What You Should Know About SI Joint Dysfunction

Medically Reviewed By:
Pain in the lower back, hips, or pelvis can have many possible sources, and one of the most overlooked is the sacroiliac (SI) joint. These small joints connect the spine to the pelvis. They help absorb impact and maintain balance during everyday movement. When the SI joints become irritated or move abnormally, they can contribute to persistent pain and stiffness that disrupt daily activities and overall quality of life.
SI joint dysfunction is more common than many realize, yet it is often mistaken for other spinal or hip problems because the symptoms are similar. Understanding how the SI joints work and how their mechanics influence surrounding structures is key to identifying the cause of pain.
Physicians in the licensed Regenexx network specialize in diagnosing and treating joint-related pain using image-guided, non-surgical procedures that support the body’s natural healing processes. By focusing on the underlying tissue and biomechanical imbalances, procedures using Regenexx injectates may help improve comfort and support more confident movement over time.
Understanding Sacroiliac Joint Dysfunction
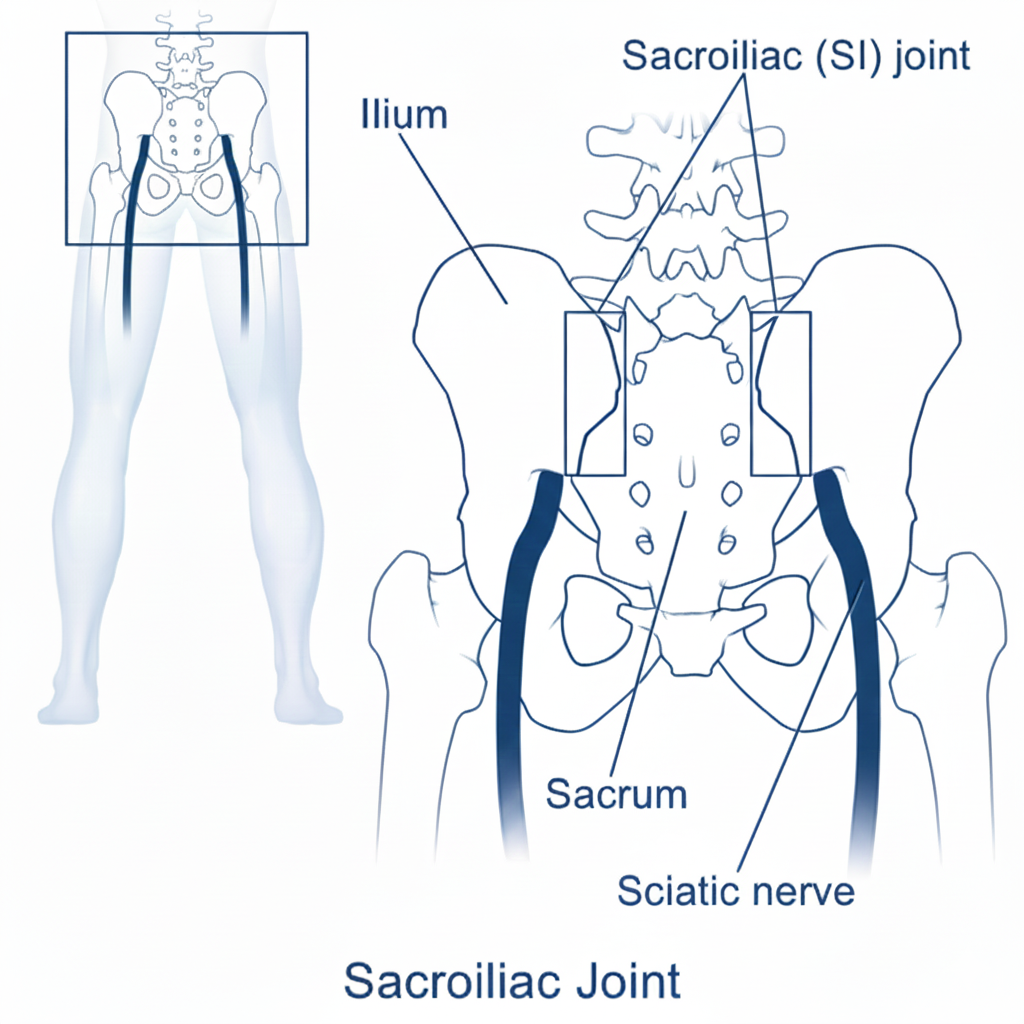
The sacroiliac joints connect the sacrum, the triangular bone at the base of the spine, to the iliac bones on either side of the pelvis. SI joint dysfunction occurs when one or both joints become irritated, restricted in movement, or overly mobile. These changes may disrupt normal biomechanics and contribute to mechanical stress in surrounding structures.
Factors that may contribute to SI joint dysfunction include trauma, pregnancy-related ligament laxity, altered gait or posture, and structural imbalances. In some individuals, previous lumbar fusion surgery may place additional strain on the SI joints, increasing the likelihood of dysfunction.
Diagnosing SI joint dysfunction can be challenging, as symptoms can resemble those of other spinal or pelvic conditions. A thorough evaluation includes a combination of physical assessment, imaging studies, and, in some cases, diagnostic injections to help confirm the SI joint as a potential source of discomfort.
The SI Joint And Its Role In Spinal Support
The SI joint forms a crucial connection between the spine and the pelvis. Each person has two SI joints, one on either side of the sacrum, that link the sacrum to the iliac bones. These joints are designed primarily for stability rather than mobility and play a key role in supporting body weight.
Although the SI joints allow only minimal movement, they help absorb shock and distribute forces generated during daily activities. Movements such as walking, bending, transitioning from sitting to standing, and lifting rely on proper SI joint function to support efficient load transfer between the upper and lower body.
When the SI joints do not move in coordination with the spine and pelvis, mechanical stress may increase, placing strain on surrounding ligaments, muscles, and adjacent joints. This imbalance can contribute to altered movement patterns and may lead to compensatory issues in the lower back, hips, or legs.
What May Cause Dysfunction In The SI Joints
SI joint dysfunction may result from biomechanical changes, repetitive stress, or structural imbalances involving the spine or pelvis. In many cases, the joint becomes either restricted or excessively mobile, which may interfere with efficient load transfer between the upper and lower body.
Contributing factors may include:
Trauma Or Injury
Trauma to the pelvis or lower back—such as from a fall, sports impact, or vehicle accident—may affect the stability of the SI joints. Even when injuries seem minor, forceful impact may stretch or irritate the supporting ligaments, potentially leading to abnormal joint movement over time. In some cases, SI joint dysfunction may not appear immediately.
Symptoms can develop gradually as the body adapts or compensates for the original injury. These changes may contribute to ongoing discomfort and altered movement patterns without thorough evaluation and stabilization.
Pregnancy And Childbirth
Hormonal changes during pregnancy, particularly increased relaxin levels, loosen pelvic ligaments to prepare for childbirth. This can increase SI joint mobility and susceptibility to mechanical stress. Studies estimate that 20% to 30% of pregnant individuals in the U.S. experience clinically significant pelvic girdle pain, while up to 50% report some form of lower back or pelvic discomfort during pregnancy.
As body weight and posture change, additional strain may be placed on the SI joints. Although symptoms often improve after delivery, about 8% to 10% experience persistent postpartum pai, which may be linked to ongoing SI joint instability or altered biomechanics.
Repetitive Stress Or Overuse
Repeated activities that place uneven or excessive stress on the pelvis may contribute to SI joint dysfunction over time. This can include long-distance running, frequent lifting or bending, or working on uneven surfaces.
Ongoing overuse may affect the ligaments that support the joint or lead to minor misalignment—especially when body mechanics are not optimal. As the joints’ ability to stabilize diminishes, surrounding muscles and tissues may become irritated, potentially resulting in persistent discomfort.
Poor Posture And Mechanics
Inefficient posture or movement patterns may gradually place added strain on the SI joints. Prolonged sitting with a tilted pelvis, uneven weight distribution while standing, or lifting without proper form can alter how forces move through the lower back and pelvis.
When posture or mechanics consistently shift load away from larger muscle groups, the SI joints and surrounding ligaments may begin to compensate. Over time, this compensation can reduce joint stability and contribute to irritation or discomfort.
Underlying Medical Conditions
Certain medical conditions may directly affect the SI joints or alter nearby structures in ways that contribute to dysfunction. These conditions may promote inflammation, joint degeneration, or mechanical changes that impact stability and function:
- Osteoarthritis: Wear and tear in the SI joints may lead to cartilage loss, joint space narrowing, or bony changes that reduce motion and cause irritation.
- Ankylosing spondylitis: This inflammatory condition may affect the SI joints early, contributing to chronic inflammation, stiffness, and—in some cases— joint fusion.
- Degenerative joint disease: Age-related changes in nearby joints, such as the lumbar spine or hips, may shift stress to the SI joints and increase dysfunction risk.
Recognizing The Signs And Symptoms
SI joint dysfunction may cause symptoms that resemble those of other spine or hip-related conditions, which can make identifying the source of symptoms more complex. Understanding the typical patterns of SI joint-related symptoms may help guide a more accurate evaluation and inform treatment planning.
Some of the more commonly reported symptoms include:
- Stiffness or reduced range of motion: Individuals may notice restricted movement in the lower back, hips, or pelvis—particularly after prolonged sitting or inactivity.
