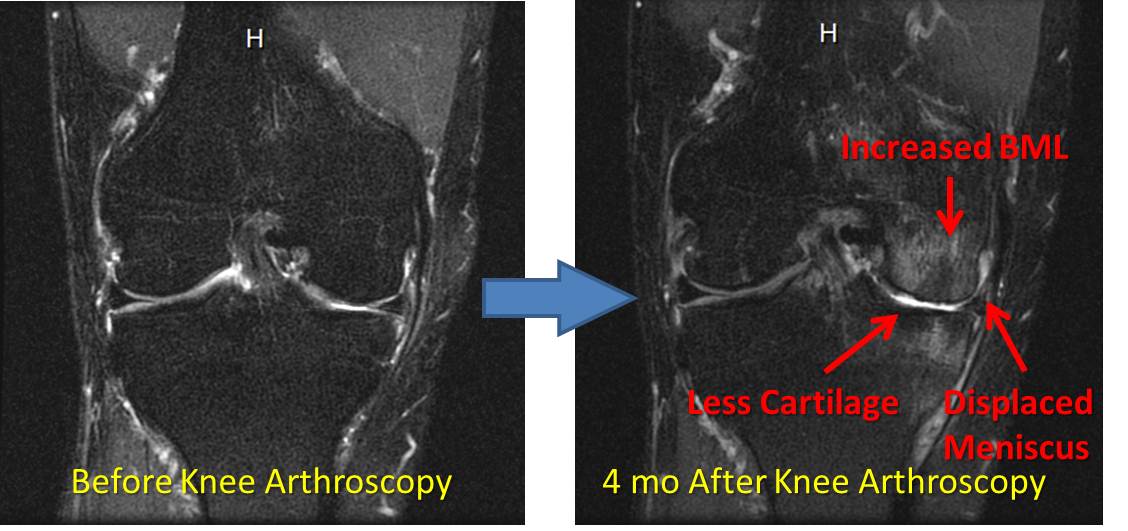
Knee Surgery Complications: Watch a Knee Go from Slightly Abnormal to a Mess in 4 Months!
Knee surgery complications are profound and consequently we’re not fans of knee surgery or really any type of arthroscopic debridement. This surgery means that the doctor removes cartilage and meniscus tissue that is torn or frayed through a knee scope. First, there is no research showing knee arthroscopy for arthritis works and in fact there’s copious research showing it doesn’t work. Second, removing tissue has it’s consequences. As an example, check out this graph of the increased stress on the knee joint caused by removing parts of the meniscus. A concrete example of this phenomenon is the knee MRI above. This picture is from a patient asking about stem cell therapy after a surgery made his knee worse. The MRI on the left is before surgery and just shows an area in the inside compartment where the cartilage is thinned. However, the lack of swelling in the bone tells me this is a functional knee, meaning that the meniscus and cartilage are working to protect the bone. The picture on the right is after an arthroscopic knee surgery to “clean up” the knee. It’s now a mess! There’s more cartilage loss, the small remaining meniscus after surgery has begun to slip outside the joint and has new tears, and the bone is now swollen (shown above as “Increased BML”), indicating that the new “cleaned up” configuration of the knee is no longer protecting the bone. It’s therefore no surprise that the knee that began in pain prior to the surgery is now in more pain. This past week I saw the same thing happen to an ankle that was surgically “cleaned up”. The patient was able to run and had mild arthritis before the surgery and is now not able to run with dramatically more arthritis and severe lost range of motion due to surgical scarring. So why are we still performing these surgeries? Good question. Is debridement surgery ever appropriate for a joint? Sure. There are times when a knee or other joint is locking due to a torn piece of meniscus or cartilage where surgery is needed or when a large non-function bone spur is preventing functional movement. However, in our experience, these only encompass only about 1 in 3 knee surgeries these days. The upshot? Getting your knee surgically “cleaned up” has no research to support that it will help you and we have lots of clinical experience that shows up that it may make you much worse.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.