My 2024 PRP RCT Infographic 2.0
I blog about what comes my way as a practicing physician using orthobiologics and the medical director of Regenexx. In many ways, LinkedIn becomes my professional sounding board with other physician colleagues. This past week, I posted my 2024 PRP RCT infographic, which was very well received. However, one colleague pointed out that I should have spent more time parsing non-inferior studies from those showing superiority for PRP. If you’re wondering what that means, don’t worry; you’re not alone. Let’s dive into that concept and an edited 2024 PRP infographic.
Why Is PRP a Game Changer?
Physicians who inject things precisely using imaging guidance into painful or damaged parts of the musculoskeletal system have inherited some severely flawed tools. One of those is corticosteroids. These medications were introduced in the 1940s after America helped win WWII. Hence, they are far older than any practicing physician using them today. In many cases, they are far older than the parents of physicians using them today.
Your body uses corticosteroids daily, but it uses nanograms of these substances. The problem is usually not the corticosteroid but the absurd milligram dose physicians use. How big a dose is a milligram of steroid? If the height of a matchbook is a nanogram, then the height of the Empire State Building is a milligram.
I first realized how crazy this dose was when we cultured mesenchymal stem cells in about 2006. I asked our lab staff to place a single drop of the corticosteroid we used in one of those cultures, which promptly killed all stem cells. What happens when you use a nanogram dose (which doctors don’t have ready access to)? You can push these cells to differentiate into one tissue over another, and they will stay quite healthy.