- Discomfort with prolonged positions or repetitive movements: Pain may gradually increase during extended periods of standing, walking, or sitting. Individuals may experience temporary relief with position changes or gentle movement.
- Tenderness around the SI joint area: Gentle pressure near the base of the spine or upper buttocks may trigger a dull ache or localized sensitivity.
- Back Pain When Getting Up From A Chair: Pain when rising from a seated position may be due to muscle stiffness, joint degeneration, or spinal issues. It can cause discomfort in the lower back, often easing with movement but recurring with prolonged sitting. Read More About Back Pain When Getting Up From A Chair.
How Symptoms Are Diagnosed
A structured diagnostic process is often needed to help identify SI joint dysfunction and distinguish it from other conditions with similar symptoms. Key diagnostic steps may include:
- Medical history and physical examination: This includes reviews of previous injuries, activity levels, and symptom patterns, and a hands-on assessment for tenderness, joint alignment, and movement restrictions near the SI joint.
- Provocative tests: Targeted maneuvers, such as FABER (flexion, abduction, and external rotation) or Gaenslen’s tests, are used to apply stress to the joint and evaluate whether symptoms can be reproduced.
- Imaging studies: X-rays, MRI, or CT scans may help detect fractures, joint changes, or nearby structural issues. SI joint dysfunction may not appear clearly on imaging.
- Diagnostic injection: A physician may inject a small amount of anesthetic into the SI joint under imaging guidance. Temporary relief may indicate the joint as a symptom source.
Conventional Treatment Options
Conservative care for SI joint dysfunction often focuses on improving stability, reducing joint stress, and promoting more efficient movement patterns. Common approaches may include:
- Physical therapy: Customized exercises target muscle imbalances, improve joint mobility, and strengthen core and pelvic support to reduce stress on the SI joints.
- SI joint belts or braces: These supportive devices may help stabilize the pelvis and limit excessive joint motion during standing, walking, or lifting.
- Heat or ice therapy: Heat may help ease muscle tightness, while cold can temporarily reduce inflammation and discomfort in the affected joint region.
- Radiofrequency ablation: This procedure applies heat to specific nerves near the SI joint to reduce pain signals for an extended period.
- Acupuncture or chiropractic care: Some individuals explore these options to manage muscle tension, improve alignment, or relieve symptoms associated with joint dysfunction.
- SI Joint Fusion: Sacroiliac (SI) joint fusion is a surgical procedure that stabilizes the SI joint by fusing the sacrum and ilium. It may be considered for chronic SI joint pain that has not responded to other treatments. Read More About SI Joint Fusion.
Regenexx’s Approach To SI Joint Recovery
Conventional treatment for SI joint dysfunction may include high-dose steroid injections or surgical fusion. While these methods are common, each carries potential limitations. Steroid injections may affect tissue quality over time, and SI joint fusion eliminates joint motion, removing a natural shock absorber between the spine and pelvis.
Studies have shown potential concerns with these approaches:
- One five-year study reported that 16.5% of individuals who underwent lower back fusion required additional surgery due to complications.
- After ten years, nearly one-third of fusion patients required revision surgery.
- Another study found that 55% of individuals continued using narcotic medications two years after SI joint fusion.
Procedures using Regenexx lab processes offer a less invasive alternative that may support joint function without removing structural movement. These outpatient procedures use imaging guidance to deliver customized concentrations of healing agents derived from a patient’s own bone marrow or blood into areas by the SI joint showing signs of tissue damage.
This approach is designed to support the body’s natural healing response and may help improve joint movement and comfort by targeting the tissues that support the joint.
Many individuals are able to resume daily routines relatively soon after treatment, depending on their diagnosis and overall health.
Physicians in the licensed Regenexx network focus on improving joint support, rather than removing structure or suppressing symptoms, to help address the underlying contributors to dysfunction.
Take The Next Step Toward Better Joint Health
When left unaddressed, SI joint dysfunction may contribute to ongoing pain and restricted movement. Early evaluation and a focused care plan may help support joint function and reduce strain on surrounding tissues. While conventional treatments may offer temporary relief, they can involve risks such as tissue breakdown or reduced joint stability over time.
Procedures using Regenexx lab processes offer a less invasive alternative for individuals seeking to avoid long-term medication use or surgical fusion. This approach is designed to help support joint mechanics, improve tissue quality, and reduce biomechanical strain.
A thorough evaluation by a physician in the licensed Regenexx network can help determine a personalized plan to support long-term joint health and function.
Find out if you are a candidate for the Regenexx approach. Schedule a consultation with a physician in the licensed Regenexx network today.

Medically Reviewed By:
