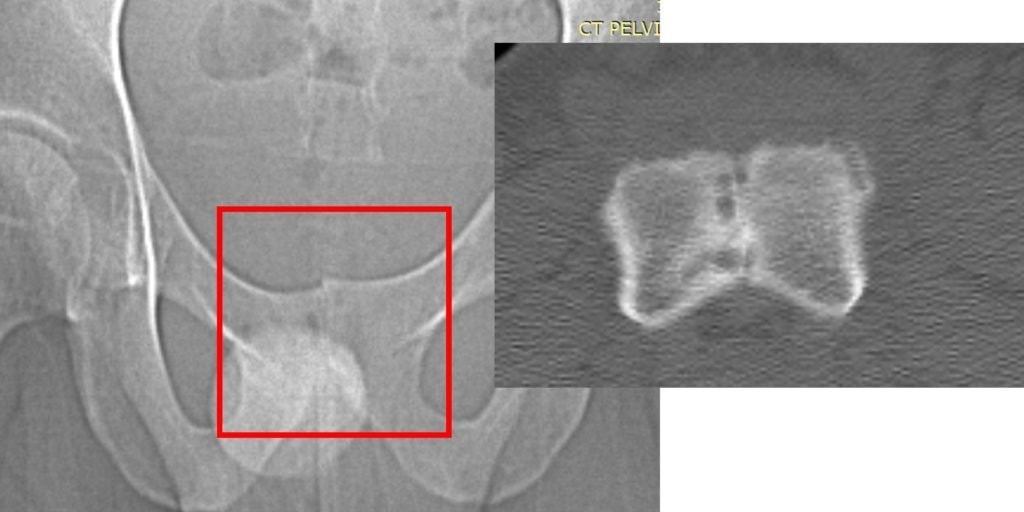
- Imaging Techniques: If osteitis pubis is suspected, imaging studies may be recommended to help assess inflammation or structural changes in the pelvis:
- X-rays: May reveal changes in bone structure, such as irregularities or reactive bone formation near the pubic symphysis.
- MRI (Magnetic Resonance Imaging): Often used to evaluate soft tissue inflammation, fluid buildup, or subtle bone changes that may not appear on X-rays.
- Ultrasound: In some cases, this may be used to examine soft tissue structures surrounding the pelvis.
Combining clinical findings with imaging results may help physicians determine whether osteitis pubis is present and guide treatment recommendations based on the individual’s condition and activity level.
Early evaluation and customized care may help improve outcomes and reduce the risk of ongoing discomfort or further complications.
Conventional Treatment Options
Managing osteitis pubis often begins with conservative, non-surgical approaches that may help reduce inflammation, relieve discomfort, and support pelvic stability. These methods aim to minimize strain on the symphysis pubis joint while promoting recovery.
- Rest And Activity Modification: Treatment may begin with rest and changes to physical activity to reduce stress on the pelvis. Athletes may need to temporarily avoid high-impact sports or movements that appear to aggravate symptoms.
- Heat Therapy: Applying heat to the affected area may help relax tight muscles and support local circulation, potentially offering temporary relief.
- Physical Therapy: Targeted exercises and manual therapy may help stabilize the pelvis and address biomechanical imbalances. Referral to a pelvic floor physical therapist may also be appropriate when deep core muscle dysfunction may be contributing to pelvic instability.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce pain and inflammation in conditions affecting joints, muscles, and the spine. While they provide temporary relief, prolonged use may increase heart, kidney, and gastrointestinal risks, requiring careful management. Read More About NSAIDs.
- Surgical intervention: Surgery may be recommended if other treatments are unsuccessful. This involves procedures like debridement, wedge resection, wide resection of the joint, or fusion (placing a screw or plate across the joint). It should be noted that all surgical options may alter the joint’s natural structure in some way.
Interventional Orthobiologic Options
Physicians in the licensed Regenexx network offer interventional orthobiologic procedures that may help manage osteitis pubis without surgery. These procedures are designed to support the body’s natural healing processes and improve joint stability.
The Regenexx approach to osteitis pubis includes platelet-rich plasma (PRP) injectates and bone marrow concentrate (BMC) injectates.
- Platelet-Rich Plasma (PRP) Injectates: PRP involves drawing a small sample of the patient’s blood, concentrating the platelets, and injecting them into the affected area to support tissue healing.
- Bone Marrow Concentrate (BMC) Injectates – BMC, which contains specialized cells and growth factors, is derived from a patient’s own bone marrow and may help support joint function and stability.
Physicians in the licensed Regenexx network use advanced imaging techniques, such as fluoroscopy, to precisely target affected areas, supporting the potential benefits of these procedures.
Case Study On Non-Surgical Management Of Osteitis Pubis
Over the years, advancements in non-surgical approaches have provided new options for managing osteitis pubis. Image-guided interventional orthobiologic procedures allow physicians in the licensed Regenexx network to target affected tissues, helping to address joint instability and promote function.
Case study:
A 30-year-old dentist and avid endurance athlete presented with mild osteitis pubis. He regularly participated in ultramarathons exceeding 100 miles, competing three to six times annually. About a year prior, he received a non-image-guided steroid injection into his symphysis pubis to manage the condition. Initially, he experienced symptom relief and resumed his rigorous training schedule.
Unfortunately, he later developed a sacral stress fracture. Imaging confirmed the fracture, and further investigation suggested it could be linked to steroid injections. Steroids may be associated with depleting progenitor cells, which are crucial in maintaining bone health and strength.
Treatment approach:
At that point, his treatment options included the use of orthobiologics to support the healing of the sacral fracture. Additionally, loose ligaments at the SI joint were likely contributing to joint instability, potentially placing excessive force on the sacrum and contributing to the fracture.
Orthobiologic injections could have been considered to help support the lax SI joint ligaments and restore stability. However, under the care of an orthopedic surgeon, the patient opted for an SI joint fusion instead.