We have a mountain of evidence that these mega doses of corticosteroid used by doctors every day kill cartilage, destroy tendon cells, kill off bone osteoblasts, and wreak havoc with the immune and endocrine systems. As currently formulated, this is a bad drug class that probably needs expanded informed consent before it’s injected.
It’s in this context that we should be discussing the non-inferiority or superiority of PRP. For example, this means that if PRP is non-inferior to corticosteroids and we know that steroids are bad drugs hurting our patients, PRP clearly wins.
What the Heck Does Non-inferior Mean?
Every profession has words and phrases it creates that are overly complex, and non-inferior is one of those terms. This basically means that when you test one drug or treatment versus another, one drug/treatment works about as well as the other or is “non-inferior.” The drug or treatment we compare against another is called a “comparator”. Superior means that the tested drug/treatment is better than the comparator. Inferior goes the other direction. Hence, in our context this morning:
- Superior-PRP is better than the comparator.
- Non-inferior-PRP is about the same as the comparator
- Inferior-PRP performed worse than the comparator
Reworking the 2024 Infographic
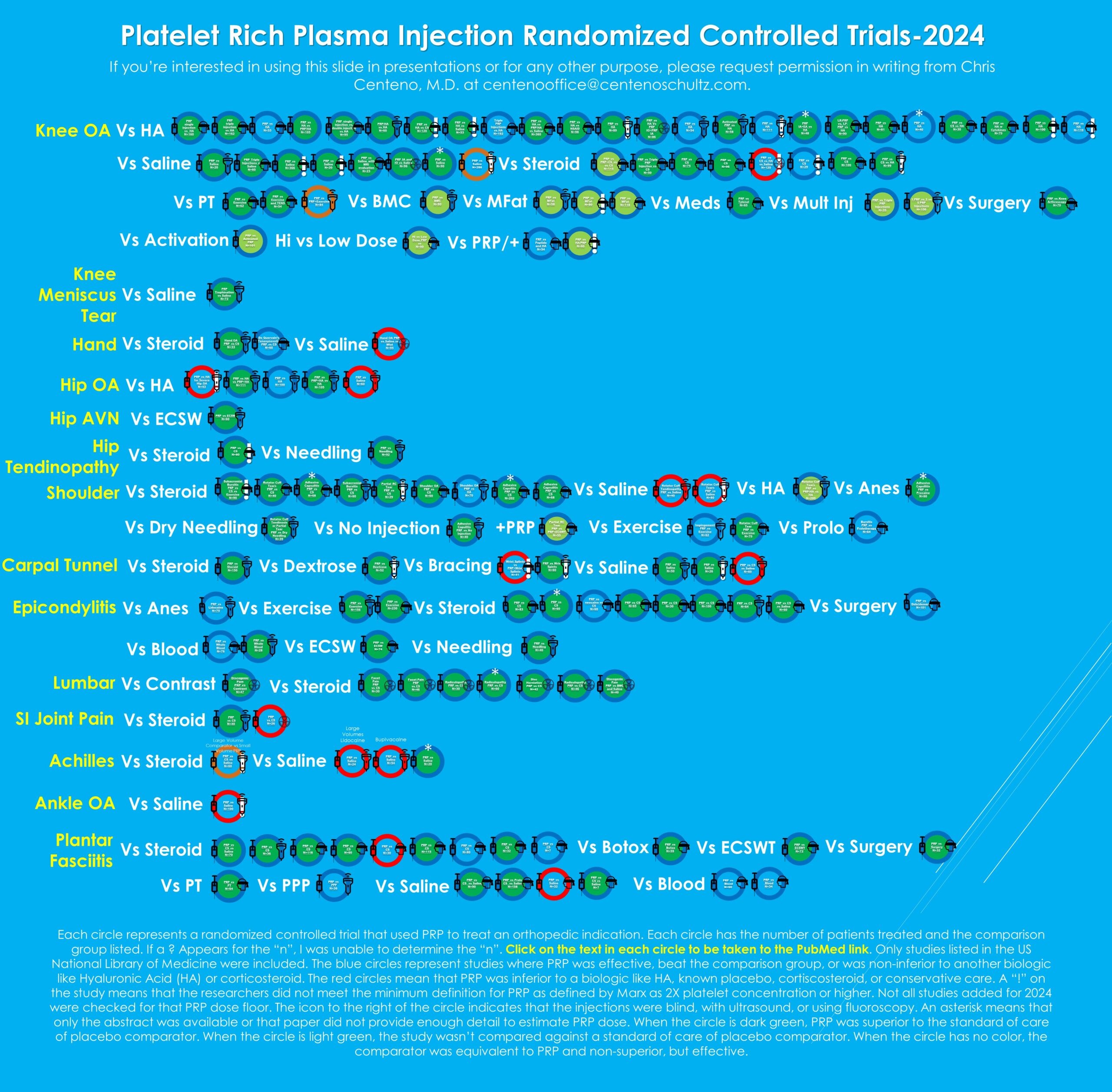
I spent the better part of a week going through the 144 entries in the 2024 PRP infographic one by one. As with any massive undertaking, I found a few errors and bad links that needed to be fixed. Often, these were double links with the correct one present and one copy/pasted from the old icon. All of that was fixed. The new 2.0 PRP infographic is below (the new one is also on the original post from July,9th). Please click the image below to be taken to the PDF with the active links.
I also coded every study with:
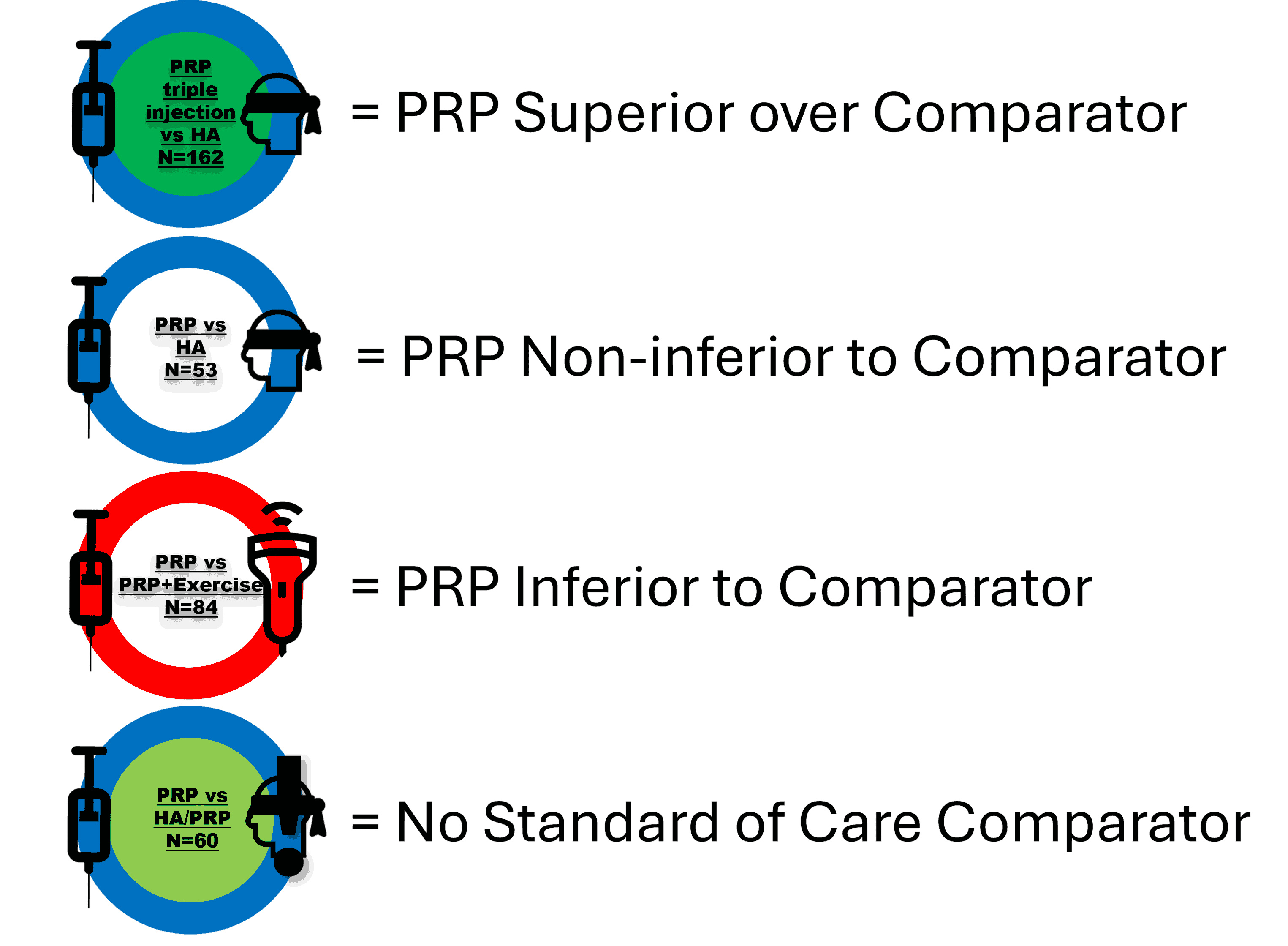
No standard of care comparator means that the study wasn’t about seeing if PRP worked better than [steroid, HA, saline, etc…], but instead something like does 1 PRP injection work better than three injections?
So what does this reworked data look like?
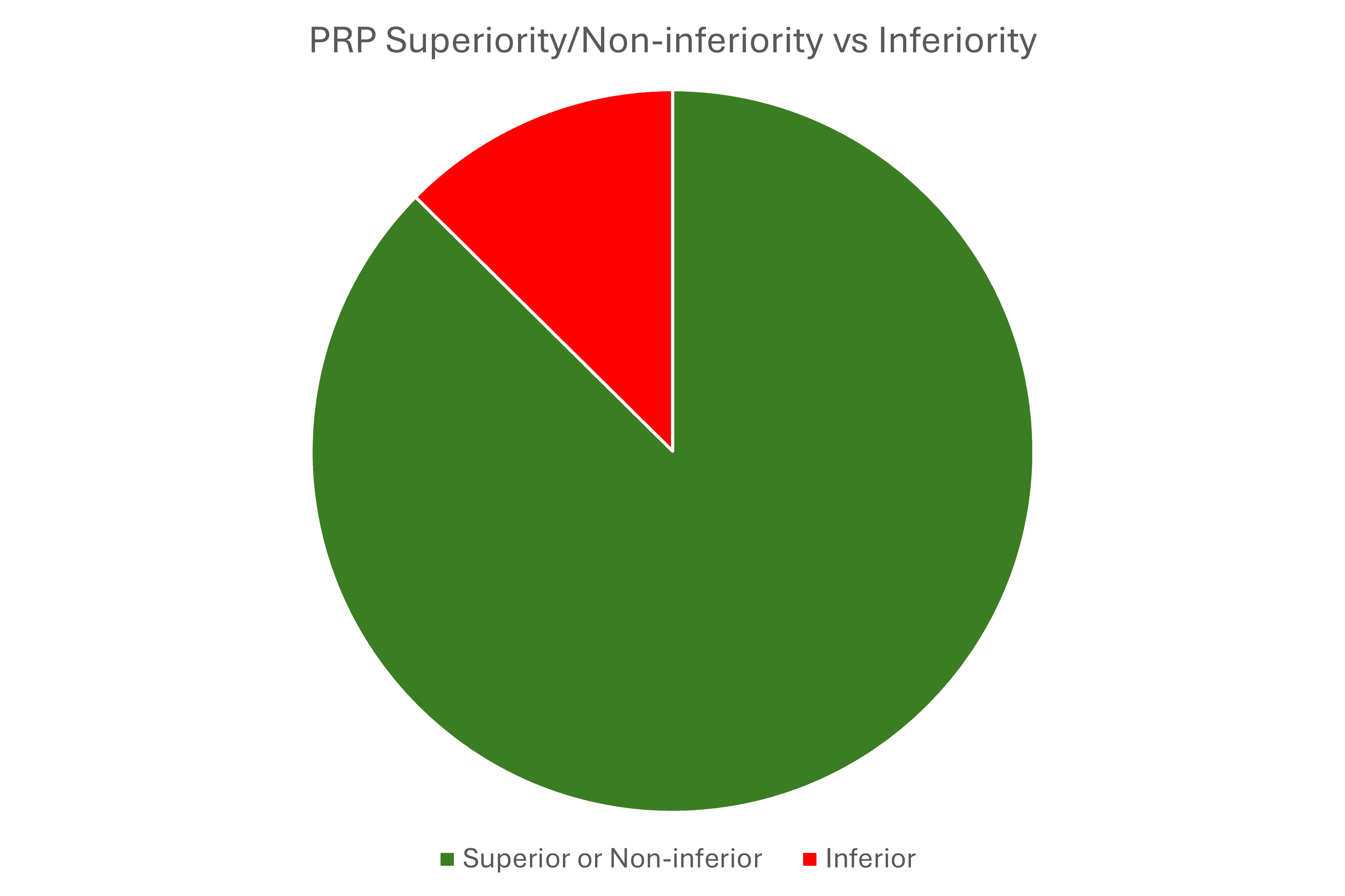
87% of PRP studies against standard-of-care comparators like steroids, HA, PT, needling, etc… were positive trials. That means they either showed that PRP was superior or non-inferior to the commonly used treatment comparator. For non-inferior, saline was excluded as that was a placebo. So, if PRP was the same as placebo, then the study was coded as a failure.
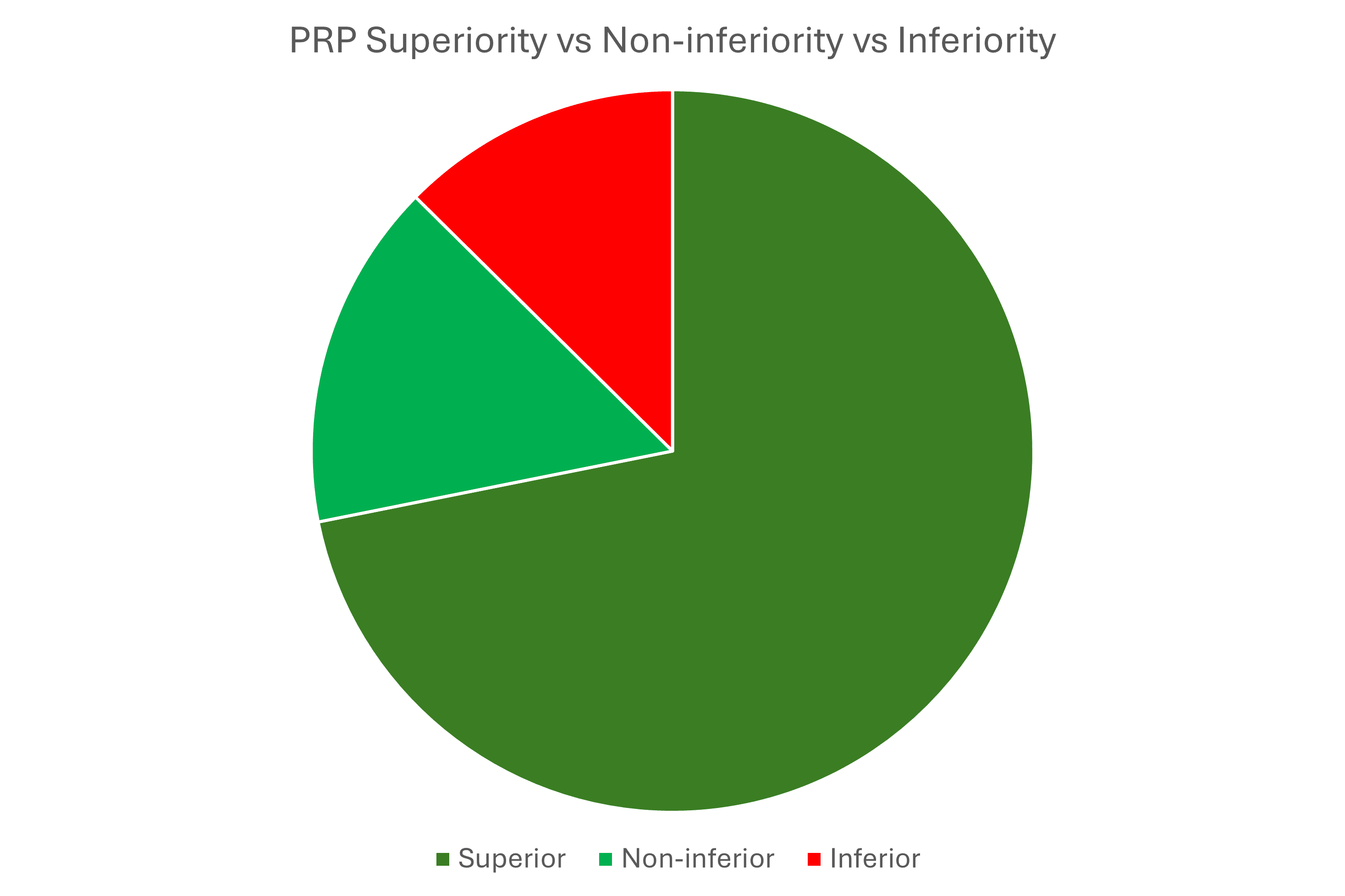
Above is superior vs. non-inferior vs. inferior, broken out into categories.
The upshot? It was great to go back through the original infographic study by study and tease all of this out. In addition, that gave me a chance to fix a few links and other things. Ultimately, my original recommendation that you now have my permission to roll on the floor laughing when someone says we don’t have enough research that PRP is effective still stands!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.