Orthopedic Academic Medical Centers Ignore Meniscectomy Research as Well
We’ve all been taught to believe that academic medical centers use the latest research to guide their treatment decisions. While that may be the case in other fields of medicine, it’s usually not the case in Orthopedics. This morning I’d like to demonstrate how one academic medical center, the Cleveland Clinic, has apparently been ignoring the high-level research showing that routine meniscectomy doesn’t help patients. Let me explain.
What Is Meniscectomy?
The meniscus is an added layer of protection for the cartilage in the knee. Tears in the meniscus don’t automatically equate to knee pain. I’ve shared before that just like we develop wrinkles as we age, we can also develop meniscus tears, so the truth is, even if you do have knee pain, you could have had meniscus tears long before you started having knee pain. In other words, your knee pain may not be due to the wear-and-tear meniscus tears that are a normal part of aging. Just because an MRI shows a meniscus tear, it doesn’t mean you need to have it “fixed,” no more so than you’d have to “fix” a wrinkle.
A meniscectomy isn’t just a repair as most patients seem to think. More than 90% of the time, the torn piece of the meniscus is being excised or removed. While a torn meniscus might not sound right, it’s usually more efficient at protecting the cartilage than a meniscus that’s missing a piece altogether. For example, studies have shown that meniscectomy can increase the load on the cartilage, which will lead to further wear and tear and, no doubt, chronic pain.
The Research Showing Meniscectomy Doesn’t Work
I’ve covered many studies over the years showing meniscectomy doesn’t work. A handful follows:
- Meniscectomy is no better than a fake, or placebo, surgery.
- Physical therapy is as good as meniscectomy.
- A large number of meniscectomy patients are dissatisfied with their results.
The Cleveland Clinic Meniscectomy Data
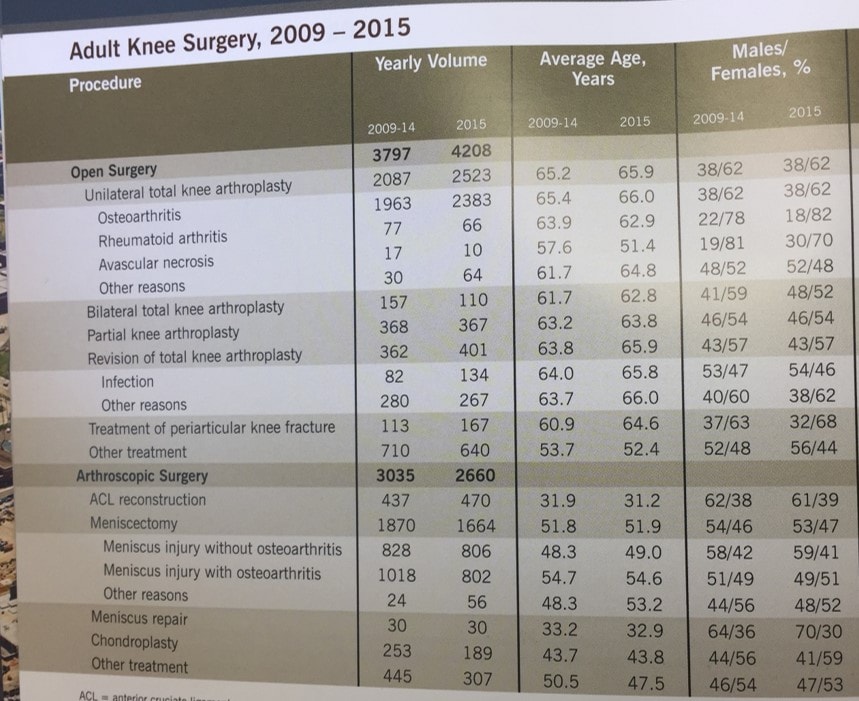
Academic medical centers frequently send flyers out to physicians in private practice to show their expertise in hopes of generating referrals for complex cases. This practice makes sense as these centers often pioneer new therapies that may not be available in smaller cities. One such marketing piece recently sent out by the Cleveland Clinic is shown above.
What you see is the orthopedic surgical rates by category. What sticks out like an unscientific sore thumb is what you don’t see. If you look at the line that shows the number of meniscectomy surgeries, given the research showing how ineffective this procedure is for patients, the 2009–2014 totals should be far more than the 2015 total. That would reflect that this academic medical center has begun to adjust its practices to reflect the research, which would mean that they are performing fewer meniscectomy procedures. So let’s delve into what’s there versus the published research.
In 2012, the prestigious New England Journal of Medicine published a paper that showed that meniscectomy for patients with knee arthritis was no better than physical therapy. Let’s look to see if the Cleveland Clinic changed its practices to conform with this high-level research. From 2009–2014, this surgery was performed in 34% of all arthroscopic surgery patients with a meniscus tear and arthritis. In 2015, it was performed in 48% of patients! So the response to the research seems to have been an increase in the surgery rates? Yikes, that’s the opposite of what should be happening if this medical center was using the evidence to guide its operations.
In 2013, the same journal published a randomized controlled trial comparing fake surgery to meniscectomy for patients who were 35–65 years of age without arthritis and who had a degenerative meniscus tear. The meniscus surgery couldn’t beat the fake procedure. So we should expect to see some decline in meniscectomy rates for patients without arthritis in these Cleveland Clinic stats. This is especially true given that their patients in this category were older (on average 48.3–49 years old) and similar in age to the patients in the study (52 years). From 2009–2014, this category made up 28% of all arthroscopies. In 2015, these surgeries accounted for 30%! Again, the opposite of what you would expect to see if this academic practice was using the level-1 evidence to guide its surgical decision-making.
It’s not hard to see from this data that the Cleveland Clinic is not following the evidence when it comes to meniscectomy. If they were, two- and three-year-old studies would be reducing the rate of this ineffective surgery. While many surgeons argue that while these procedures may not work when groups are compared some individual patients may still need the procedure, if this academic institution were following that guideline we would expect to see the rates of meniscectomy with and without arthritis go significantly down, not up.
The upshot? If academic medical centers refuse to change their practices when research shows that a particular surgery is ineffective in most patients, how can we expect the rank-and-file private-practice orthopedic surgeons to alter what they do? We can’t. Bottom line, I’m not sure there’s any way to interpret this data other than that the Cleveland Clinic Orthopedic Surgery department is ignoring the research, which is not a good thing.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