The two large screws visible on the left pass through the SI joint into the sacrum. While this fusion stabilizes the joint, it also eliminates its natural movement. The SI joint is designed to absorb and distribute energy, and this functionality is lost after fusion. As a result, the energy that would typically dissipate through the SI joint is redirected elsewhere in the pelvic region.
When the patient resumed running just two months after the fusion surgery, the stress that the SI joint would typically absorb was instead redirected to the symphysis pubis. This excessive strain led to the rapid onset of severe osteitis pubis. Imaging studies (X-ray and CT scan) revealed significant damage: the normal space within the symphysis pubis, which houses the fibrous disc, had disappeared entirely, and the surrounding bone exhibited marked erosion.
At this stage, the patient faced the prospect of another surgery—this time to address the osteitis pubis resulting from the initial procedure. Instead, he sought treatment from Dr. Markle, a physician in the licensed Regenexx network, where orthobiologic procedures were utilized to address the worsening condition of his symphysis pubis joint.
Fluoroscopy-guided imaging demonstrated the precise delivery of the patient’s own bone marrow concentrate into the deteriorating bone surrounding the symphysis pubis and into the degenerated joint itself. This approach designed to support healing, may help reduce inflammation, and may help promote stability in the affected area.
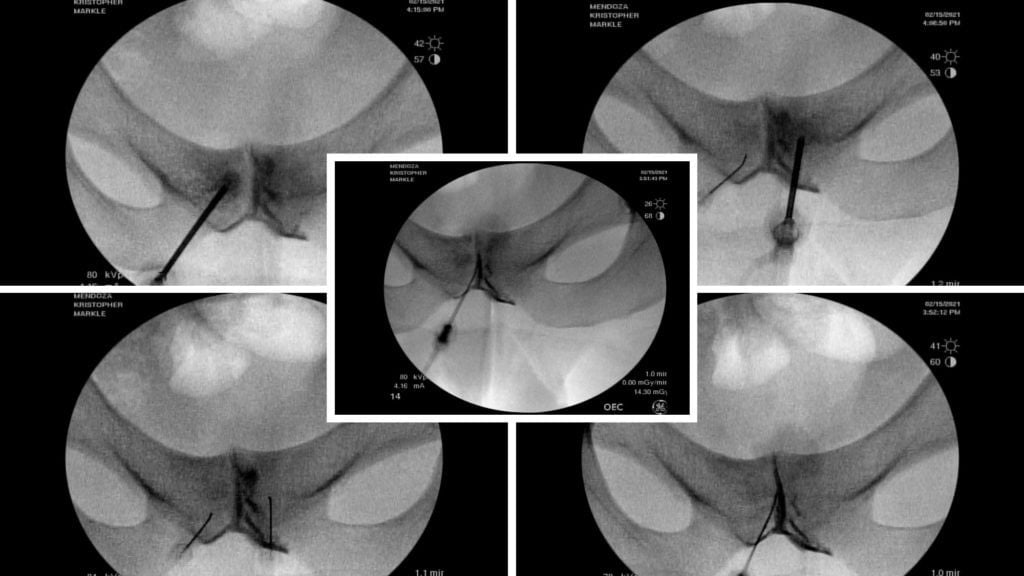
Outcome:
The images below, taken several months after the orthobiologic procedure, demonstrate significant improvement in the condition of the symphysis pubis joint.

The follow-up images indicate a restored joint space in the symphysis pubis, with improvements in the surrounding bone structure. The patient reported noticeable improvement, noting that 80–90% of his symptoms had diminished and that he experiences minimal daily discomfort. This outcome illustrates the potential role of orthobiologic procedures in supporting joint health and function.
Supporting Recovery Without Surgery After Osteitis Pubis
Osteitis pubis may interfere with daily activities and athletic performance, making proper management important for individuals seeking alternatives to surgery. While surgical intervention may be considered in severe cases, many people explore non-surgical approaches to help support joint function and relieve symptoms.
Interventional orthobiologic procedures, such as those using SCP or SD injectates, may help reduce inflammation, support tissue health, and contribute to improved pelvic stability in appropriate cases. Complementary strategies, including physical therapy, targeted strengthening exercises, and posture adjustments, may also help support long-term pelvic and spinal health.
For individuals experiencing persistent discomfort or mobility challenges, consult a physician in the licensed Regenexx network to explore treatment options.
References
- Walters C, West S, Nippita TA. Pelvic girdle pain in pregnancy. Aust J Gen Pract. 2018;47(7):457–461. doi:10.31128/AJGP-01-18-4467. https://www1.racgp.org.au/ajgp/2018/july/pelvic-girdle-pain-in-pregnancy

Medically Reviewed By:
