Neck Headache Causes: Your Neck Muscles Are Jacked into Your Brain?
First, the cine MRI of a CCJ (upper neck) injury patient, above, is just plain cool. It shows how the neck structures move in a way that has never been seen before. It also shows a few significant issues, but today we’ll focus on neck headache causes, specifically the myodural bridge. What’s that? The connection between your neck muscles and your brain!
What Is the Myodural Bridge?
As I’ve said before, we MDs can be arrogant idiots. I remember when I began my career that the neurologists I met actually disputed that the neck had any role in headaches. This was despite a century of experience of physical therapists, chiropractors, and alternative health practitioners successfully relieving headaches by treating the neck. So there were no recognized neck headache causes.
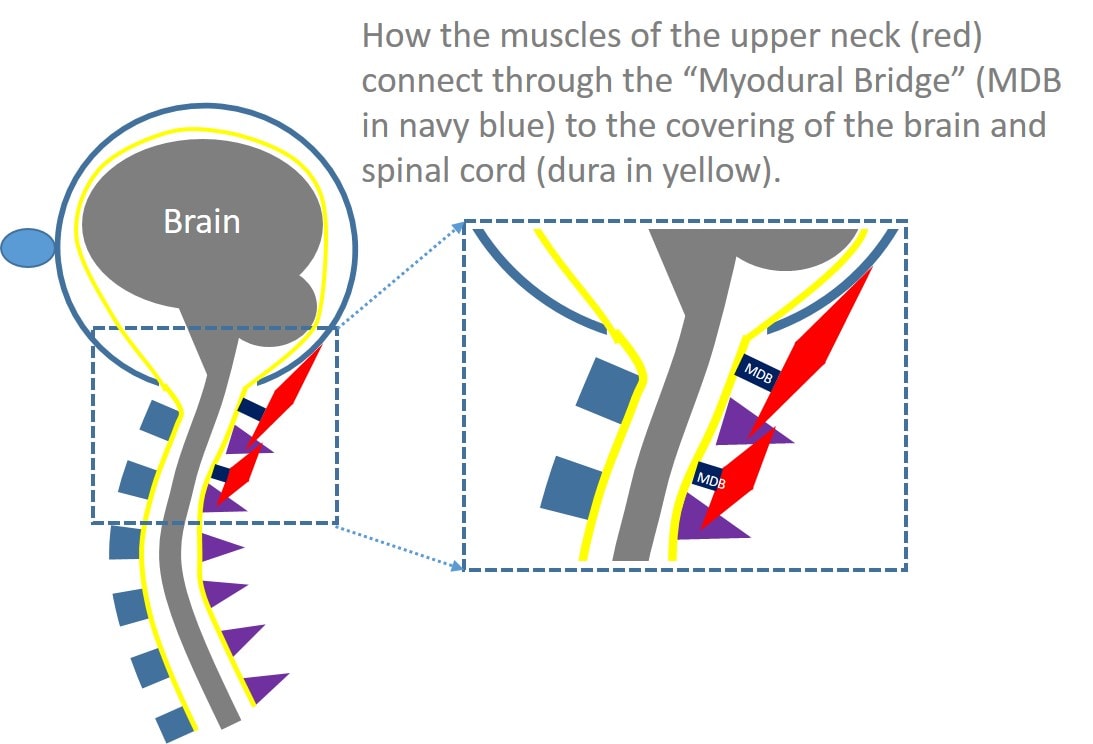
In the ’90s, researchers began to uncover neck headache causes. First they noted that the upper neck joints could refer pain to the head. Then they noted that certain nerves in the neck could also cause headaches. By the early 2000s, a few neurosurgeons began to notice that when they needed to cut through the upper neck muscles, some patients’ headaches would vanish. They then began studying cadaver dissections more closely, and they discovered what everyone else had missed: the upper neck muscles actually connected into the covering of the brain, called the dura. They called this newest neck headache connection the myodural bridge (myo=muscle and dural=covering of the brain).
One of the interesting things about this muscle-brain connection is that we now have several studies that show that muscle atrophy in this area is a bigger deal than tight muscles. Atrophy means that a muscle gets smaller and weaker. One of our ex-physical therapists, Jim Elliott (now a professor at Northwestern), has done some excellent research showing that upper neck muscle atrophy is associated with traumatic neck injury and more pain. Interestingly, that same type of research factors into the myodural bridge as well, with one group looking at traumatic-head-injured patients with headaches and finding that the only muscle atrophied that was associated with pain was the rectus capitis posterior minor. Why is this important? This is the specific muscle that jacks into the brain through the myodural bridge!
Can We “See” Myodural Bridge Problems on MRI?
Way up in Upstate NY there’s a hidden gem of an imaging center. Scott Rosa is an upper cervical chiropractor whom I’ve known for many years. Scott has a passion for upright MRI and an on-site machine where he does groundbreaking work on getting pictures of what’s going wrong with CCJ patients. I’ve gotten to know Scott because of our mutual interest in CCJ patients (upper neck injuries) and some of the cutting-edge procedural work we’ve done in the upper neck. This last week, we shared a mutual patient as we’ve done many times in the past, and Scott sent the cine MRI you see above for me to take a look. There are many interesting things on this MRI, but it has one finding that plays into our discussion this morning of the myodural bridge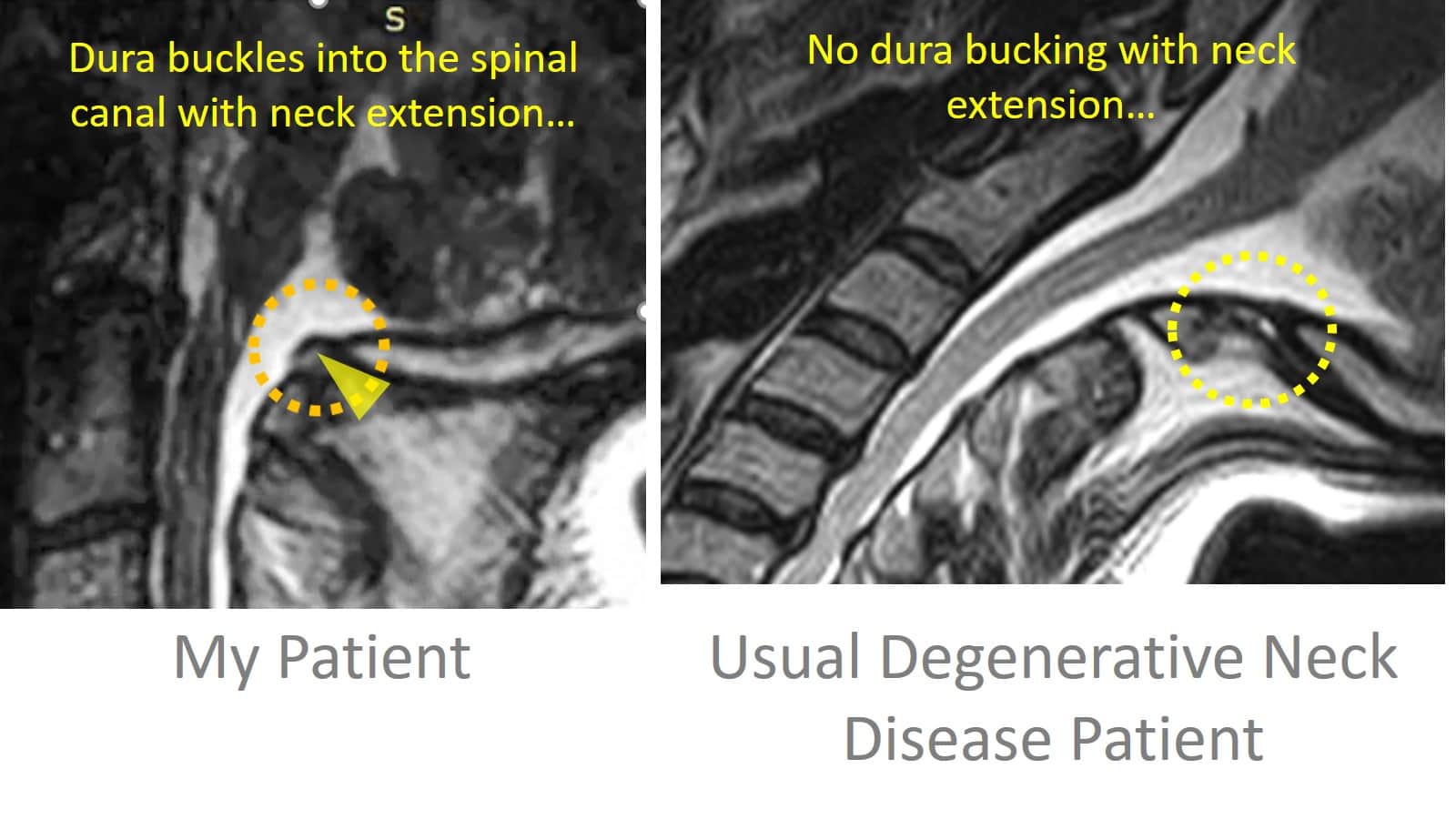
As I mentioned above, upper neck muscle atrophy has been shown, by Elliott and others, to be linked to prolonged pain after traumatic injuries. If you pay close attention to the upper part of the neck in the cine loop above, you’ll see the dura “buckle” into the spinal canal when my patient brings his head back into extension (see adjacent image). This might go unnoticed in a usual MRI that was static (without motion), but it jumps out in the cine loop. Note that the image to the left also shows a patient with common degenerative disc disease of the neck, also in extension, where this doesn’t happen in this area. So let’s explore why this could be happening.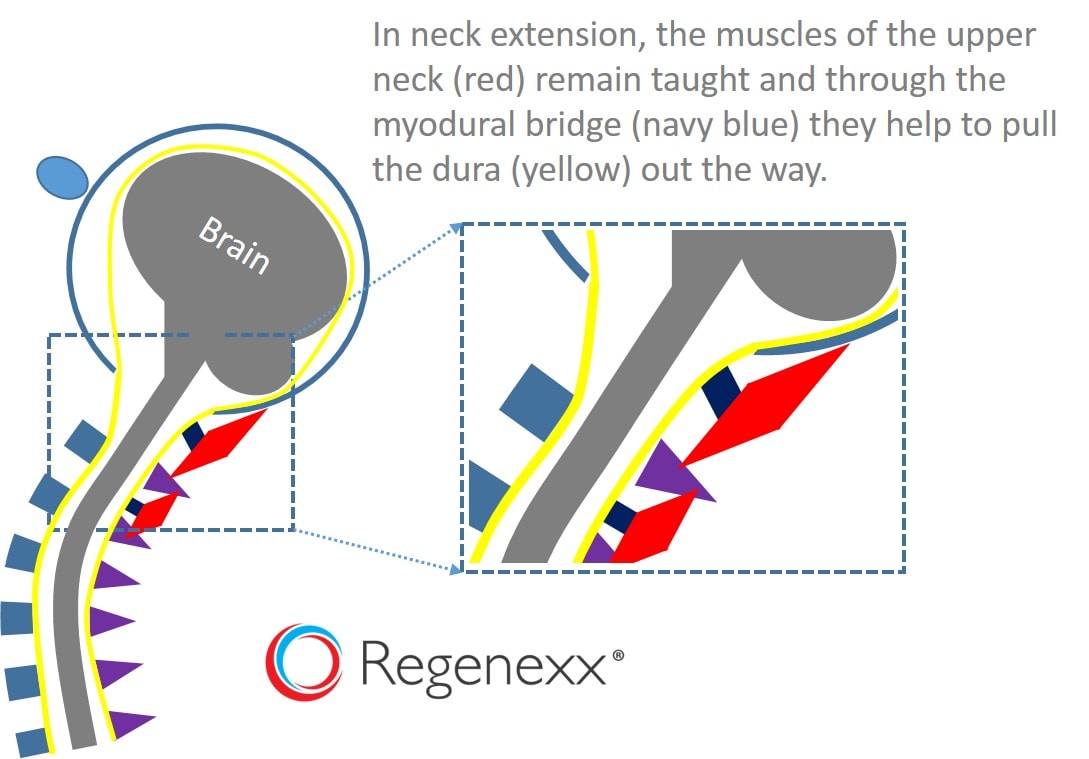
In the image above, I’ve vastly simplified the previous MRI image, showing how thick and healthy neck muscles can keep the dura taught and out of the spinal canal when the neck extends. Again, they do this by gently tugging through the myodural bridge. What would happen if these muscles were atrophied as shown in the research on patients with chronic neck and headache pain after a traumatic injury, like whiplash? Given that some MRI studies of the normal myodural bridge show it pulling in the direction of the muscles (away from the spinal canal), one possibility is that weakened upper neck muscles would allow the dura to bulge into the spinal canal. 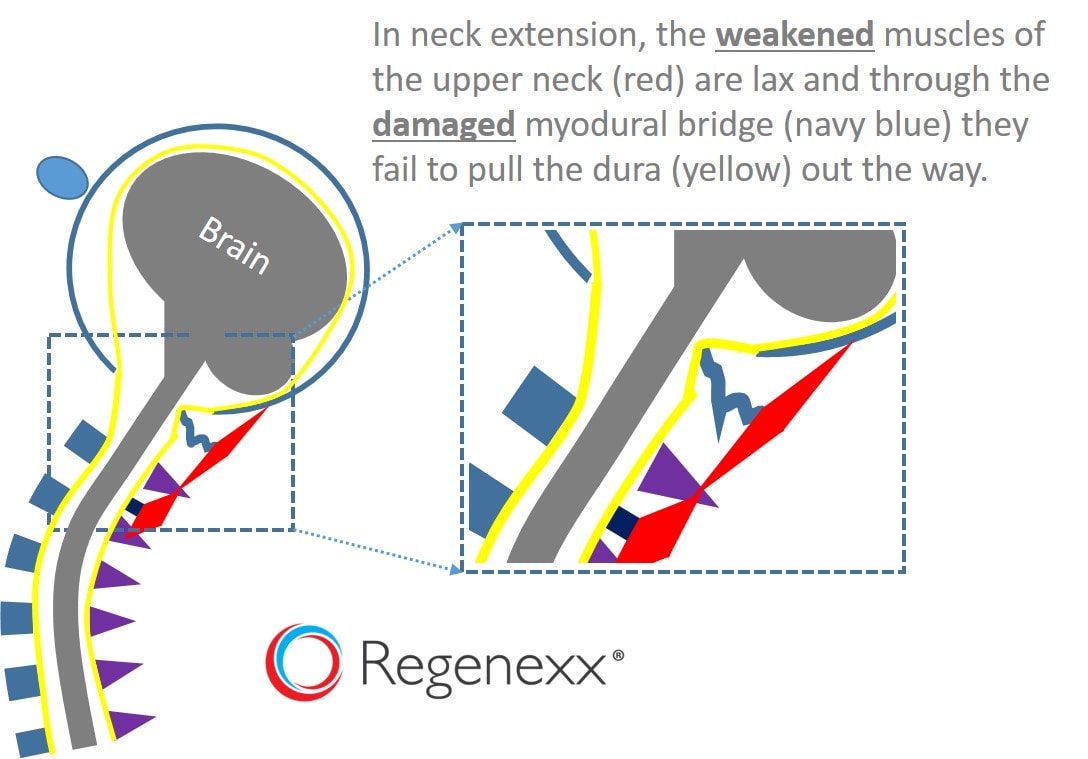
Above, I’ve illustrated what happens when my patient extends his neck. This shows that either a weakened myodural bridge or weak and atrophied upper neck muscles could allow the dura to bulge into the spinal canal. So is this causing my patient’s headaches? It’s likely not the lone cause as he has other CCJ injuries, such as loose and/or ruptured ligaments. However, it does bring up an interesting concept, that perhaps cine MRI loops like the one above, performed with great care, like the way Dr. Rosa does his, could image myodural bridge abnormalities.
The upshot? Your upper neck muscles are jacked into your brain. That’s a pretty sobering thought as it means that the status of these little muscles is pretty important. While there are other known neck headache causes, like upper neck joints and nerves, there’s just something paradigm shifting about the myodural bridge. In addition, we’re getting closer to imaging these issues every day. While MRI isn’t the “end all be all” of cinching a diagnosis, it’s certainly helpful for physicians and patients to see where the problem that’s been causing severe headaches for years is located and what may be happening.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.