Straightening Of The Cervical Lordosis And What May Cause It

Medically Reviewed By:
The cervical spine normally curves forward in a shape called cervical lordosis. This curve helps distribute weight, absorb shock, and support smooth head and neck movement. When the curve straightens, it may place excess stress on spinal joints, muscles, and discs, which may lead to structural changes over time.
Identifying the factors contributing to this change can help guide appropriate evaluation and inform clinical strategies for maintaining spinal alignment and function.
Anatomy And Function Of The Cervical Spine
The cervical spine comprises seven vertebrae (C1 to C7) that support the head and allow for a wide range of motion. These vertebrae are separated by discs and stabilized by joints, ligaments, and muscles. On imaging, physicians may note a reduction in the neck’s natural curve, commonly referred to as cervical lordosis.
Physicians may describe this with terms such as:
- Straightening of the normal cervical lordosis
- Loss of cervical lordosis
- Straightening of the cervical curvature
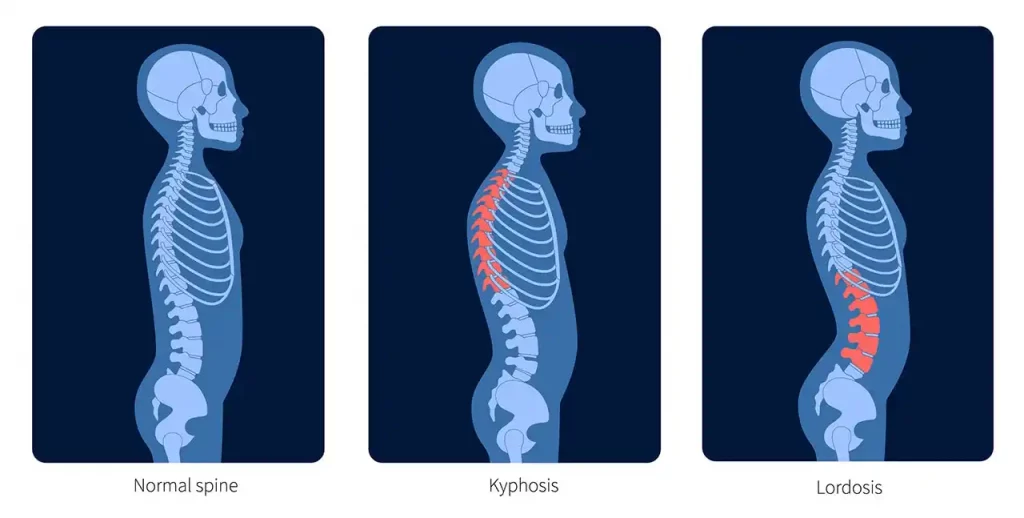
The spine’s alignment is shaped by alternating curves that help manage load and maintain balance. The cervical and lumbar regions curve forward in lordosis, while the thoracic spine curves backward in kyphosis. These complementary curves support upright posture and help distribute stress across spinal structures.
When one of these curves, such as the cervical lordosis, is reduced, it may shift how forces are absorbed through the spine. This change can lead to postural adaptations, increased soft tissue strain, or added joint stress in the neck. Over time, these compensations may affect mobility or contribute to physical discomfort.
Understanding Loss Of Cervical Lordosis (Natural Curve Of The Spine)
Loss of cervical lordosis refers to a reduction, straightening, or reversal of the neck’s natural forward curve. This change may alter how mechanical forces travel through the spine, adding stress on discs, joints, and surrounding soft tissues.
One recent study examined the relationship between cervical alignment and blood flow through the vertebral arteries. These vessels pass through the cervical vertebrae and help supply blood to the back of the brain.
Using Doppler ultrasound, researchers compared individuals with normal cervical curvature to those with a straightened cervical spine. Findings showed that those with reduced cervical lordosis had narrower artery diameters and lower blood flow.
These results suggest that changes in cervical alignment may impact musculoskeletal function and influence blood flow to brain regions served by these arteries. While more research is needed, the findings highlight the potential for broader physiologic effects when spinal alignment is disrupted.
Other Symptoms That May Affect The Natural Spinal Curve
Changes in the cervical curve may be associated with a range of symptoms, many of which overlap with other spinal conditions. These may include:
- Neck pain: Muscle fatigue, joint stress, or disc loading may contribute to persistent or activity-related discomfort in the neck.
- Headaches: Increased tension in the upper cervical spine may affect nerves that communicate with the scalp, potentially contributing to cervicogenic headaches.
- Reduced range of motion: A loss of normal curvature may limit neck flexibility, making it more challenging to look up, look down, or rotate the head.
- Disc degeneration: Uneven mechanical pressure on cervical discs may play a role in structural changes over time, including bulging or herniation.
- Decreased blood flow: Changes in vertebral alignment have been associated with reduced diameter of the vertebral arteries, which may influence circulation to posterior brain regions.
How Does Straightening Of The Cervical Lordosis Happen?
Straightening of the cervical curve can develop gradually in response to long-term mechanical stress or injury. Rather than maintaining its natural arc, the spine may shift alignment to adapt to abnormal forces. Several factors may contribute to this change over time. Common contributors include:
Trauma Or Whiplash Injuries
Trauma, including whiplash injuries, may introduce sudden force through the cervical spine. As a protective response, surrounding muscles may tighten, resulting in temporary changes to spinal alignment. In some cases, the natural curve may remain reduced if soft tissue injury or joint dysfunction persists over time.
Poor Posture Or Muscle Imbalances
Prolonged forward head posture, often linked to screen use, can shift the head’s weight and increase strain on the neck. Over time, tight muscles and weak stabilizers may alter spinal alignment. These imbalances may reduce the natural curve and restrict movement. If left uncorrected, long-term structural changes may gradually develop.
Cervical Spondylosis Or Degenerative Disc Disease
Age-related changes, such as disc dehydration and joint wear may lead to cervical spondylosis. As discs lose height, the spine may compensate by flattening its natural curve. These changes can also reduce shock absorption, limit mobility, and alter joint mechanics over time.
Ligament Injuries Or Laxity
Ligaments help stabilize the cervical spine and support its natural curve. When injured or lax, this support may be reduced, allowing the spine to shift out of alignment. Over time, this instability may contribute to a straighter curve, joint irritation, and muscle overcompensation.
Post-Surgical Changes
Spinal surgeries, particularly those involving fusion or hardware, may alter cervical alignment. Limited motion in one area can shift mechanical stress to surrounding segments. Over time, this may contribute to a gradual loss of the natural curve. Muscle tension or scarring after surgery may also affect posture and stability.
Underlying Medical Conditions
Some medical conditions may influence spinal alignment and contribute to a reduced cervical curve. These conditions can affect joint health, muscle tone, or connective tissue stability. In such cases, changes in posture or movement patterns may develop gradually.
- Annular Tears: An annular tear is a small rupture in the outer layer of a spinal disc, which may cause localized back pain or nerve irritation. Symptoms can vary, with some tears leading to radiating pain, numbness, or weakness if the disc presses on nearby nerves. Read More About Annular Tears.
- Dural Leak: A dural leak occurs when the protective membrane surrounding the brain and spinal cord (dura mater) is damaged, leading to cerebrospinal fluid (CSF) leakage. This may cause headaches, dizziness, nausea, and other neurological symptoms, often worsening when upright. Read More About Dural Leaks.
- Bulging Discs: A bulging disc occurs when a spinal disc extends beyond its normal space without rupturing. Depending on the affected area, it may cause localized pain or nerve compression, leading to numbness, tingling, or weakness in the back, neck, or limbs. Read More About Bulging Discs.
Key Tests To Diagnose Loss Of Cervical Lordosis
Accurate diagnosis begins with a thorough clinical evaluation and appropriate imaging. These tools help assess the degree of curvature change and identify possible contributing factors.
- Physical examination: A physician in the licensed Regenexx network may assess posture, range of motion, muscle tone, and signs of joint or nerve involvement.
- X-rays: Standard side-view cervical X-rays can reveal whether the natural curve is preserved, reduced, or reversed.
- MRI (magnetic resonance imaging): MRI offers detailed views of discs, ligaments, the spinal cord, and soft tissues useful for identifying degeneration or ligament injury.
- CT (computed tomography) scans: CT scans provide high-resolution images of bone structure and may help evaluate post-surgical alignment or bone damage.
- Motion imaging (dynamic X-rays): Flexion-extension X-rays can detect abnormal movement or instability between vertebrae that are not visible on static images.
Along with clinical findings, these diagnostic tools help guide treatment planning and determine whether the curve change is related to structure, soft tissue, or injury.
Conventional Treatments To Address Spinal Curve Changes
Treatment for cervical curve changes often begins with conservative, non-surgical approaches. These methods focus on improving alignment, restoring function, and reducing symptoms linked to altered biomechanics.
- Physical therapy: Targeted exercises and mobility work aim to strengthen the neck’s stabilizing muscles, improve posture, and correct muscle imbalances that may contribute to alignment changes.
- NSAIDs: Nonsteroidal anti-inflammatory drugs may help reduce inflammation and manage pain related to joints, muscles, or soft tissues, improving function during daily activities.
- Chiropractic care: Manual adjustments, traction, or mobilizations may promote spinal motion and help reduce stress on supporting structures.
- Postural correction devices: Temporary use of braces or supports may cue proper neck positioning during standing, sitting, or movement.
- Surgical intervention: Surgery may be considered in more complex cases, such as those involving structural instability, neurologic symptoms, or where conservative care has not produced sufficient improvement.
- Spinal fusion: This procedure permanently connects vertebrae to stabilize motion segments, often used when significant damage or instability is present.
- Laminectomy: Removes part of the vertebra to relieve pressure on the spinal cord or nerve roots, commonly performed in cases of spinal canal narrowing.
- Discectomy: Involves removing damaged disc material that may be compressing nearby nerves or contributing to abnormal spinal curvature.
- Cervical artificial disc replacement (ADR): Replaces a degenerated disc with a mobile implant designed to preserve motion and support more natural alignment.
- Osteotomy: A surgical technique used to realign spinal segments by cutting and repositioning bone. Typically reserved for severe spinal deformities.
- Spinal fusion: This procedure permanently connects vertebrae to stabilize motion segments, often used when significant damage or instability is present.
The Regenexx Approach: Advanced Non-Surgical Options for Supporting Spinal Curvature
For individuals with cervical curve loss related to ligament injury or joint instability, procedures using Regenexx lab processes may offer a non-surgical approach to support spinal alignment and function.
These image-guided treatments use precise injections of a patient’s own biologics, such as platelet-rich plasma (PRP) or bone marrow concentrate to target affected ligaments and supporting tissues. Image guidance allows for accurate placement into areas contributing to instability or altered alignment.
By supporting the body’s natural healing response, these procedures may help reduce symptoms and promote improved stability. The Regenexx approach addresses the biomechanical sources of dysfunction rather than focusing only on symptom relief.
Tips To Avoid Losing The Normal Spinal Curve
Maintaining the cervical spine’s natural curve requires consistent attention to posture, movement, and ergonomics. Daily adjustments may help support long-term alignment and reduce strain on soft tissues.
- Maintain good posture: Keep your head centered over your shoulders with a neutral spine and relaxed shoulders to reduce stress on neck muscles and joints.
- Set up an ergonomic workstation: Position your monitor at eye level and adjust your chair and keyboard to minimize forward head posture during computer use.
- Sleep in spine-supportive positions: Use a cervical-supportive pillow and sleep on your back or side to help maintain alignment while resting.
- Stay active with low-impact movement: Walking, swimming, or cycling may help improve circulation and support joint and muscle health.
- Strengthen core and back muscles: A stable core may reduce excess strain on the neck by promoting more balanced posture and movement control.
- Take breaks from prolonged sitting: Stand, stretch, or walk every 30 to 60 minutes to relieve pressure on spinal discs and reduce muscle fatigue.
- Hold devices at eye level: Bring phones, tablets, or laptops up to eye height to avoid repeated downward bending of the neck.
- Use proper lifting mechanics: Bend through the hips and knees, keep objects close to the body, and avoid twisting to help protect spinal alignment.
Optimize Cervical Spine Health For Improved Function
The cervical curve plays a key role in supporting the head, balancing spinal forces, and protecting joints, discs, and soft tissues. When this curve flattens, strain on these structures may increase.
Recognizing early changes, such as altered posture or injury, and addressing contributing factors can help maintain long-term spinal health. Conservative care and image-guided biologic procedures may support better alignment and reduce symptoms.
The Regenexx approach offers non-surgical options designed to help support spinal stability and promote functional improvement. Supporting cervical alignment is essential for daily movement, neurologic function, and structural integrity.
Get started to see if you are a Regenexx candidate
To talk one-on-one with one of our team members about how the Regenexx approach may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.

Medically Reviewed By:
