Her Neck Goes Out All the Time: Definitive Treatment?
Every physician has patients who challenge his or her skills, and it’s the reaction to those patients that determines what kind of doctor that physician is —Chris was one of those patients. She would tell me consistently that “my neck goes out all the time,” but every tool I had to use couldn’t seem to really put a dent in that phenomenon. In fact, it wasn’t until I invented a new procedure to get access to obscure neck ligaments that hold the head on that things changed.
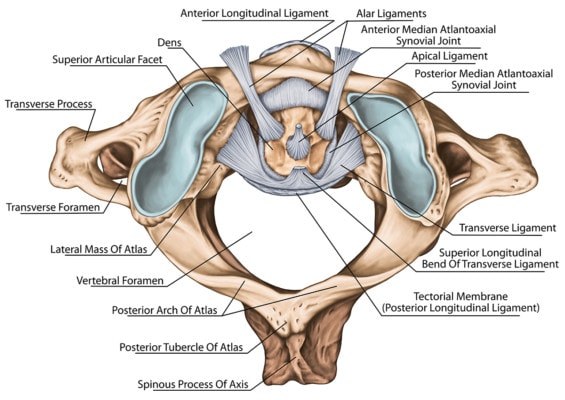
Ligaments found in the neck. Stihii/Shutterstock
What Does “My Neck Goes Out” Even Mean?
Like many MDs, for most of my career, the concept of BOOP (bone out of place) has been a bizarre and even threatening one. However, all of that changed when it began happening to me. So why does a patient saying “my neck goes out all the time” sound crazy to an MD?
We MD physicians can be arrogant bastards when we don’t know what we don’t know. Meaning that for any professional, there’s the world of what you know and the world of what you know you don’t know. However, what blindsides you is if the stuff you can’t fathom exists. BOOP is in that place for an MD.
The idea of a neck or back “going out of place” seems foreign to us because in our world, we were taught that instability is a binary concept (a joint in the body is either stable or unstable). If it’s stable, it’s fine; if it’s unstable, it will fall apart on its own or that instability is easy to see on X-rays or on an exam where you try to move the joint.
An example of this binary thinking about instability is an anterior cruciate ligament (ACL) in the knee. Surgeons often consider an ACL to be “intact” or “ruptured,” a binary concept like “on” or “off.” However, the ACL, like any ligament, is made up of hundreds of thousands of individual fiber bundles, and it, of course, can be “loose” when some of those fibers are injured and some are left intact. However, this frankly flies over the heads of most surgeons, who were never taught to think that way. As a result, BOOP sounds like alternative-medicine mumbo jumbo to them. If a spine bone were “out of place,” it should be dislocated, and that would be easily seen on an X-ray as some catastrophic misalignment. However, in this case the surgeons don’t know what they don’t know.
Prima Facie Evidence That the Neck and the Back “Go Out”
These past few years, I began to understand what patients tell me when they say, “My neck goes out all the time.” First, I began to experience “crepitus” in my neck and back, or what feels like the spine bones are “moving.” These abnormal movements can certainly lead to episodes that cause severe pain. So what’s happening as interpreted by a physician who knows the spine research? The term is called, “degenerative instability.”
My neck and back ligaments are getting loose as the discs degenerate with age as well as a lifetime of wear and tear. In addition, the small muscles built to stabilize the spine are intermittently getting turned off, leading to even sloppier movement. Hence the individual spine bones (vertebrae), stacked one on the other, can get into awkward positions where a spinal nerve gets pinched or a facet joint or disc gets suddenly damaged. This is what my patients have been relaying through the years when they tell me things like, “My neck goes out all the time.”
Chris’s Neck-Instability Story
Chris has been a patient of mine for more than a decade. In that time, she has told me many times that her “neck goes out all the time.” Early on in her care, when I didn’t know personally what that meant, I at least knew that what she was describing was some type of instability. Over those years, we tried countless physical therapy visits for strengthening and manual medicine. She also tried chiropractic, massage, acupuncture, trigger-point dry needling, trigger-point injections, etc. I also injected her neck many times with prolotherapy-type treatments meant to tighten loose ligaments as well as injections around nerves (epidurals) and into painful joints (facet injections). While some of this helped, nothing really changed her instability.
“The back of mouth injections have helped a lot, much more than anything else, including other injections you’ve done.
So what Chris describes is that after a honeymoon period and then after an adaption period where her muscles had to relearn how to deal with a more stable upper neck, this procedure has been a game changer for her.
The upshot? Happy Mothers Day to Chris! The idea that your neck or back can go out is a real thing due to instability and loose ligaments. While oftentimes this can be taken care of by chiropractic or other types of manipulation or simple shots to tighten ligaments (prolotherapy), that only works when the area is stable enough to hold or you can reach those ligaments. When the ligaments are like the ones that hold the head on, then new procedures must be invented to get access to them. In Chris’s case, finally reaching those ligaments after more than a decade of other treatments has made a big difference!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.